- Department of Maternal and Child Health and Ministry of Education (MOE) Key Lab of Environment and Health, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Background: The long-term mental health effects of coronavirus disease 2019 (COVID-19) in children are rarely reported. We aimed to investigate the progression of depressive and anxiety symptoms among a cohort of children in the initial epicenter of COVID-19 in China.
Methods: Two waves of surveys were conducted in the same two primary schools in Wuhan and Huangshi, Hubei province: Wave 1 from 28 February to 5 March, 2020 (children had been confined to home for 30–40 days) and Wave 2 from 27 November to 9 December, 2020 (schools had reopened for nearly 3 months). Depressive and anxiety symptoms were estimated using the Children's Depression Inventory – Short Form (CDI-S) and the Screen for Child Anxiety Related Emotional Disorders (SCARED), respectively. ΔCDI-S and ΔSCARED scores between Wave 2 and Wave 1 were calculated and further categorized into tertiles. Multivariable linear regression and multinomial logistic regression models were then applied.
Results: A total of 1,224 children completed both surveys. The prevalence of mental health outcomes at Wave 2 increased significantly compared to Wave 1, specifically depressive symptoms (age-standardized prevalence rates: 37.5 vs. 21.8%) and anxiety symptoms (age-standardized prevalence rates: 24.0 vs. 19.6%). Higher ΔSCARED scores were observed in females and children in Wuhan, and children with experience of neglect had higher ΔCDI-S (β = 1.12; 95% CI = 0.67–1.58) and ΔSCARED (β = 6.46; 95% CI = 4.73–8.19) scores compared with those without experience of neglect. When the Δ scores were further categorized into tertiles, similar results were found.
Conclusions: The prevalence of depressive and anxiety symptoms after schools resumed was increased compared with that during the home quarantine period, even though the COVID-19 pandemic was under control. Females and children in Wuhan, and also children with experience of neglect were at increased risk of mental health disorders.
Introduction
Mental health has been increasingly seen as a major public health problem. It is estimated that between 10 and 20% of children and adolescents suffer from some type of mental health disorder (1). As most mental health disorders begin in childhood, a sensitive period of child development, early identification and treatment of mental health needs during this time is essential (2).
The coronavirus disease 2019 (COVID-19) outbreak was declared a pandemic by the World Health Organization (WHO), and COVID-19 emergency measures (i.e., city-wide lockdown) began in Wuhan, Hubei province on 23 January, 2020. This was eventually followed by other cities in Hubei province (3, 4). According to the Ministry of Education, the COVID-19 pandemic has caused long-term home restrictions for 180 million primary and secondary school students (5). In Hubei province, primary schools have been closed and shifted to home-based distance-learning models for the whole Spring semester. Hence, children did not have face-to-face learning until September 2020. Recent literature suggested that COVID-19 itself, along with school closures and home quarantine caused by COVID-19, has adversely affected children's mental health (6–9). COVID-19 has become a major global threat, impacting the mental well-being of children (10, 11). A series of studies from Effects of home Confinement on multiple Lifestyle Behaviours during the COVID-19 outbreak (ECLB-COVID19), an international online survey on mental health and multi-dimensional lifestyle behaviors during home confinement, have also highlighted the significant impact that home confinement has had on health, mental well-being, mood, life satisfaction, and multidimensional lifestyle behaviors (12–17). COVID-19 home confinement has negatively impacted mental health, with a greater proportion of people experiencing psychosocial and emotional disorders (14).
A range of mental health problems have accompanied the pandemic, such as depressive/anxiety disorders and post-traumatic stress disorder (PTSD) (18). For instance, isolated children had average PTSD scores that were four times higher than those of children who were not isolated (19). The mental health problems of children could continue into adulthood and adversely affect their physical and mental health (11). Depressive and anxiety symptoms are considered to be the early stages of major depressive disorder and anxiety disorder (20, 21), both of which could lead to poor academic performance, impaired cognitive function, social problems, and impaired psychosocial functions (20–22). The COVID-19 pandemic and the related measures against it, including self-isolation, quarantine, and social distancing, could have a detrimental impact on mental health. Individuals had to face significant changes in everyday life, possibly causing acute fight-or-flight responses (23). Uncertainty, fear, and discrimination toward infected people and their family members might generate psychological consequences that would need to be addressed by professionals and psychiatrists (24). The psychiatric problems that accompanied COVID-19 might therefore be a marathon rather than a sprint (25).
Until now, the majority of existing studies have focused on cross-sectional data, which cannot examine the long-term impact of COVID-19 over time (26–28). Our previous cross-sectional study conducted between 28 February and 5 March 2020 found that the prevalence of depressive (17.2%) and anxiety (18.9%) symptoms of children in Hubei province was higher than from other surveys in China (6). One longitudinal cohort study of children and adolescents in an area of China with a low risk of COVID-19 showed that the prevalence of psychological symptoms was higher after school reopening (on May 2020) than before the COVID-19 outbreak (29). Therefore, there is an urgent need for long-term follow-up studies on the psychological symptoms of school-aged children, especially those in the high risk area of the COVID-19 outbreak (30). We aimed to examine depressive and anxiety symptoms among a cohort of children after school reopening in Wuhan and Huangshi, Hubei province, China based on our previous study about the mental health status of children during the COVID-19 outbreak (6). We hypothesized that the impact of COVID-19 on the mental health of children may be long term and that the mental health status of children may worsen over time.
