Telemedicine in French Memory Clinics During the COVID-19 Pandemic
Abstract
This multicenter study was conducted in French memory clinics during the first COVID-2019 lockdown (March–May 2020). The objective was to evaluate the effect of a telemedicine consultation on treatment modification in dementia care. Among 874 patients who had a telemedicine consultation, 103 (10.7%) had treatment modifications, in particular those living with a relative or diagnosed with Alzheimer’s disease. A control group of patients referred March–May 2019 was also included. Treatment modification rate was similar between periods with an adjusted percentage difference of –4% (p = 0.27). Telemedicine consultations allowed treatment modifications with only a minor short-term negative impact on therapeutic strategies.
INTRODUCTION
On March 17, 2020, the coronavirus disease 2019 (COVID-19) pandemic led the French government to establish a first national lockdown until May 11, 2020. In most memory clinics, all face-to-face medical visits were canceled to ensure social distancing and prioritize university hospital activities for the management of patients with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1, 2].
In order to continue providing care, many physicians switched to telemedicine consultations as an alternative to face-to-face visits [3, 4].
At that time, literature was quite scarce with no clear statement concerning patients and their management in an unprecedented situation [5, 6]. Due to lockdown conditions, some patients with dementia had to move to a relative’s home, while others were isolated in their own residence. Moreover, there was a substantial decrease of home visits by professional caregivers. As patients living with dementia are not inclined to change their daily routines, neuropsychiatric symptoms might have increased during that period [7–10], with a higher prevalence of hallucinations [11] and depression [12] in elderly with dementia. Facing that new context with no possibility to perform clinical examination, we hypothesized that physicians might have modified their therapeutic strategies regarding psychoactive drugs.
To better describe the use of telemedicine consultations in clinical practice, we conducted a retrospective study including patients from seven memory clinics in France. The objective of the study was to evaluate the effect of a telemedicine consultation on treatment modification during the first period of lockdown in France and to detect any changes in physicians’ prescribing habits. First, we evaluated treatment modifications in seven French centers, then we analyzed determinants, and finally, in the Rouen center only, we compared treatment modifications in 2020 to those in the same period in 2019, including patients from 2020 who had their visit postponed to avoid any selection bias.
METHODS
French telemedicine group
Between March 17 and May 11, 2020 (first lockdown period in France), all patients who had a telemedicine consultation, by phone or webcam, in one of seven memory clinics of the French network of memory clinics were included. These memory clinics are located in the university hospital centers of Amiens, Caen, Lille, Marseille, Paris Sainte-Anne, Paris Lariboisière-Fernand Widal, and Rouen. Among these patients, a subgroup analysis was performed in patients from Rouen center, for complementary comparisons.
All telemedicine consultations were follow-up visits, as telemedicine was, at that time, considered not appropriate for new patients. New patients were postponed to a later onsite visit after lockdown and not included in the study.
Demographic and clinical data were retrospectively collected from medical reports: age, sex, consultation context (scheduled/unscheduled consultation), behavioral/cognitive condition (stable, improved, or worsened based on the physician’s subjective perception), lockdown living conditions (individual house/flat, nursing home, alone/with a relative) current diagnosis reported by the physician (Alzheimer’s disease (AD), frontotemporal lobar degeneration (FTLD), Lewy body disease (LBD), vascular/toxicity (VT), psychiatric condition (Psy), pending diagnoses, other), any drug modification (introduction, interruption, no modification, increase, decrease) regarding four types of drugs (acetylcholinesterase inhibitors, antipsychotics, benzodiazepines, mood stabilizers). All drugs were prescribed during the telemedicine consultation, and prescriptions were sent using online services or postal services.
Patients from Rouen center
Between March 17 and May 11, 2020, patients from Rouen center were included in two groups:
– Rouen telemedicine subgroup: patients who had a telemedicine consultation; these patients were part of the French telemedicine group.
– Rouen non-telemedicine control group: patients who did not have a telemedicine consultation but who had been scheduled to have a consultation during lockdown; these patients were contacted by telephone to ensure that they did not need to contact their physician for any concern, preferring to postpone their scheduled visit to a later date, on-site, after lockdown. For these patients, drug prescriptions were considered maintained.
