
Gender differences have no effect on recurrent PCR positivity in patients with COVID-19: a meta-analysis and systematic review
Introduction
Coronavirus disease 2019 (COVID-19) becomes a global pandemic and is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). At present, it is believed that SARS-CoV-2 belongs to the β-coronavirus genus (2). The clinical manifestations of COVID-19 patients mainly involved the fever, fatigue, and dry cough. A few patients develop the symptoms such as nasal congestion, runny nose, sore throat, muscle aches and diarrhea. Severe cases often progress rapidly to acute respiratory distress syndrome, septic shock, metabolic acidosis, and coagulopathy (3). The elderly, male, smokers and those with chronic underlying diseases have a poor prognosis (4).
Currently in China, as long as the COVID-19 patients meet the following conditions, they can be discharged for observation: (I) the body temperature is normal for more than three days; (II) the respiratory symptoms are significantly improved; (III) the lung imaging shows that the acute exudation lesions are significantly improved; (IV) twice consecutive sputum and throat swabs of the above patients were negative for viral nucleic acid (at least 24 hours apart) (5). However, there are reports in the literature that patients have a positive viral nucleic acid test during follow-up after discharge (6,7). The research showed that Chinese males were more susceptible to SARS-CoV-2 infection than females (8) and there are different symptoms between the males and females (9). Moreover, gender differences are the most common patient information in clinical work. Therefore, we wondered whether there were gender differences in recurrent PCR positivity in COVID-19 patients and conducted a meta-analysis of recurrent PCR positivity in COVID-19 patients between different genders. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/aoi-20-10).
Methods
Research strategy
On June 4, 2020, we searched English databases, such as Pubmed, Embase, Cochrane Library, and Web of Science, and Chinese databases, such as China National Knowledge Infrastructure Database, Wanfang Data, Traditional Chinese Medicine Database, and VIP Database, by using keywords such as "covid 19 virus", "severe acute respiratory syndrome coronavirus 2", "SARS COV 2", "severe acute respiratory syndrome coronavirus 2", "COVID-19", "relapse" and "recurrent". The process and results of the literature search are shown in Figure 1.
Study selection
The Inclusion criteria in this study included the following requirements: (I) the studies’ design must conform to case inclusion and rationality; (II) the study type should be case-control study Cohort studies; (III) the research topic should cover the recurrent PCR positivity in COVID-19 patients; (IV) the reported data of eligible studies should include the total number of males and the total number of females come from recurrent group and non- recurrent separately.
Exclusion criteria included the following requirements: (I) duplicate publications; (II) literature review; (III) pieces of literature in the same area in the same year; (IV) the definition of related diseases given in the article is ambiguous; (V) non-Chinese or English literature.
Two reviewers (Wang, Ren) reviewed the main title and abstract separately and independently to select potential full-text articles for further review based on inclusion and exclusion criteria. When the title and abstract were not rejected by either reviewer, the two reviewers (Wang, Ren) separately and independently read the full text of the included literature and carefully checked whether the included article met the exclusion criteria. The inclusion or exclusion of each study was determined by discussion and consensus between the two reviewers.
Data extraction
The data were extracted by two reviewers (Wang, Ren), and the results were checked after the relevant data were extracted. The differences were resolved through discussion, and a consensus was reached among the two reviewers. The two reviewers (Wang, Ren) observed the included case-control and cohort studies and designed a table for data extraction using Excel. The extracted data included the first author, year of publication, type of study, patient source, and patient sample size.
Quality assessment
We excluded irrelevant literature by reading the title of the article, eliminating duplicate published clinical studies, and reading the full text to find documents that met the inclusion criteria. The two reviewers then evaluated the quality of each study that met the inclusion criteria using the Newcastle-Ottawa scale (NOS).
Meta analyses
Meta-analysis was performed using Stata15 software. Q test and I2 analyses were used to evaluate the heterogeneity between the included studies. When P>0.1 and I2<50%, it indicated that there was no statistical heterogeneity in each study, and the data was analyzed using the fixed effect model; otherwise, we used the random effect model to analyze the data. Funnel chart analysis was used to identify the presence of publication bias.
Results
Literature search
After searching the literature, there were a total of 447 related articles from the electronic database. After removing the duplicate literature, 45 of these articles were excluded. After completing a preliminary screening by reviewing the titles and abstracts, 382 articles were excluded. After further reading the full text, eventually, the remaining 4 studies were included in further meta-analyses. Details of full-text screening and study selection process are illustrated in Figure 1.