Materials and Methods
Study Design
At Wave 1, we conducted the survey among children in Grades 2–6 at two primary schools in Hubei province from 28 February to 5 March 2020 through an online crowd-sourcing platform. At that time, children had been confined in their home for 30–40 days. Children took the online survey after their guardian agreed to the statement “I permit my child to participate in the survey” in the survey link. Detailed information were shown in our previous article (6).
At Wave 2, we conducted the second survey at the same schools between 27 November and 9 December 2020 on site. At that time, cities had been unsealed for nearly 7 months and schools had reopened for nearly 3 months. We obtained oral informed consent from parents by inquiring through head teachers. The investigators organized children to independently accomplish the questionnaires in class and encouraged them to complete the questionnaire as much as possible.
This study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. Informed consent of the children and their guardians was obtained after the nature of the procedures had been fully explained. There was no disclosed information that might identify a particular person. All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Study Population
Wave 1
A total of 2,330 children in Grades 2–6 from two primary schools in Hubei province were invited to participate the survey and 1,784 participants completed the survey (675 children residing in Wuhan and 1,109 in Huangshi). The response rate was 76.6%. All questionnaires passed the quality audit, and the effective rate was 100.0%.
Wave 2
Children were promoted to the next grade in September each year, and all the children in the two primary schools were promoted at Wave 2. Therefore, the second survey started with children in Grade 3. As children in Grade 6 at Wave 1 were promoted from the primary school to the junior middle school, they were not included in the follow-up at Wave 2. A total of 2,245 children in Grades 3–6 from the same schools, including 698 from Wuhan and 1,547 from Huangshi, were invited to participate in the survey at Wave 2. Among these children, 2,211 completed the survey, with a response rate of 98.5%. After a quality audit, 2,209 questionnaires were further analyzed, with an effective rate of 99.9%.
Using student names and IDs, we matched the questionnaires from both waves. There was a total of 1,224 children who completed both surveys, with 689 (56.3%) male and 805 (65.8%) participats who resided in Huangshi. The data from those 1,224 children were used in all analyses.
Measures
In both surveys, the gender, grade, location of school, and depressive and anxiety symptoms of participants were collected. In China, children aged 6 enter primary school and are about 11 years old when they are in grade 6. Thus, the grade could be a good approximation of age. Detailed information was shown in our previous article (6). Depressive and anxiety symptoms were measured using the Children's Depression Inventory—Short Form (CDI-S) and the Screen for Child Anxiety Related Emotional Disorders (SCARED), respectively. Additionally, at Wave 1, COVID-19-related questions were collected. At Wave 2, the daily sleep time in the past week and experience of neglect in the previous year were measured and collected via five items in the Conflict Tactics Scales, Parent-child Version (CTSPC).
Depressive symptoms
Depressive symptoms were estimated using the CDI-S at Waves 1 and 2 (31). The CDI-S consists of 10 items, each with a score of 0–2. Each item requires respondents to rate the severity of each symptom of depression. The CDI-S has shown good internal consistency (Cronbach's α = 0.75) in the study with Chinese children (32). The total score ranges from 0 to 20. A higher score indicates more severe depressive symptoms, while a CDI-S value of ≥ 4 is defined as depressive symptoms (33). The difference (Δ) in CDI-S score between Wave 2 and Wave 1 was calculated via subtraction, with a positive/negative change representing an increase/decrease of CDI-S score at Wave 2, respectively. Based on the tertiles of the ΔCDI-S score, it is further categorized into low (< 1), moderate (≥ 1, < 3), and high (≥ 3) change.
Anxiety Symptoms
Screen for Child Anxiety Related Emotional Disorders is a 41-item self-report instrument that was used to measure anxiety symptoms at Waves 1 and 2 (34). The questionnaire proved to have adequate reliability (retest reliability: 0.567–0.608; internal consistency: 0.890) and fair validity (correlation coefficients from 0.300 to 0.444) (35). Children rate each symptom on a three-point Likert scale: 0 (almost never), 1 (sometimes), and 2 (often). Total scores ranged from 0 to 82, and the accepted cut-off score for anxiety disorder is 23 (35). Children with higher scores have more severe symptoms of anxiety. The ΔSCARED score between Wave 2 and Wave 1 was calculated and was used to indicate an increase/decrease of SCARED score in Wave 2. Based on the tertiles of the ΔSCARED score, it is further categorized into low (< 0), moderate (≥ 0, < 11), and high (≥ 11) change.
Neglect
Five items covering neglect behaviors in the CTSPC were used to measure the experience of neglect (36). Children were asked to report their experience of neglect in the preceding year at Wave 2. Thus, children's experience of neglect at the time of the first survey was also covered. The affirmative responses to any item were used to represent self-reported exposure to neglect.