Rouen control group
A control group of patients referred to Rouen center between March 17 and May 11, 2019 was also included, in order to compare drug prescribing between the two periods, before lockdown and during lockdown. All the patients had an on-site visit as there was no telemedicine device in Rouen memory clinic at that time. To be fully comparable, we also excluded new patients, as our study concerns treatment modification in follow-up patients.
The ethical approval for the study design, data collection, and publication was obtained from the institutional review board of Rouen University Hospital for retrospective non-interventional research.
Statistical analysis
Qualitative variables and quantitative variables were described with, respectively, percentage and mean (with standard deviation).
In order to study risk factors for treatment modification, an adjusted difference percentage was calculated based on a multiple linear mixed-effect model. The primary outcome was drug modification (introduction, modification, or interruption of acetylcholinesterase inhibitors, antipsychotics, benzodiazepines, mood stabilizers). The secondary outcome was sedative drug increase (any increase in the prescription of antipsychotics and benzodiazepines).
Potential risk factors were: number of weeks of lockdown, diagnoses, living conditions, housing, scheduled/unscheduled visit. Center was added to the model as random effect.
In order to study the impact of lockdown on therapeutic strategies in Rouen between the two periods 2019 and 2020, we computed a multiple linear regression. The exposure variable was ‘year of the consultation’, and an adjustment covariate ‘diagnosis’. Confidence intervals at 95% were computed based on 5000 bootstrap repetitions with bias-corrected accelerated method. Patients with missing data on any variable were excluded in the modeling process. The same model was computed after including patients from the Rouen non-telemedicine group and with a different outcome defined as increase or introduction of sedative drugs.
RESULTS
The French telemedicine group included 874 patients; 73 in the Rouen telemedicine subgroup. The Rouen non-telemedicine control group included 86 patients (corresponding to patients whose scheduled visits had been postponed during lockdown to a further date). Lastly, the Rouen control group included 190 patients with follow-up visit in the Rouen memory clinic between March 17 and May 11, 2019. Thirty patients were excluded from the model-analysis due to missing data. Patients’ demographic characteristics are presented in Table 1.
Table 1
Demographical characteristics of patients from COVID-19 cohort (whole cohort and Rouen only cohort) and 2019 control cohort
| French tele-medicine group | Rouen tele-medicine subgroup | Rouen non-telemedicine control group | Rouen control group | |
| Patients (n) | 874 | 73 | 86 | 190 |
| Age | 71.2 (±11.7) | 70.8 (±10.4) | 70.2 (±12.5) | 67.58 (±12.4) |
| Sex (N female) | 89 (43.4%) | 27 (37%) | 47 (54.7%) | 104 (54.7%) |
| Consultation context [N, (%)] | ||||
| Scheduled consultation | 763 (87.3%) | 67 (91.8%) | NA | NA |
| Unscheduled consultation | 104 (11.9%) | 6 (8.2%) | NA | NA |
| Not determined | 7 (0.8%) | 0 (0%) | NA | NA |
| Behavioral symptoms or cognitive course [N, (%)] | ||||
| Improved | 32 (3.7%) | 3 (4.1%) | 0 (0%) | NA |
| Stable | 541 (62.1%) | 28 (38.4%) | 86 (100%) | NA |
| Worsened | 298 (34.2%) | 42 (57.5%) | 0 (0%) | NA |
| Lockdown living conditions [N, (%)] | ||||
| Alone in a flat | 140 (16.2%) | 6 (8.2%) | 8 (9.3%) | NA |
| Alone in a house | 44 (5.1%) | 5 (6.8%) | 11 (12.8%) | NA |
| In a nursing home | 38 (4.4%) | 5 (6.8%) | 9 (10.5%) | NA |
| With a relative in a flat | 304 (35.1%) | 6 (8.2%) | 13 (15.1%) | NA |
| With a relative in a house | 339 (39.2%) | 51 (69.9%) | 45 (52.3%) | NA |
| Diagnosis [N, (%)] | ||||
| Alzheimer’s disease | 369 (43.2%) | 31 (44.3%) | 35 (41.2%) | 69 (36.5%) |
| Frontotemporal lobar degeneration | 59 (6.9%) | 8 (11.4%) | 6 (7.1%) | 16 (8.5%) |
| Lewy body disease | 62 (7.3%) | 8 (11.4%) | 7 (8.2%) | 3 (1.6%) |
| Other | 28 (3.3%) | 1 (1.4%) | 5 (5.9%) | 12 (6.3%) |
| Psychiatric disorder | 3 (0.4%) | 1 (1.4%) | 10 (11.8%) | 12 (6.3%) |
| Undetermined | 268 (31.4%) | 20 (28.6%) | 16 (18.8%) | 64 (33.9%) |
| Vascular or toxic dementia | 65 (7.6%) | 1 (1.4%) | 6 (7.1%) | 13 (6.9%) |
Within the French telemedicine group, 57.4% of patients presented with neurodegenerative disease and the most frequent diagnosis was AD (43.2%), with a similar rate to the Rouen non-telemedicine group (41.2%, p = 0.82). Most patients were in lockdown with a relative, in a house (39.2%) or in a flat (35.1%). Drug prescribing was relatively stable during that period and only 11.8% of patients had a change in their treatment (Table 2).
