Abstract
Purpose
The COVID pandemic has decreased orthopaedic fracture operative intervention and follow-up and increased the use of virtual telemedicine clinics. We assessed the implications of this management on future orthopaedic practice. We also surveyed patient satisfaction of our virtual fracture follow-up clinics.
Method
We prospectively analysed 154 patients during two weeks of ‘lockdown’ assessing their management. We surveyed 100 virtual fracture clinic follow-up patients for satisfaction, time off work and travel.
Results
Forty-nine percent of patients had decisions affected by COVID. Twelve percent of patients were discharged at diagnosis having potentially unstable fractures. These were all upper limb fractures which may go onto mal-union. Twenty-nine percent of patients were discharged who would have normally had clinal or radiological follow-up. No patients had any long-term union follow-up. Virtual telemedicine clinics have been incredibly successful. The average satisfaction was 4.8/5. In only 6% of cases, the clinician felt a further face-to-face evaluation was required. Eighty-nine percent of patients would have chosen virtual follow-up under normal conditions.
Conclusion
Lessons for the future include potentially large numbers of upper limb mal-unions which may be symptomatic. The non-union rate is likely to be the same, but these patients are unknown due to lack of late imaging. Telemedicine certainly has a role in future orthopaedic management as it is well tolerated and efficient and provides economic and environmental benefits to both clinicians and patients.
Similar content being viewed by others
Introduction
The coronavirus pandemic has had huge implications for the whole of the medical profession. Orthopaedics has been affected by the limitation of resources (particularly theatre capacity) and the need to additionally consider patient and clinical safety in terms of virus transmission. Fracture management in the UK has altered with higher rates of conservative management fractures and a reduction in the amount of follow-up, particularly face to face. The BOAST ‘Management of orthopaedic outpatient fracture management during COVID-19’ set up a pragmatic way of managing patients with fractures [1].
The Great Western Hospital in Swindon is a large district general hospital in the UK with 480 inpatient beds. In the orthopaedic department, we have adapted to the coronavirus pandemic through the increase in virtual fracture clinic follow-ups using a combination of video and telephone clinics. We discuss the implications for orthopaedic surgeons in the future based on this treatment. We also address the lessons learnt from virtual fracture and how they may be usefully developed for the future.
COVID-19 outpatient orthopaedic management
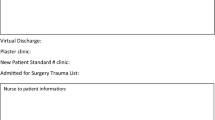
Great Western Hospital was an early adopter of the new patient ‘Virtual Fracture Clinic’ (VFC). There is a large amount of evidence in the literature that virtual fracture clinics are a cost-efficient and cost-effective way of triaging trauma [2,3,4,5]. All new patients are initially reviewed virtually, based on information from emergency departments. They receive a telephone call from the trauma nurse team with advice and their management decision. The changes to this structure since the coronavirus pandemic were merely organisational. Two doctors ran the clinic every day remotely.
Management decisions were based on the British orthopaedic association standards for trauma and orthopaedics (BOAST) guidelines for the management of orthopaedic outpatient management [1]. There was reduced operative capacity due to reduced theatre capacity, primarily due to redeployment of ventilators, time for PPE and decontamination. Patient face-to-face appointments were minimised for patient and staff safety. Removable immobilisation was utilised and no late clinical imaging was undertaken. New virtual follow-up fracture clinics reduced patient face-to-face appointments. Anonymised telephone calls and video calls via Fleming ‘accurx’ system were used.