With regard to COVID-19, children were asked to answer two questions at Wave 1: 1) “Which are more likely the host of SARS-CoV-2?,” with choices that include “wild animals,” “domesticated animals,” and “do not know,” and 2) “Which of the following protective measures have you taken during the COVID-19 outbreak?,” with choices that include “Reminding my family members to wear masks,” “Convince my family members not to go out or gathering,” “Ventilating the house frequently,” and “Washing hands frequently.” Children who chose wild animals and those who had taken all protective measures were deemed to know the host of SARS-CoV-2 and how to take protective measures during the COVID-19 pandemic.
Statistical Analysis
All analyses were performed in Statistical Package for the Social Sciences (SPSS) 22.0 and Microsoft Excel (2016). Both R (v3.2.5) and Microsoft Excel (2016) were used to generate the figures. Frequencies and percentages were summarized for categorical variables. Means and standard deviations were used to describe continuous variables. Age-standardized prevalence rates of depressive and anxiety symptoms were calculated based on the Chinese population from the 2020 China census data (37). We used McNemar's test to evaluate the trend in the prevalence of psychological symptoms between the two waves. We also performed multivariable linear regression models to examine the ΔCDI-S and ΔSCARED scores. Multinomial logistic regression models were applied to examine the tertiles of the ΔCDI-S and ΔSCARED scores. Multiple imputation with 20 times interpolation was carried out for independent variables that had a few nonresponses [daily sleep time (missing data, 20.5%) and neglect behaviors (missing data, 0.8%)]. Sensitivity analysis using the complete data was also performed to evaluate the validity of multiple imputation. The odds ratio (OR), β value, and 95% confidence interval (95% CI) were reported and p-values were two-tailed, with a significance level at 0.05.
Results
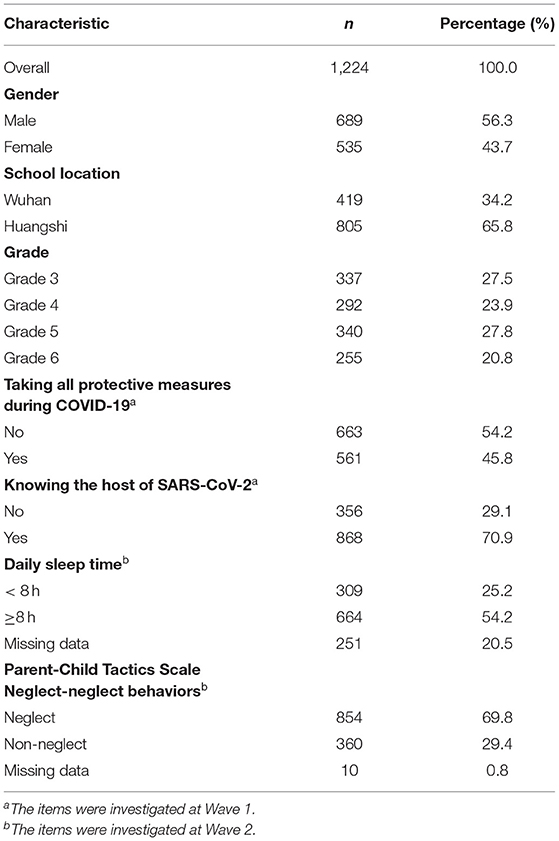
Among 1,224 children who completed both surveys, 689 (56.3%) children were males and 805 (65.8%) resided in Huangshi. The average ages of children were 9.32 ± 1.10 years at Wave 1 and 10.07 ± 1.10 years at Wave 2, with 1.1% of children lacking age information. The percentages of participants in Grades 3–6 were 27.5% (337), 23.9% (292), 27.8% (340), and 20.8% (255), respectively. There were 45.8% of children who took all required protective measures during COVID-19 and 70.9% who knew the host of SARS-CoV-2 at Wave 1. Additionally, 54.2% of children had more than 8 h of daily sleep time and 69.8% showed that they had experience of neglect in the preceding year at Wave 2 (Table 1).
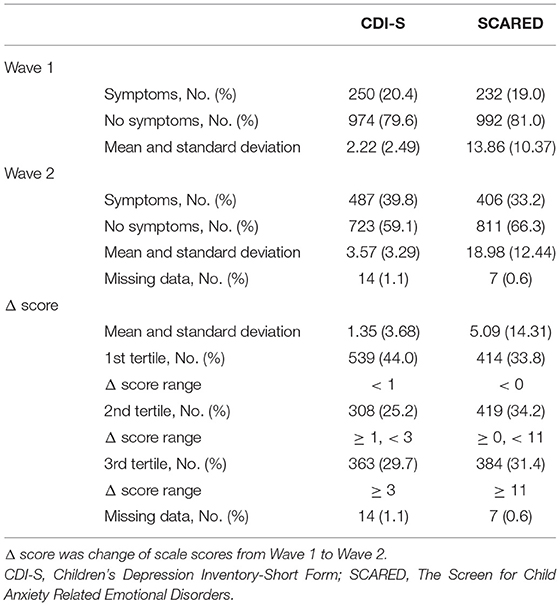
Age-standardized prevalence rates of depressive symptoms at Wave 1 and Wave 2 were 21.8 and 37.5%, respectively, and were 19.6 and 24.0%, respectively, for anxiety symptoms. A total of 20.4% (250) of participants had depressive symptoms at Wave 1 and 39.8% (487) at Wave 2. The average score of the CDI-S rose from 2.22 (2.49) for Wave 1 to 3.57 (3.29) for Wave 2. For the anxiety symptoms, 19% (232) of children were detected at Wave 1 and 33.2% (406) were detected at Wave 2. The average score of SCARED were 13.86 (10.37) and 18.98 (12.44), respectively (Table 2). The distributions of ΔCDI-S and ΔSCARED were shown in Supplementary Figure S1. The mean score of CDI-S and SCARED for the two waves was reported in Supplementary Figure S2A. For both scales, we found that the score was increased at Wave 2 compared with those at Wave 1 for each grade. The mean and standard deviations of ΔCDI-S and ΔSCARED were 1.35 (3.68) and 5.09 (14.31), respectively (Table 2). As shown in Supplementary Figure S2B, children in Wuhan had a higher change of SCARED score than those in Huangshi.