Table 2
Drug prescription characteristics in patients from Covid-19 cohort (whole cohort and Rouen only cohort) and 2019 control cohort
| French tele-medicine group Nb. (%) | Rouen tele-medicine subgroup Nb. (%) | Rouen control group Nb. (%) | |
| Acetylcholinesterase inhibitor | |||
| Interruption | 6 (0.7%) | 0 (0%) | 1 (0.5%) |
| Increase | 5 (0.6%) | 1 (0.6%) | 3 (1.6%) |
| Decrease | 2 (0.2%) | 0 (0%) | 0 (0%) |
| Start | 30 (3.4%) | 3 (1.9%) | 2 (1.1%) |
| No change | 831 (95.1%) | 69 (97.5%) | 184 (96.8%) |
| Antipsychotics | |||
| Interruption | 5 (0.6%) | 0 (0%) | 1 (0.5%) |
| Increase | 2 (0.2%) | 3 (4.1%) | 0 (0%) |
| Decrease | 6 (0.7%) | 2 (2.7%) | 3 (1.6%) |
| Start | 11 (1.3%) | 0 (0%) | 2 (1.1%) |
| No change | 850 (97.3%) | 68 (93.2%) | 184 (96.8%) |
| Benzodiazepines | |||
| Interruption | 2 (0.2%) | 0 (0%) | 0 (0%) |
| Increase | 8 (0.9%) | 2 (2.7%) | 2 (1.1%) |
| Decrease | 1 (0.1%) | 1 (1.4%) | 3 (1.6%) |
| Start | 28 (3.2%) | 7 (9.6%) | 0 (0%) |
| No change | 835 (95.5%) | 63 (86.3%) | 185 (97.4%) |
| Mood stabilizers | |||
| Interruption | 6 (0.7%) | 4 (5.5%) | 1 (0.5%) |
| Increase | 1 (0.1%) | 1 (1.4%) | 3 (1.6%) |
| Decrease | 8 (0.9%) | 3 (4.1%) | 3 (1.6%) |
| Start | 0 (0%) | 0 (0%) | 4 (2.1%) |
| No change | 859 (98.3%) | 65 (89%) | 179 (94.2%) |
| Treatment modification | 103 (11.8%) | 18 (24.6%) | 25 (13.2%) |
| Sedative drug increase | 45 (51.5%) | 9 (12.3%) | 4 (2.1%) |
However, a treatment modification was more frequent among patients living with a relative than those living alone (+6.8% CI95 %[2.0; 11.3] p = 0.01) and more frequent among AD patients compared to all other etiologies (+9.8% (CI95 %[5; 14.5] p < 0.001). Results from the mixt model evaluating the impact of prescription (drug modification) depending on predictive variables are summarized in the Supplementary Material.
Regarding patients from Rouen center, when comparing the lockdown period in 2020, and the control period in 2019, treatment modifications were observed in 18 patients out of 73 (24.6%) and 25 patients out of 190 (13.2%) respectively, with an adjusted percentage difference of treatment modification of+9.5% (CI95 % [–2.2; 22.5]; p = 0.11). After adding the Rouen non-telemedicine group in the model, the adjusted percentage difference was –3.6% (CI95 % [–10.8; 4.0]; p = 0.36).