Basic characteristics and quality evaluation
A total of 4 articles (10-13) were included in this study. All patients were laboratory confirmed as COVID-19 patients. The specific basic characteristics are shown in Table 1. We used the NOS scale to rate the literature we included. The star ratings of the included literature were all greater than 6 stars, which met the basic conditions for our meta-analysis. The specific star rating by the NOS scale is shown in Table 1.
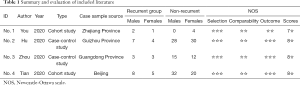
Full table
Gender differences
Analysis of the gender differences included a total of 4 works of literature. After heterogeneity testing (Figure 2), we obtained I2=0% and P>0.1, indicating that there was almost no heterogeneity in the combined literature. Using the fixed effect model, we found the OR=1.418 (95% CI 0.657 to 3.061; P=0.373), indicating no statistical differences in the distribution of sex between recurrent group and non-recurrent (Figure 2). The funnel plot for this study was symmetrical (Figure 3).
Discussion
As mentioned in the literature, COVID-19 is an emerging disease that has features of high infectivity and high mortality (14,15). More and more literature confirmed the existence of COVID-19 patients with recurrent PCR positivity. Therefore, research on the recurrent PCR positivity of COVID-19 patients is fundamental to manage the disease.
Gender differences showed different susceptibility to multiple viral infections. According to Vidal’s (16) research results, compared with males, females were a high-risk group of Chikungunya virus, but it was not clear whether this phenomenon was caused by immune response, genetics, lifestyle or environmental factors. As for the epidemiology aspect of COVID-19, Wu et al. (17) summarized the clinical data of 72314 COVID-19 patients and found that Chinese males were more susceptible to SARS-CoV-2 infection than females. The meta-analysis conducted by Li (8) confirmed these studies. As for symptoms of COVID-19, Radosław et al. (9) found that in non-hospitalized COVID-19 patients, there were gender differences in the frequency of gastrointestinal symptoms, olfactory and taste disorders. Based on the available data, older male adults and people of any age who have chronic underlying morbidities might be at higher risk for severe illness and fatal outcome from COVID-19 (18). However, from our meta-analysis studies basing on the existing literature, gender differences did not play a corresponding role in the recurrent PCR positivity of COVID-19 patients, which means gender differences may not be the reason for the recurrent PCR positivity and there may be other causes.
The current research considered that differences between males and females in the severity of COVID-19 disease might be related to angiotensin-converting enzyme 2 (ACE2). ACE2 is related to physiopathology of SARS-CoV-2, and Zhou et al. (19) found that the expression of ACE2 of different species in HeLa cells could lead to the infection and replication of SARS-CoV-2, thus directly indicating that SARS-CoV-2 used the ACE2 as the receptor to invade host cells. Interestingly, ACE2 is widely distributed in different organs and may show differences in different ages and sexes (18). As risk factors of COVID-19, smoking could be a risk factor of COVID-19 disease and it is related to higher expression of ACE2 (20). The distribution and content of ACE2 in different genders are different, which seems to explain the gender difference of COVID-19. However, from our meta-analysis studies basing on the existing literature, gender differences did not play a corresponding role in the recurrent PCR positivity of COVID-19 patients, which means the distribution and content of ACE2 have nothing with the recurrent PCR positivity of COVID-19 patients. Zheng et al. (21) carried out the study to show the many recurrent PCR positivity of COVID-19 patients were in asymptomatic condition. Our study’s results seen to explain this phenomenon according to the above findings.
At present, the reasons for recurrent PCR positivity of COVID-19 are attributed to two aspects. On the one hand, the study found that some patients who appeared recurrent PCR positivity had more severe symptoms than before, and it could be ruled out the relapse of the disease (22). On the other hand, due to reasons such as the medical environment, we speculated the patient’s nucleic acid test before the discharge might be false negative. We have always been unclear about the difference between two occasions when the patient’s virus nucleic acid tested positive again after being discharged from the hospital, but our research suggested that the distribution and content of ACE-2 had nothing to do with the recurrent PCR positivity and ACE-2 was related to severe of the COVID-19, which means patients may be in a condition of long-term PCR positivity rather than recurrent PCR positivity.