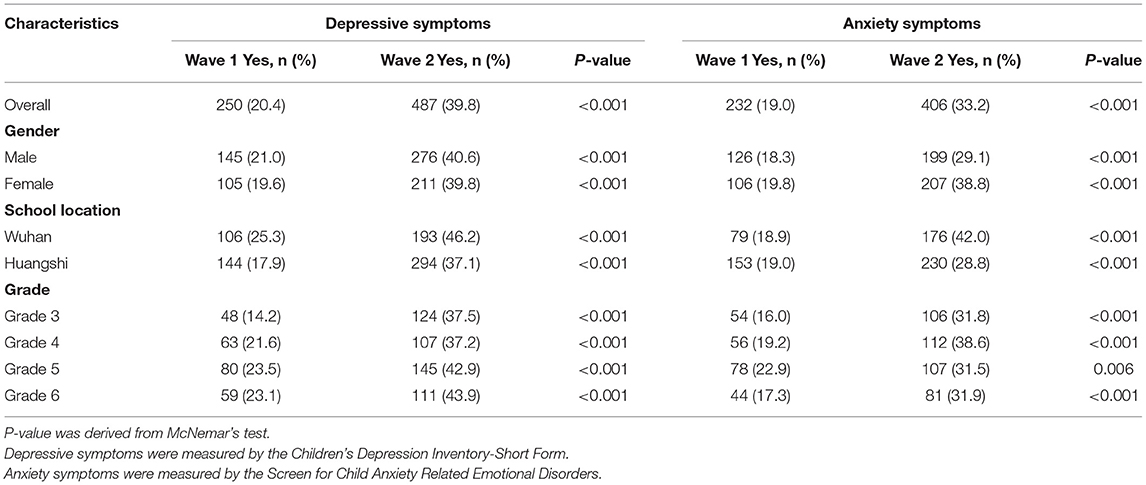
As shown in Table 3, the prevalence of mental health outcomes among children at Wave 2 significantly increased from those levels at Wave 1, specifically in depressive symptoms [39.8% (Wave 2) vs. 20.4% (Wave 1), p < 0.001] and anxiety symptoms [33.2% (Wave 2) vs. 19.0% (Wave 1), p < 0.001]. Further subset analyses for gender, grade, and school location showed similar results (all p < 0.001). Tables 4, 5 showed the OR and β for associations of Δ score and demographic characteristics in the regression models. Children with experience of neglect had higher ΔCDI-S scores (β = 1.12; 95% CI = 0.67–1.58) and ΔSCARED score (β = 6.46; 95% CI = 4.73–8.19) compared with those without neglect. Children with experience of neglect had higher odds in the 3rd tertile of the ΔCDI-S score (OR = 2.51; 95%CI = 1.82–3.47). Similar results were found for ΔSCARED score (2nd tertile vs. 1st tertile, OR = 1.37; 95% CI = 1.02–1.84; 3rd tertile vs. 1st tertile, OR = 3.46; 95% CI = 2.45–4.89). Females had significantly higher Δ score of SCARED than males (β = 1.83; 95% CI = 0.26–3.40) and children in Wuhan had significantly higher ΔSCARED score than those in Huangshi (β = 3.42; 95% CI = 1.77–5.07). Children in Wuhan had higher odds in the third tertile of ΔCDI-S score (OR = 1.38; 95% CI = 1.03–1.83) and the third tertile of ΔSCARED score (OR = 1.65; 95% CI = 1.22–2.25). We also found that students in Grade 4 and 5 had lower ΔCDI-S score compared with those students in Grade 3 (β = −0.93; 95% CI = −1.50 to −0.36; β = −0.68; 95% CI = −1.23 to −0.14). The sensitivity analyses that used complete data before multiple imputation showed similar results (Supplementary Tables S1, S2).