A sedative drug increase was observed in 9 patients (12.3%) in the 2020 period compared to 4 patients in 2019 (2.1%) with an adjusted percentage of+10.8% (CI95% [3.65; 20.8] p = 0.001) and+3.3% (CI95% [–0.7; 8.1] p = 0.11) after adding the no-telemedicine cohort in the model.
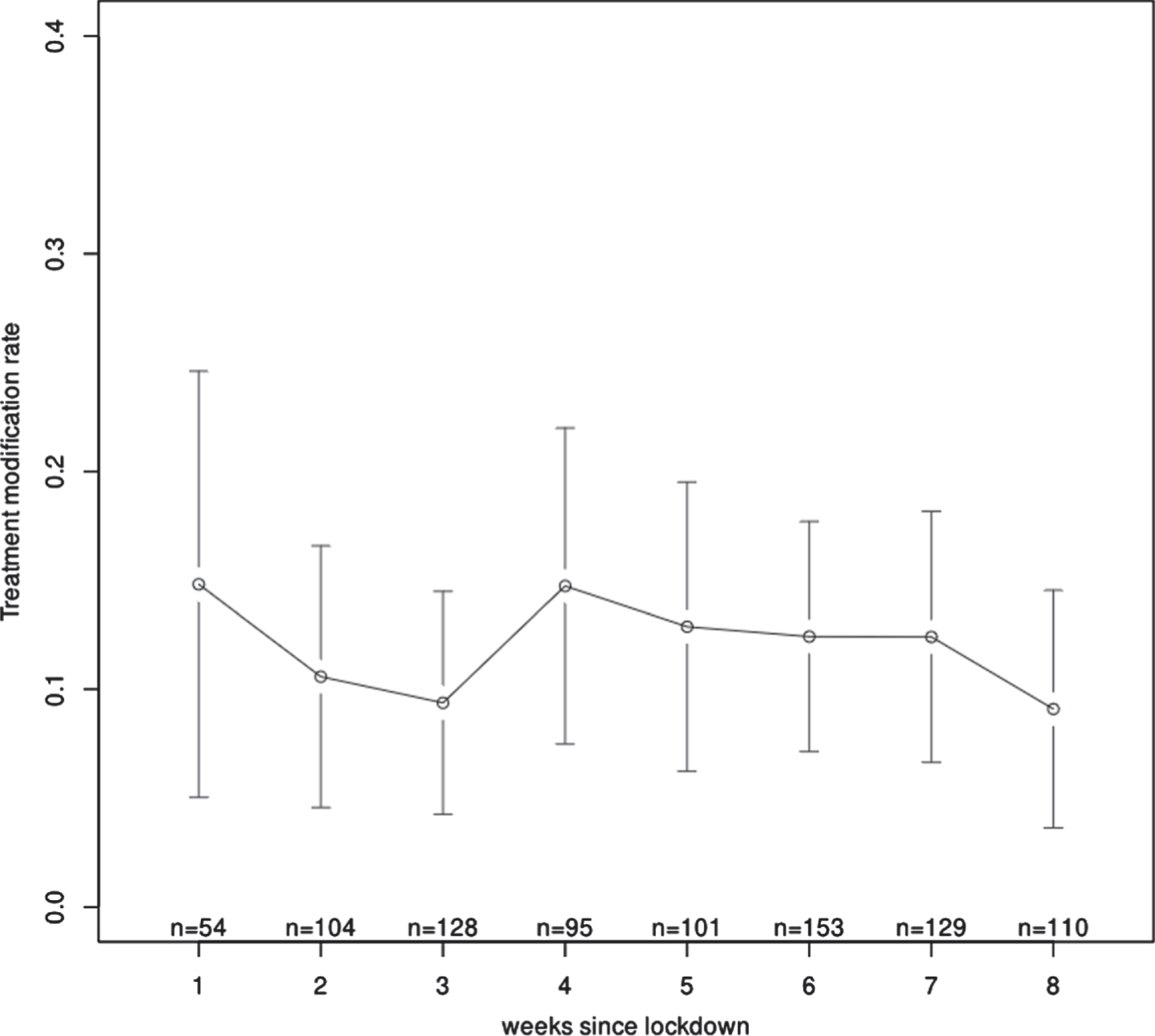
During the lockdown period in 2020, drug prescriptions were relatively stable over time and there was no more than a 4.72% change in prescription between weeks (Fig. 1).
