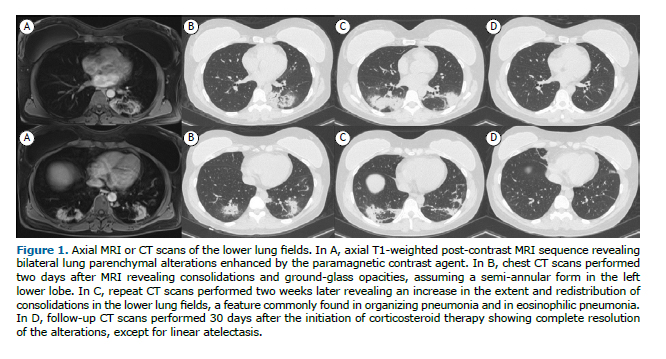
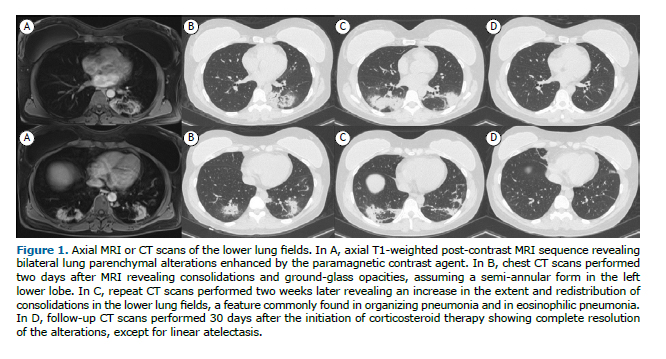
TO THE EDITOR: A 48-year-old woman underwent abdominal MRI for the investigation of a pancreatic cyst. Incidentally, alterations at the lung bases were revealed in the scans (Figure 1A). When specifically asked about symptoms, the patient reported persistent cough and headache for three weeks. She was referred to the ER for further evaluation and to be tested for SARS-CoV-2, showing negative results (RT-PCR and serology). Two days later, she presented with fatigue and fever (38°C) and was hospitalized. A CT of the chest revealed areas of consolidation associated with discrete ground-glass opacities in the lower lobes (Figure 1B), which were interpreted as suspected COVID-19 pneumonia with mild parenchymal extent in the radiological reports. A new round of tests for COVID-19 was performed, showing negative results once again. She was discharged afebrile on antibiotic therapy and was instructed to report for follow-up at the pulmonology outpatient clinic of the institution. Two weeks later, during the clinical evaluation at the outpatient clinic, the patient presented with persistent cough, worsened fatigue, and chills (but no fever). Repeat CT of the chest revealed a small increase in the number of consolidations in the lower lobes (Figure 1C).
Her previous medical history was unremarkable, except for the pancreatic cyst and a diagnosis of depressive disorder (treated with bupropion). She had no history of environmental exposure and was a former smoker (five pack-years; she quit at the age of 27). She reported having used electronic cigarettes in various occasions during the first semester of 2020 (more than 10 times). Her last consumption (together with the use of cannabis) had been one week after the onset of symptoms.
On physical examination, she was breathing normally, showing paroxysmal coughing without expectoration. SpO2 was 96% on room air. Lung auscultation revealed crackles at the lung bases. The remainder of the physical examination was unremarkable. RT-PCR and serology for SARS-CoV-2 were negative again, as were the results for other viral serological tests. Rheumatologic tests were normal. Bronchoscopy showed normal results, followed by BALF collection and transbronchial biopsy at the left posterior lung base. BALF cytology revealed the presence of 20% of eosinophils, whereas examination of the biopsy specimen revealed signs of pneumonia and a great number of eosinophils. Tests for infection in BALF and in the biopsy specimen resulted negative.
Treatment with prednisolone was started (60 mg/day). A follow-up CT performed 30 days later demonstrated complete resolution of the consolidations, and only linear atelectasis remained at the lung bases (Figure 1D). In parallel, the patient, who had already quit the use of e-cigarettes, showed clinical improvement after corticosteroid therapy.
In March of 2020, the WHO declared COVID-19 a pandemic, a reflection of a ruthless disease with a high rate of transmission in an epidemiological context that virtually makes it imperative to discard this diagnosis at the minimum signs of respiratory and systemic symptoms. One of the major diagnostic methods that have been largely employed in this scenario is chest CT. According to the Radiological Society of North America consensus statement
(1) on how to report chest CT findings related to COVID-19, four categories were proposed: typical, indeterminate, atypical, and negative for pneumonia. The objectives of that standardized classification system are to provide guidance and confidence to radiologists and help them communicate clearly with other healthcare providers. In that classification system, typical features are those that are reported in the literature to be frequently and more specifically seen in COVID-19 pneumonia during the current pandemic.
(1) Although CT findings represent an important tool for COVID-19 screening, they can often be limited, even when findings deemed typical are demonstrated. Therefore, various different etiologies are able to induce clinical and radiological findings that are very similar to those in COVID-19 and need to be taken into account as differential diagnoses, including both infectious and noninfectious causes.
E-cigarette, or vaping, product use-associated lung injury (EVALI) is one of such diagnoses. The number of e-cigarettes has been significantly increasing since their introduction in Europe in 2006; about 41 million users were estimated in 2018.