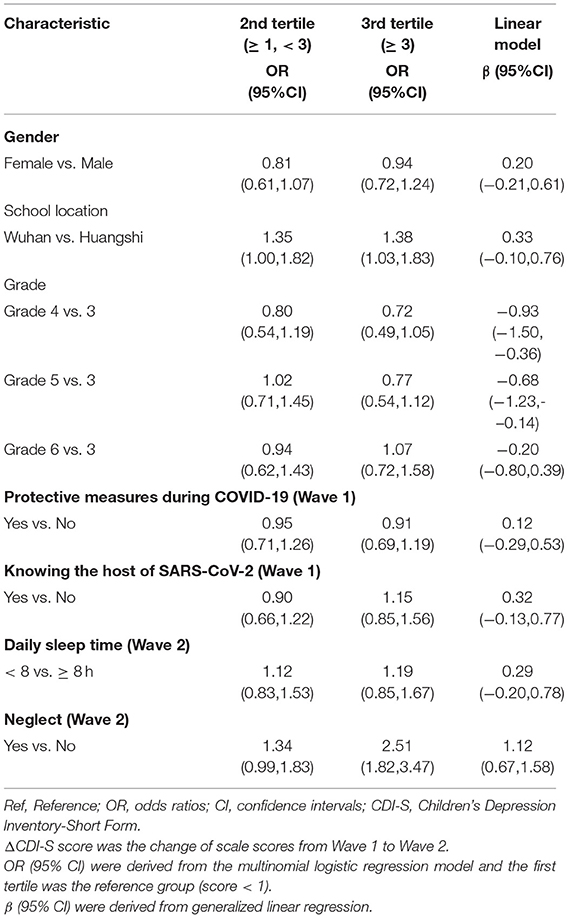
Table 4. Association between demographic characteristics and the difference in Children's Depression Inventory-short form (ΔCDI-S) score.

Table 5. Association between demographic characteristics and difference in Screen for Child Anxiety Related Emotional Disorders (ΔSCARED) score.
Discussion
This study suggested that about 3 months after school reopening, the prevalence of depressive and anxiety symptoms among children in Hubei province remained elevated compared with that during the COVID-19 pandemic lockdown. When considering the ΔCDI-S and ΔSCARED scores, the risk factors for a high change from Wave 1 to Wave 2 were: the school in Wuhan, being female, and having experience of neglect.
The psychological and mental effects of major public health events could be long term (38–40). Lessons from the outbreak of severe acute respiratory syndrome (SARS) in 2003 indicated that the mental health of survivors did not improve over time and gradually deteriorated (41). The post-traumatic disturbance of residents in areas with high SARS prevalence, regardless of age, was more intense than in areas with low prevalence (42). A national mental health study among adolescents in China, administered separately in February and April 2020, showed that the prevalence of depression and anxiety significantly increased over time (43). In addition, surveys covering 5,285 adults in the USA found that the prevalence of adverse mental health symptoms during the later phase of the COVID-19 pandemic (September 2020) was higher than in June 2020 (44). Daly et al. found that a pronounced and prolonged deterioration of mental health occurred between April and June 2020 among participants of the nationally representative United Kingdom Household Longitudinal Study (45). Studies in Italy showed an increase in stress and depression among citizens along with a different time course of mental health problems between men and women (46, 47). Our results among children in Hubei province, China, were consistent with these findings. Although different socio-cultural contexts (i.e., tight and loose cultures) led to a varied response to a global pandemic (48), COVID-19 seemed to have a similar impact on the long-term consequences of mental health.
The significant increase in the prevalence of depressive and anxiety symptoms may be related to the fact that an online mental health service in the early phase of COVID-19 in China was not designed for children (49). Children who developed psychological symptoms at Wave 1 may persist with these symptoms until Wave 2 due to lack of effective intervention. For children with depressive symptoms, there will be considerable difficulties in resuming normal life after school reopening (50). The other important thing to note in this study was that we used screening criteria, rather than clinical thresholds, of the CDI-S (≥ 7) (51) and SCARED (≥ 25) (52). This was because we tried to screen out more children at high or potential risk from the aspect of early prevention, especially for the children in Wuhan who experienced the pandemic earlier and more severely. Although the sample size was limited and is not fully representative of the population in Hubei province, the evidence of increased depressive and anxiety symptoms suggested that there is a great need to provide timely psychological support to enhance resilience and reduce fear and anxiety (53). On a related note, timely mental health education and treatment should be available for these children (54).
Consistent with previous findings, females had higher SCARED scores in our study (43, 55). The gender difference in anxiety symptoms may be partly attributable to relationships between adrenarcheal hormones and functional connectivity of the amygdala according to an imaging study in children (56). Hormone levels in females were inversely associated with the connection from the right amygdala to the insula, but were positively associated with the connection from the left amygdala to anterior cingulate cortex in males. Furthermore, we found that children in Wuhan at Wave 2 had a higher ΔSCARED score than those in Huangshi, which may be attributed to the fact that the epidemic in Wuhan was more severe than in Huangshi, and that children in Wuhan have been isolated at home for longer periods (57). Moreover, we found higher ΔCDI-S and ΔSCARED scores at Wave 2 in children with experience of neglect in the preceding year vs. those without neglect. The experience of neglect over the past year also included the children's experience at the time of the first survey. This may be partly attributed to the fact that children might have a decreased frequency of positive parent–child interaction after the school reopened, which increased the probability of neglect (58). Changes to daily family life due to financial hardship and social restrictions on parents may increase parental stress and lead to an increase in adverse childhood experiences (ACEs), including neglect (59). In this study, 69.8% of children reported experience of neglect in the preceding year at Wave 2, which was higher than a previous study among Chinese elementary students in Shanghai, China (52.26%) (60). ACEs, such as abuse and neglect, are associated with increased risk for depression, anxiety, and PTSD (61), along with elevated mortality rates (62). Although Chinese parents have a more democratic parenting style influenced by Western thoughts, the power disparity between parents and children in traditional Chinese culture may facilitate ACEs. Support for dealing with family difficulties and available child welfare services are needed.