Due to the limited information in the included studies, the impact of gender differences on recurrent PCR positivity of COVID-19 patients cannot be fully evaluated, which is limiting this study. We need more relevant literature for further meta-analysis so that more conclusions can be confirmed and corrected.
Acknowledgments
We are very grateful for the data support provided by MD Di Tian (Center of Infectious Diseases, Beijing Ditan Hospital, Capital Medical University. Beijing, China).
Funding: This study was supported by the National Science and Technology Major Project of China (2018ZX09711003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/aoi-20-10
Peer Review File: Available at http://dx.doi.org/10.21037/aoi-20-10
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoi-20-10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and Cardiovascular Disease. Circulation 2020;141:1648-55. [Crossref] [PubMed]
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565-74. [Crossref] [PubMed]
- Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect 2020;80:656-65. [Crossref] [PubMed]
- Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect 2020;81:e16-25. [Crossref] [PubMed]
- China National Health Commission. Diagnosis and treatment of 2019-nCoV pneumonia in China (version 7) [in Chinese]. Published March 4, 2020. Accessed March 5, 2020.
- Zhao Y, Wu W, He H, et al. Analysis of re-positive nucleic acid conversion in patients recovered from COVID-19 in Tianjin. Acta Academiae Medicinae Militaris Tertiae 2020;42:879-82.
- Zhang B, Liu S, Dong Y, et al. Positive rectal swabs in young patients recovered from coronavirus disease 2019 (COVID-19). J Infect 2020;81:e49-52. [Crossref] [PubMed]
- Li LQ, Huang T, Wang Y, et al. 2019 novel coronavirus patients clinical characteristics, discharge rate and fatality rate of meta- analysis. J Med Virol 2020;92:577-83. [Crossref] [PubMed]
- Radosław S, Jarosław P, Mateusz J, et al. Gender differences in the frequency of gastrointestinal symptoms and olfactory or taste disorders among 1,942 non-hospitalized patients with COVID-19. Pol Arch Intern Med 2020.
- Li Y, Hu Y, Zhang X, et al. Follow-up testing of viral nucleic acid in discharged patients with moderate type of COVID-19. Zhejiang Da Xue Xue Bao Yi Xue Ban 2020;49:270-4.
- Hu R, Jiang Z, Gao H, et al. Recurrent Positive Reverse Transcriptase-Polymerase Chain Reaction Results for Coronavirus Disease 2019 in Patients Discharged From a Hospital in China. JAMA Netw Open 2020;3:e2010475 [Crossref] [PubMed]
- Zhou L, Wei F, Zhou J, et al. Factors influencing the outcome of 34 patients with COVID-19. The Journal of Practical Medicine 2020.
- Tian D, Wang L, Wang X, et al. Clinical research and factors associated with prolonged duration of viral shedding in patients with COVID-19. 2020.
- Song QQ, Zhao H, Fang LQ, et al. Study on assessing early epidemiological parameters of COVID-19 epidemic in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020;41:461-5. [PubMed]
- Davide T, Alessandro V, Manuela V. COVID-19 Fatality Rate and Performed Swabs in Italy: a Misleading Perception. J Med Internet Res 2020;
- Vidal OM, Jorge AR, Jesús P, et al. Chikungunya outbreak (2015) in the Colombian Caribbean: Latent classes and gender differences in virus infection. PLoS Negl Trop Dis 2020;14:e0008281 [Crossref] [PubMed]
- Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239-42. [Crossref] [PubMed]
- Ambrosino I, Barbagelata E, Ortona E, et al. Gender differences in patients with COVID-19: a narrative review. Monaldi Arch Chest Dis 2020;90. [Crossref] [PubMed]
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270-3. [Crossref] [PubMed]
- Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med 2020;8:e20 [Crossref] [PubMed]
- Zheng KI, Wang XB, Jin XH, et al. A Case Series of Recurrent Viral RNA Positivity in Recovered COVID-19 Chinese Patients. J Gen Intern Med. 2020;35:2205-6. [Crossref] [PubMed]
- Wang X, Xu H, Jiang H, et al. The Clinical Features and Outcomes of Discharged Coronavirus Disease 2019 Patients: A Prospective Cohort Study. QJM 2020; [Crossref] [PubMed]
Cite this article as: Wang X, Ren X, Ge Z, Cui S, Chen Z. Gender differences have no effect on recurrent PCR positivity in patients with COVID-19: a meta-analysis and systematic review. Ann Infect 2021;5:1.