Fig. 1
Prescription modifications over time (each plot presenting the amount of treatment modifications during each lockdown week).
DISCUSSION
To better describe the innovative use of telemedicine in cognitive disorders and its relation to psychoactive drug prescribing during the lockdown period, we analyzed treatment modifications among 874 patients who had telemedicine consultations during the first lockdown in France.
First, it is noteworthy that memory clinics were able to adapt their organization to this new pandemic context, and continued to provide care, despite the frailty of their patients.
In France, patients had access to drug prescriptions during the whole lockdown period and these prescriptions were broadly stable over time. Lockdown conditions might have affected those prescriptions as living conditions might have changed (such as moving to a relative’s home), and living with a relative was reported as a risk factor for treatment modification.
In Rouen center, the fact that drug prescriptions were relatively stable throughout the lockdown period, and compared to face-to-face visits, was a major finding. To the best of our knowledge, this result has not yet been reported in that context. Contradictory findings were suggested by a preliminary analysis of the English National Health Service data. In that study, monthly antipsychotic prescription was estimated based on a ratio including patients living with dementia and the total amount of antipsychotics prescribed in patients with dementia during March and April 2020 in England, and the results revealed that antipsychotic prescription had substantially increased during lockdown [13].
Prescribing drugs remotely can be challenging in a field where clinical and neuropsychological evaluation play a key role in decision-making for dementia care. Few tools are available to monitor cognition remotely [14–16]. Even though the use of telemedicine seems to have no effect on global cognition evaluation compared to face-to-face visits, evaluating behavioral symptoms remotely could lead to inappropriate prescription based on misinterpretation of symptoms. Furthermore, as COVID-19 spread, there was a risk of an increased incidence of delirium [17], hallucinations [11], depression [12], and other neuropsychiatric symptoms [7, 10], thus inducing an escalation in psychoactive drug prescription. Those modifications have been mostly described in patients living in retirement homes [11, 12]. In our patients, living with a relative tended to enhance the rate of drug modification, potentially due to an increase in the reporting of neuropsychiatric symptoms.
Besides this potential impact on behavior, the fact that drug prescriptions were relatively stable over time might indicate that patients tolerated lockdown or, that negative consequences might appear later. The relatively short duration of our data collection leaves this question unanswered. Further studies are needed to better explore potential delayed negative consequences of lockdown conditions.
If we look more closely at patients who had a telemedicine consultation, there was a slight tendency to overprescribing in 2020. This result might represent a selection bias, as only patients in need of care had a telemedicine consultation while other patients had their visit postponed. This tendency no longer remained after including the Rouen non-telemedicine control group in the analysis, suggesting that future studies evaluating lockdown impact on prescribing habits should consider both patients who actually had a visit and patients who had a visit scheduled that was then postponed.
This study has potential limitations. Data were collected retrospectively and drug prescription in 2019 and 2020 was only analyzed by center, providing a rather good comparability but with limited extrapolation. Correlations with cognitive measures or neuropsychiatric symptoms could have been of interest; however, no scale was homogeneously performed in all centers for all possible diagnoses. Moreover, no usual scales as the Mini-Mental State Examination or Montreal Cognitive Assessment are feasible or validated for telemedicine consultations.
Telemedicine consultations allowed treatment modifications for patients followed in memory clinics with only a minor short-term negative impact on therapeutic strategies. Overall, telemedicine consultations allowed treatment modifications for patients followed in memory clinics, with only a minor short-term negative impact. This strategy appears relevant to prevent the spread of COVID-19 disease, particularly in these frail and elderly patients at high risk of contracting severe forms of the disease.
ACKNOWLEDGMENTS
The authors are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for her help in editing the manuscript.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/21-5459r1).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-215459.