Although we explored psychological problems among the cohort of children in Hubei province, China, there were several limitations. First, the results may be generalized only to children in school. We adopted a cluster sampling method and selected two primary schools for the surveys. The sample was therefore not necessarily representative of the whole population of children in China. Second, no information on household income or other types of ACEs was surveyed. The impact of the COVID-19 pandemic may be related to parental unemployment/loss of household income and high-stress home environments, thus increasing the likelihood of ACEs or emotional problems (63). We also did not collect information related to family functioning or family context. Third, children in higher grades were more likely to suffer from mental health problems (64). The students in Grade 6 at Wave 1 were lost during follow-up due to promotion from primary school to junior middle school, which may lead to an underestimation of the prevalence of depressive and anxiety problems at Wave 2. Fourth, we did not collect information on learning styles. The learning styles were inconsistent between the two surveys (home learning vs. studying on campus), which may have an impact on the mental health of students. Furthermore, we used electronic questionnaires when students were confined to home and paper-based questionnaires when students were at school. Although we adopted some methods to ensure that students completed the questionnaires independently, we still need to unify the form of survey tools in future studies. Finally, we reported the symptoms rather than the clinical diagnoses because of the short follow-up period.
In conclusion, our study identified increased prevalence of depressive and anxiety symptoms among a cohort of children in Hubei province, China, despite the fact that the COVID-19 pandemic had been brought under control and schools had reopened. The mental health problems of children are warnings. There is a lack of knowledge on the long-term psychological impact of COVID-19 on children, and our results fill an important gap in the research. In addition, China is one of the early affected countries whose schools are now functioning normally. Our study, focusing on the progression of psychological symptoms in children who have experienced long-term home quarantine and have now resume school, may guide the mental health support plan in other countries (65). We anticipate that our results may be helpful to decision makers and that post-COVID-19 public health for mental health protection be given priority. Schools, which are the primary provider of mental health services for many children (66), should take timely action to mitigate the disruption of COVID-19 on children when they return to school, especially those who have experienced neglect within their families (2). For psychiatrists and healthcare professionals, they may participate in educational and media activities for children, parents, or educators about the mental health distress caused by physical distancing and quarantine. They should also alert policy makers of the long-term consequences of COVID-19 and the increased demand for mental health services (67). Continuing to follow-up these children and giving attention to their emotional problems is also necessary.
Data Availability Statement
The datasets presented in this article are not readily available because the data are not publicly available due to privacy/ethical restrictions: Requests to access the datasets should be directed to RS, songranran@hust.edu.cn.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. Written/oral informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
XX and RS conceived the study. XX, QL, KZ, YF, and RS critically appraised the data. XX, KZ, QJ, XW, and PX prepared the initial manuscript. RS reviewed and edited the manuscript. All authors collected data for the study and critically reviewed and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the children who participated in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.809107/full#supplementary-material
References
1. World Health Organization. Child and Adolescent Mental Health. (2020). Available online at: https://www.who.int/mental_health/maternal-child/child_adolescent/en/ (accessed on May 3,2021).
2. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. (2020) 174:819–820. doi: 10.1001/jamapediatrics.2020.1456
3. Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in wuhan, China. JAMA. (2020) 323:1915–1923. doi: 10.1001/jama.2020.6130
4. Tian H, Liu Y, Li Y, Wu CH, Chen B, Kraemer MUG, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. (2020) 368:638–42. doi: 10.1126/science.abb6105
5. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. (2020) 395:945–7. doi: 10.1016/S0140-6736(20)30547-X
6. Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei province, China. JAMA Pediatr. (2020) 174:898–900. doi: 10.1001/jamapediatrics.2020.1619
7. Bignardi G, Dalmaijer ES, Anwyl-Irvine AL, Smith TA, Siugzdaite R, Uh S, et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child. (2020) 106:791–7. doi: 10.31219/osf.io/v7f3q
8. Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. (2021) 8:535–50. doi: 10.1016/S2215-0366(21)00025-0