Virtual fracture clinic analysis
We prospectively analysed the outcomes of virtual fracture clinic patients from the 14th to the 28th of April, during peak lockdown. One hundred fifty-four patients were reviewed. Decisions were classified as ‘normal’ or ‘COVID-related’ decisions. Fifty-one percent of the decisions were as normal and 49% were affected by the coronavirus pandemic. Of those, 19 (12%) patients were brought into hospital, 108 (71%) patients were given a patient-initiated follow-up (PIFU) and 27 (17%) were given a virtual follow-up telemedicine clinic. All the patients brought into hospital were ‘normal’ decisions and all those in the virtual fracture clinic review clinic were ‘COVID’ due to lack of normal face-to-face interaction. The PIFU patients were subdivided into 3 groups: ‘normal’ decisions, ‘COVID’ decisions based on lack of clinical review or follow-up, and ‘COVID’ decisions based on potential mal-unions (see Fig. 1).
Brought into hospital (19 patients, 12%)
Of these patients, five required operative intervention, five had manipulations in clinic, five needed nurse led clinic for wound issues and four needed further clinical review and imaging.
Virtual clinic follow-up (27 patients, 17%)
Of these patients, 15 of them attended the hospital prior to the appointment for an X-ray. Twenty-three patients were then given a PIFU as a result of the appointment, one was brought in for a face-to-face appointment due to clinical need and three were sent for further imaging.
PIFU: COVID lack of follow-up (29 patients, 29%)
These patients were not brought back for any formal review. They lacked further imaging and clinical examination. Most (23 patients) sustained upper limb injuries.
PIFU: Potential mal-union (19 patients, 12%)
These sustained fractures were unstable and could potentially collapse in the future. They were not followed up but could be corrected by a late osteotomy if required. These were all upper limb injuries and the majority of them were in elderly patients. Ten patients had distal radius fractures, five had shoulder injuries, three hand injuries and one sustained an elbow injury.
Implications of COVID managed patients for the future
Nineteen patients had unstable fractures which may lead to symptomatic mal-union. Extrapolating this over 12 weeks of lockdown, with increasing patient numbers, leads to a conservative estimate of over 250 in this group. Mal-union can lead to impaired function and pain [6, 7]. Even if 20% of them went on to symptomatic mal-union requiring surgery, this equates to fifty correctional osteotomies on top of a strained elective upper limb service.
The rate of non-union is unlikely to be affected, but due to the lack of late imaging, we are unable to identify these patients. There should be no increase in surgical intervention, but patients may present later or with more profound complications.
Virtual fracture follow-up clinics through telemedicine
There has been a paradigm shift in the attitude towards telemedicine in the general public. Virtual meetings and working remotely have been widely adopted throughout the public and private sector [8]. Technology has rapidly expanded to enable continuation of services [9].
Telemedicine clinics have advantages and disadvantages compared with face-to-face evaluation, which will always remain the gold standard to clinical evaluation. We will discuss the advantages, the disadvantages and implications for the future.
Advantages
For clinicians, telemedicine provides a wide variety of advantages. They can be done remotely from the hospital, do not require any physical infrastructure such as access to clinic rooms and require less staff namely a receptionist or clinic nurse. They generally involve quicker appointments (although if video conferencing is used in addition, this can take some time to set up). All this leads to increased cost-effectiveness. Clinics can be easily screened by consultants and effective triaging can take place. Training is also easily adapted into clinics. Clinicians can video call each other, share screens and use a continuous ‘chat’ system so communication can occur throughout the consultations. In the current situation, they also decrease potential viral transmission.
For patients, there is also plethora of advantages. The time to appointment is quicker due to increased capacity in clinic. There is no travel time or inconvenience to the patient, including travel and car parking costs. They are particularly helpful to patients who are working as they do not require any time off work. There is a less waiting and time taken out of the patient’s day. There is also a greater degree of flexibility with virtual clinics not being tied to a set rota timetable. If imaging is required, this can be done at the patient’s convenience rather than in pre-designated slots. Environmentally, virtual clinics can save a great deal of travel time, road congestion and petrol consumption.