(2) EVALI seems to be a syndrome characterized by respiratory insufficiency and intense inflammatory response. Patients show fever, leukocytosis, and increased CRP levels, as well as negative viral and bacterial tests. Patients commonly demonstrate an inflammatory phenotype with high concentrations of at least two markers (CRP, ESR, leukocytosis, and procalcitonin).
(3) Different products work as vaporizers, including the modern e-cigarettes. All of these devices work through the heating of a liquid inside cartridges, producing aerosolized vapor inhaled to the lungs. The liquid in e-cigarettes can contain various components, such as vitamin E acetate (generally used as a diluent for tetrahydrocannabinol oil), being one of the ingredients to be implicated as a major causal agent of EVALI, because it has been found in BALF samples of a wide number of patients.
(4) However, there are many other components that are potentially pernicious when they are inhaled. Thus, it is still necessary to have a better understanding about the pathophysiology of EVALI, including studies on the chemistry and toxicology of those components, as well as on the mechanisms of molecular and cellular changes involved.
(5)The imaging presentations of EVALI are quite varied, characterized by ground-glass opacities (the dominating finding in the majority of patients), consolidations, interlobular septal thickening, and mosaic attenuation. Different radiological patterns have been described and correlated with different histopathological presentations, such as acute alveolar damage, eosinophilic pneumonia (EP), organizing pneumonia (OP), alveolar hemorrhage, hypersensitivity pneumonitis, lipoid pneumonia, and other mixed or nonclassifiable patterns.
(6) Although imaging findings are varied, a common point between the different patterns seems to exist: the bilaterality of parenchymal changes. These changes may be diffuse or predominate in one of the lung (upper or lower) fields.
In our patient, the initial chest CT demonstrated consolidations and ground-glass opacities in the lower lobes, some assuming annular or semi-annular forms, resembling the reversed halo sign, which is usually seen in the classic OP pattern.
(7) The imaging findings in patients with COVID-19 pneumonia, as well as in those with other viral pneumonias, can partially be attributed to secondary OP.
(8) The investigation was continued with transbronchial biopsy and BALF analysis, which revealed a high number of eosinophils and EP, respectively. EP has overlapping imaging findings with OP, and they can be distinguished by the indirect demonstration of peripheral eosinophilia or by direct demonstration of eosinophilic infiltrates.
(9) EP can have different triggering factors, including the use of e-cigarettes and viral infections. Recently, a case of EP associated with COVID-19 has been reported,
(10) and there was clinical and radiological improvement after treatment with prednisolone, which is similar to what occurred with our patient.
In conclusion, in the face of negative laboratory testing for SARS-CoV-2 and other infectious agents, negative rheumatological tests, the fact that our patient reported e-cigarette use, and the rapid clinical response after she discontinued that use and completed corticosteroid therapy, we reached the diagnosis of EVALI-related EP.
REFERENCES
- Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020;35(4):219-227. https://doi.org/10.1097/RTI.0000000000000524
- World Health Organization [homepage on the Internet]. Geneva: WHO [cited 2021 Jan 1]. WHO global report on trends in prevalence of tobacco smoking 2000-2025 – Second Edition. [Adobe Acrobat document, 121p.]. Available from: https://www.who.int/tobacco/publications/surveillance/trends-tobacco-smoking-second-edition/en/
- Kalininskiy A, Bach CT, Nacca NE, Ginsberg G, Marraffa J, Navarette KA, et al. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. Lancet Respir Med. 2019;7(12):1017-1026. https://doi.org/10.1016/S2213-2600(19)30415-1
- Blount BC, Karwowski MP, Shields PG, Morel-Espinosa M, Valentin-Blasini L, Gardner M, et al. Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI. N Engl J Med. 2020;382(8):697-705. https://doi.org/10.1056/NEJMoa1916433
- Chand HS, Muthumalage T, Maziak W, Rahman I. Pulmonary Toxicity and the Pathophysiology of Electronic Cigarette, or Vaping Product, Use Associated Lung Injury. Front Pharmacol. 2020;10:1619. https://doi.org/10.3389/fphar.2019.01619
- Panse PM, Feller FF, Butt YM, Smith ML, Larsen BT, Tazelaar HD, et al. Radiologic and Pathologic Correlation in EVALI. AJR Am J Roentgenol. 2020;215(5):1057-1064. https://doi.org/10.2214/AJR.20.22836
- Baque-Juston M, Pellegrin A, Leroy S, Marquette CH, Padovani B. Organizing pneumonia: what is it? A conceptual approach and pictorial review. Diagn Interv Imaging. 2014;95(9):771-777. https://doi.org/10.1016/j.diii.2014.01.004
- Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, et al. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology. 2020;296(2):E55-E64. https://doi.org/10.1148/radiol.2020200843
- Arakawa H, Kurihara Y, Niimi H, Nakajima Y, Johkoh T, Nakamura H. Bronchiolitis obliterans with organizing pneumonia versus chronic eosinophilic pneumonia: high-resolution CT findings in 81 patients. AJR Am J Roentgenol. 2001;176(4):1053-1058. https://doi.org/10.2214/ajr.176.4.1761053
- Murao K, Saito A, Kuronuma K, Fujiya Y, Takahashi S, Chiba H. Acute eosinophilic pneumonia accompanied with COVID-19: a case report. Respirol Case Rep. 2020;8(9):e00683. https://doi.org/10.1002/rcr2.683