9. Gassman-Pines A, Ananat EO, Fitz-Henley II J2nd. COVID-19 and parent-child psychological well-being. Pediatrics. (2020) 146:e2020007294. doi: 10.1542/peds.2020-007294
10. Campion J, Javed A, Sartorius N, Marmot M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry. (2020) 7:657–9. doi: 10.1016/S2215-0366(20)30240-6
11. Clark H, Coll-Seck AM, Banerjee A, Peterson S, Dalglish SL, Ameratunga S, et al. A future for the world's children? A WHO-UNICEF-lancet commission. Lancet. (2020) 395:605–58. doi: 10.1016/S0140-6736(19)32540-1
12. Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, et al. Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 international online survey. Int J Environ Res Public Health. (2021) 18:4329. doi: 10.3390/ijerph18084329
13. Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol Sport. (2021) 38:495–506. doi: 10.5114/biolsport.2021.101605
14. Ammar A, Trabelsi K, Brach M, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. (2021) 38:9–21. doi: 10.5114/biolsport.2020.96857
15. Ammar A, Chtourou H, Boukhris O, Trabelsi K, Masmoudi L, Brach M, et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicenter study. Int J Environ Res Public Health. (2020) 17:6237. doi: 10.3390/ijerph17176237
16. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. (2020) 12:1583. doi: 10.3390/nu12061583
17. Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PLoS ONE. (2020) 15:e0240204. doi: 10.1371/journal.pone.0240204
18. Morganstein JC, Ursano RJ. Ecological disasters and mental health: causes, consequences, and interventions. Front Psychiatry. (2020) 11:1. doi: 10.3389/fpsyt.2020.00001
19. Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. (2013) 7:105–10. doi: 10.1017/dmp.2013.22
20. Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry. (2010) 196:365–71. doi: 10.1192/bjp.bp.109.071191
21. Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. (2011) 377:2093–102. doi: 10.1016/S0140-6736(11)60512-6
22. Kusi-Mensah K, Donnir G, Wemakor S, Owusu-Antwi R, Omigbodun O. Prevalence and patterns of mental disorders among primary school age children in Ghana: correlates with academic achievement. J Child Adolesc Ment Health. (2019) 31:214–23. doi: 10.2989/17280583.2019.1678477
23. Marazziti D, Stahl SM. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. (2020) 19:261. doi: 10.1002/wps.20764
24. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) 63:e32. doi: 10.1192/j.eurpsy.2020.35
25. Unutzer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. (2020) 19:130–131. doi: 10.1002/wps.20766
26. Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2025591. doi: 10.1001/jamanetworkopen.2020.25591
27. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
28. Qin Z, Shi L, Xue Y, Lin H, Zhang J, Liang P, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the covid-19 pandemic in China. JAMA Netw Open. (2021) 4:e2035487. doi: 10.1001/jamanetworkopen.2020.35487
29. Zhang L, Zhang D, Fang J, Wan Y, Tao F, Sun Y. Assessment of mental health of chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2021482. doi: 10.1001/jamanetworkopen.2020.21482
30. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
31. Ahlen J, Ghaderi A. Evaluation of the Children's depression inventory-short version (CDI-S). Psychol Assess. (2017) 29:1157–66. doi: 10.1037/pas0000419
32. Guo J, Chen L, Wang X, Liu Y, Chui CH, He H, et al. The relationship between Internet addiction and depression among migrant children and left-behind children in China. Cyberpsychol Behav Soc Netw. (2012) 15:585–90. doi: 10.1089/cyber.2012.0261
33. Allgaier AK, Fruhe B, Pietsch K, Saravo B, Baethmann M, Schulte-Korne G. Is the children's depression inventory short version a valid screening tool in pediatric care? A comparison to its full-length version. J Psychosom Res. (2012) 73:369–74. doi: 10.1016/j.jpsychores.2012.08.016
34. Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. (1997) 36:545–53. doi: 10.1097/00004583-199704000-00018
35. Wang K, Lin-Yan SU, Zhu Y. Norms of the screen for child anxiety related emotional disorders in Chinese urban children. Chin J Clin Psychol. (2002) 10:270–2. doi: 10.3969/j.issn.1005-3611.2002.04.009
36. Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse Negl. (1998) 22:249–70. doi: 10.1016/S0145-2134(97)00174-9
37. National Bureau of Statistics of China. China Statistical Yearbook. (2020). Available online at: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm (accessed February 26, 2021).
38. Hou F, Liu Z, Xiang Y, Zeng Z, Hu X, Li T, et al. Follow-Up study of psychological self-report symptoms for middle school students in Wenchuan earthquake-stricken areas. Chin J Sch Health. (2010) 31:1188–90. doi: 10.16835/j.cnki.1000-9817.2010.10.017
39. Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. (2021) 34:100806. doi: 10.1016/j.eclinm.2021.100806
40. Del Rio C, Collins LF, Malani P. Long-term Health Consequences of COVID-19. JAMA. (2020) 324:1723–4. doi: 10.1001/jama.2020.19719
41. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
42. Lee TM, Chi I, Chung LW, Chou KL. Ageing and psychological response during the post-SARS period. Aging Ment Health. (2006) 10:303–11. doi: 10.1080/13607860600638545