Disadvantages and limitations
There are some considerable disadvantages to telemedicine. Telephone communication requires a better understanding of English as a spoken language and in some patient groups this is much more challenging than face-to-face conversations. Patients with hearing impairments or those who use lip reading as an adjunct suffer particular communication difficulties. Video conference requires a certain level of technological ability and equipment which may limit certain population groups, especially the elderly. Non-verbal communication, which is extremely important in communication, is totally removed if just the telephone is used. Clinical examination can be adapted for telemedicine, but there are limitations to it. Lack of palpation is inevitable and can lead to significant impairment in clinical ability. Certain examinations including range of movement can be assessed relatively easily and clinical examinations in the extremities, particularly the upper limb, are considerably easier than other assessments. There are also some potential security risks over the telephone with a lack of the person being identified. Issues such as coercion particularly in child protection issues and vulnerable adults are much harder to identify which is a huge concern. Even in a video call, there is no knowing who is behind the camera. A face-to-face assessment of a patient will always provide a wider picture of the whole situation.
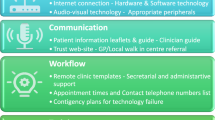
Pre-requisites for a successful virtual clinic
In order for a virtual clinic to be successful, there has to be fluid communication and transition between virtual and face-to-face assessment. Patients who have been assessed virtually and require face-to-face clinical assessment need quick access to appointments in order not to be disadvantaged. Ideally, this needs to be across a wide variety of subspecialists to allow the best assessment and management options. There also needs to be adequate technological infrastructure in order for virtual clinics to work reliably. Contact details, electronic records and dependable remote access are fundamental.
Patient satisfaction
In order to assess the effectiveness of our virtual clinics, we needed to consider not only the clinician and hospital experience but also the patient experience. We asked patients what they thought of virtual clinics. We focussed on patient satisfaction, working status, time off work and travel time. We surveyed patients from the 5th of June to the 16th of July. At the time of their appointment, we asked them where they were, if they worked, if they had taken any time off work for the virtual appointment, how much time they would have taken off work if it had been a hospital appointment, their travel time if they didn’t work and if they would be amenable to a follow-up call. They then received a second phone call some days later from a different member of the orthopaedic team, asking them for a satisfaction score out of five and whether under normal circumstances they would have preferred the appointment in hospital or a virtual clinic appointment.
We have full responses from 100 patients. Twenty-seven patients were contacted by a consultant-level doctor and 73 by two senior registrars (ST7 and ST8). Seventy-five had been discharged from clinic, 11 needed a further face-to-face follow-up, 14 required further virtual assessment and one required an injection. Thirty-six patients were working on the day we phoned, nine were actively employed but not working that day, 12 were off sick due to their injury and 43 of people were not employed. Sixteen people were at work at the time of the call and 84 were at home (a proportion of people worked from home). In the working group, nobody had taken any time off work for a virtual clinic appointment but if it had been a hospital appointment, an average of 161 minutes of working time would have been taken off (range 40–360 minutes). This totalled 93.6 hours of working time for one clinic over six weeks. In the non-working that day group, the travelling time averaged 57 minutes (range 10–240 minutes). This totalled 61.5 hours of travelling time. The average satisfaction score was 4.8/5 (range 4–5). The number of people who under normal circumstances who would have preferred to have been reviewed in a hospital setting was 11 (with 89 people preferring a telephone/video call). Both the satisfaction scores and the preference of appointment were broken down for each clinician and there was no significant difference between the three doctors.
Of the people who would have preferred a hospital appointment, the satisfaction score was 4.4 (range 4–5). There was no significant difference in age of the patients, type of injuries or working status or travel time. Of the 11 patients who were brought back for a face-to-face follow-up, five were due to future appointments to have a cast removed and six were due to the clinician deciding they needed a clinical assessment in hospital (thus a repeat appointment). In five of these six cases, this was due to the clinician deciding they needed a more detailed clinical examination. The remaining patient was brought in due to an English language communication barrier. Interestingly, these patients still had a satisfaction score of 4.7 and only one of these patients (20%) would have preferred their appointment to have been in the hospital initially, which was unexpected.