REFERENCES
[1] | Peretti-Watel P , Seror V , Cortaredona S , Launay O , Raude J , Verger P , Beck F , Legleye S , L’Haridon O , Ward J , Longitudinale E ((2021) ) Attitudes about COVID-19 Lockdown among General Population, France, March 2020. Emerg Infect Dis 27: , 301–303. |
[2] | Di Domenicos L , Pullano G , Sabbatini CE , Boëlle P-Y , Colizza V ((2020) ) Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med 18: , 240. |
[3] | Klein BC , Busis NA ((2020) ) COVID-19 is catalyzing the adoption of teleneurology. Neurology 94: , 903–904. |
[4] | Capra R , Mattioli F ((2020) ) Tele-health in neurology: An indispensable tool in the management of the SARS-CoV-2 epidemic. J Neurol 267: , 1885–1886. |
[5] | Perry G ((2020) ) Alzheimer’s disease patients in the crosshairs of COVID-19. J Alzheimers Dis 76: , 1. |
[6] | Wang H , Li T , Barbarino P , Gauthier S , Brodaty H , Molinuevo JL , Xie H , Sun Y , Yu E , Tang Y , Weidner W , Yu X ((2020) ) Dementia care during COVID-19. Lancet 395: , 1190–1191. |
[7] | Boutoleau-Bretonnière C , Pouclet-Courtemanche H , Gillet A , Bernard A , Deruet AL , Gouraud I , Mazoue A , Lamy E , Rocher L , Kapogiannis D , El Haj M ((2020) ) The effects of confinement on neuropsychiatric symptoms in Alzheimer’s disease during the COVID-19 crisis. J Alzheimers Dis 76: , 41–47. |
[8] | Cagnin A , Di Lorenzo R , Marra C , Bonanni L , Cupidi C , Laganà V , Rubino E , Vacca A , Provero P , Isella V , Vanacore N , Agosta F , Appollonio I , Caffarra P , Pettenuzzo I , Sambati R , Quaranta D , Guglielmi V , Logroscino G , Filippi M , Tedeschi G , Ferrarese C , Rainero I , Bruni AC ; SINdem COVID-19 Study Group ((2020) ) Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry 11: , 578015. |
[9] | Lara B , Carnes A , Dakterzada F , Benitez I , Piñol-Ripoll G ((2020) ) Neuropsychiatric symptoms and quality of life in Spanish patients with Alzheimer’s disease during the COVID-19 lockdown. Eur J Neurol 27: , 1744–1747. |
[10] | Simonetti A , Pais C , Jones M , Cipriani MC , Janiri D , Monti L , Landi F , Bernabei R , Liperoti R , Sani G ((2020) ) Neuropsychiatric symptoms in elderly with dementia during COVID-19 pandemic: Definition, treatment, and future directions. Front Psychiatry 11: , 579842. |
[11] | El Haj M , Larøi F , Gallouj K ((2021) ) Hallucinations and Covid-19: Increased occurrence of hallucinations in patients with Alzheimer’s disease during lockdown. Psychiatr Q 92: , 1531–1539. |
[12] | El Haj M , Moustafa AA , Gallouj K ((2021) ) Higher depression of patients with Alzheimer’s disease during than before the lockdown. J Alzheimers Dis 81: , 1375–1379. |
[13] | Howard R , Burns A , Schneider L ((2020) ) Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol 19: , 892. |
[14] | Brouillette RM , Foil H , Fontenot S , Correro A , Allen R , Martin CK , Bruce-Keller AJ , Keller JN ((2013) ) Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One 8: , e65925. |
[15] | Lancaster C , Koychev I , Blane J , Chinner A , Wolters L , Hinds C ((2020) ) Evaluating the feasibility of frequent cognitive assessment using the Mezurio smartphone app: Observational and interview study in adults with elevated dementia risk. JMIR MHealth UHealth 8: , e16142. |
[16] | Brearly TW , Shura RD , Martindale SL , Lazowski RA , Luxton DD , Shenal BV , Rowland JA ((2017) ) Neuropsychological test administration by videoconference: A systematic review and meta-analysis. Neuropsychol Rev 27: , 174–186. |
[17] | LaHue SC , James TC , Newman JC , Esmaili AM , Ormseth CH , Ely EW ((2020) ) Collaborative delirium prevention in the age of COVID-19. J Am Geriatr Soc 68: , 947–949. |