We have therefore concluded that patients were pleased with our virtual fracture clinic service. There was no particular group that was highlighted as being dissatisfied or where the clinician was unable to effectively assess the patient.
Taking virtual clinics further
Virtual fracture clinics have huge benefits both in terms of cost-effectiveness, flexibility and efficiency of fracture clinic management. Patient satisfaction is high among our population group. The economic impact in terms of time off work and the environmental impact of travel is significant. We hope to make virtual follow-up fracture clinics part of standard orthopaedic practice in the future. Reviews following on call admission or assessment (for instance a limping child or cellulitis) work particularly well as a phone call. Follow-up imaging review such as in suspected scaphoid fractures or post-manipulation cases is significantly more efficient. Immediate post-operative checks can be done with a wound review via video and discussion regarding normal recovery. This can also be translated to an elective service; for instance, long-term follow-up after arthroplasty can easily be done with a pre-arranged X-ray and outcome scores.
Conclusion
COVID-19 has had a profound impact on the outpatient orthopaedic management of fractures, but we have highlighted three particular aspects of potential change.
Our first consideration is to the group of patients who have been discharged with potential mal-unions who may need assessing and a corrective osteotomy in the future. In our hospital, this is likely to be over 250 patients with upper limb fractures. These patients may also have worse outcomes following their fracture. This may well impact the already stretched elective upper limb service after COVID, requiring significant operative time. These patients have been identified and we will report back on these patients after a one year follow-up.
The second group of patients that are yet to be identified is those with any fracture who are developing non-union. The rate of non-union is unlikely to have changed, but these patients have not been followed up, so their presentation may be significantly later than normal.
The third consideration is that virtual clinics were developed out of necessity but have proven to be very successful. Patient satisfaction is high (4.8/5) and the rate of conversion to hospital appointment due to the clinician feeling that inadequate assessment was made was low (6%). The economic advantage to lack of lost working time and the environmental impact on saved journeys was significant. They are now being integrated into our standard fracture pathways.
COVID-19 will have many implications throughout the health sector and to the whole of society. We hope to utilise the learning from the challenges that it has provided to design a more efficient and effective orthopaedic department in the future.
References
Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic (2020) www.boa.ac.uk Version 2 – 21 April 2020
Holgate J, Kirmani S and Anand B (2017) Virtual fracture clinic delivers British Orthopaedic Association compliance. Annals of the Royal College of Surgeons of England, Jan 2017
Logishetty K, Subramanyam S. (2017) Adopting and sustaining a Virtual Fracture Clinic model in the District Hospital setting – a quality improvement approach. BMJ Quality Improvement Reports 2017
McKirdy A, Imbuldeniya AM (2017) The clinical and cost effectiveness of a virtual fracture clinic service: an interrupted time series analysis and before-and-after comparison. Bone Joint Res:2017
Jenkins PJ (2016) Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care. Bone Joint Res:2016
Patton M (2004) Distal radius malunion. J Hand Surg [Am] 2004:4(4)
Katt B, Seigerman D, Lutsky K and Beredjiklian P (2020) Distal radius malunion J Hand Surg [Am] 2020; 45(5)
Doshi A, Platt Y, Dressen J, Mathews B, Siy J (2020) Keep calm and log on: telemedicine for COVID-19 Pandemic Response. J Hosp Med (May 2020)
Webster P (2020) Virtual health care in the era of COVID-19. Lancet 2020(395):10231
Acknowledgements
The authors would like to acknowledge the whole orthopaedic department at the Great Western Hospital in Swindon for their hard work during this busy and challenging period.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dunkerley, S., Thelwall, C., Omiawele, J. et al. Patient care modifications and hospital regulations during the COVID-19 crisis created inequality and functional hazard for patients with orthopaedic trauma. International Orthopaedics (SICOT) 44, 2481–2485 (2020). https://doi.org/10.1007/s00264-020-04764-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04764-x