43. Chen X, Qi H, Liu R, Feng Y, Li W, Xiang M, et al. Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: a comparison of two cross-sectional studies. Transl Psychiatry. (2021) 11:148. doi: 10.1038/s41398-021-01271-4
44. Czeisler ME, Lane RI, Wiley JF, Czeisler CA, Howard ME, Rajaratnam SMW. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, september 2020. JAMA Netw Open. (2021) 4:e2037665. doi: 10.1001/jamanetworkopen.2020.37665
45. Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. (2020) 13:1–10. doi: 10.1017/S0033291720004432
46. Roma P, Monaro M, Colasanti M, Ricci E, Biondi S, Di Domenico A, et al. A 2-month follow-up study of psychological distress among italian people during the COVID-19 lockdown. Int J Environ Res Public Health. (2020) 17:8180. doi: 10.3390/ijerph17218180
47. Salfi F, Lauriola M, Amicucci G, Corigliano D, Viselli L, Tempesta D, et al. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: A longitudinal study on the Italian population. Neurobiol Stress. (2020) 13:100259. doi: 10.1016/j.ynstr.2020.100259
48. Gelfand MJ, Raver JL, Nishii L, Leslie LM, Lun J, Lim BC, et al. Differences between tight and loose cultures: a 33-nation study. Science. (2011) 332:1100–4. doi: 10.1126/science.1197754
49. Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8
50. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
51. Comiskey CM, O'Sullivan K, Quirke MB, Wynne C, Hollywood E, S MG. Baseline results of the first healthy schools evaluation among a community of young, Irish, urban disadvantaged children and a comparison of outcomes with international norms. J Sch Health. (2012) 82:508–13. doi: 10.1111/j.1746-1561.2012.00730.x
52. Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. (1999) 38:1230–6. doi: 10.1097/00004583-199910000-00011
53. Amsalem D, Dixon LB, Neria Y. The coronavirus disease 2019 (COVID-19) outbreak and mental health: current risks and recommended actions. JAMA Psychiatry. (2021) 78:9–10. doi: 10.1001/jamapsychiatry.2020.1730
54. Raviv T, Warren CM, Washburn JJ, Kanaley MK, Eihentale L, Goldenthal HJ, et al. Caregiver perceptions of children's psychological well-being during the COVID-19 pandemic. JAMA Netw Open. (2021) 4:e2111103. doi: 10.1001/jamanetworkopen.2021.11103
55. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. doi: 10.1007/s00787-020-01541-4
56. Barendse MEA, Simmons JG, Byrne ML, Patton G, Mundy L, Olsson CA, et al. Associations between adrenarcheal hormones, amygdala functional connectivity and anxiety symptoms in children. Psychoneuroendocrinology. (2018) 97:156–63. doi: 10.1016/j.psyneuen.2018.07.020
57. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
58. Shan W, Zhang Y, Zhao J, Zhang Y, Cheung EFC, Chan RCK, et al. Association between maltreatment, positive parent-child interaction, and psychosocial well-being in young children. J Pediatr. (2019) 213:180–6 e1. doi: 10.1016/j.jpeds.2019.06.050
59. Calvano C, Engelke L, Di Bella J, Kindermann J, Renneberg B, Winter SM. Families in the COVID-19 pandemic: parental stress, parent mental health and the occurrence of adverse childhood experiences-results of a representative survey in Germany. Eur Child Adolesc Psychiatry. (2021). doi: 10.1007/s00787-021-01739-0. [Epub ahead of print].
60. Sun X. Child maltreatment and quality of life among urban chinese children. J Interpers Violence. (2020) 36:NP13077-NP13093. doi: 10.1177/0886260519900331
61. Turecki G, Ota VK, Belangero SI, Jackowski A, Kaufman J. Early life adversity, genomic plasticity, and psychopathology. Lancet Psychiatry. (2014) 1:461–6. doi: 10.1016/S2215-0366(14)00022-4
62. Ostergaard SD, Larsen JT, Petersen L, Smith GD, Agerbo E. Psychosocial Adversity in infancy and mortality rates in childhood and adolescence: a birth cohort study of 1.5 million individuals. Epidemiology. (2019) 30:246–55. doi: 10.1097/EDE.0000000000000957
63. Solerdelcoll M, Arango C, Sugranyes G. Calling for the integration of children's mental health and protection into COVID-19 responses. Rev Psiquiatr Salud Ment. (2021) 14:113–6. doi: 10.1016/j.rpsm.2021.02.004
64. Thienkrua W, Cardozo BL, Chakkraband ML, Guadamuz TE, Pengjuntr W, Tantipiwatanaskul P, et al. Symptoms of posttraumatic stress disorder and depression among children in tsunami-affected areas in southern Thailand. JAMA. (2006) 296:549–59. doi: 10.1001/jama.296.5.549
65. Rimmer A. Covid-19: Government must plan for schools to reopen, say paediatricians. BMJ. (2020) 369:m2458. doi: 10.1136/bmj.m2458
66. Dibner KA, Schweingruber HA, Christakis DA. Reopening K-12 schools during the COVID-19 pandemic: a report from the national academies of sciences, engineering, and medicine. JAMA. (2020) 324:833–4. doi: 10.1001/jama.2020.14745
Keywords: depressive symptom, anxiety symptom, school-aged children, coronavirus disease 2019, longitudinal study
Citation: Xie X, Liu Q, Zhu K, Jiang Q, Feng Y, Xiao P, Wu X and Song R (2022) Psychological Symptom Progression in School-Aged Children After COVID-19 Home Confinement: A Longitudinal Study. Front. Psychiatry 13:809107. doi: 10.3389/fpsyt.2022.809107
Received: 04 November 2021; Accepted: 15 March 2022;
Published: 13 April 2022.
Edited by:
Daria Smirnova, Samara State Medical University, RussiaReviewed by:
Gaia Sampogna, University of Campania “L. Vanvitelli”, ItalyChongjian Wang, Zhengzhou University, China
Hamdi Chtourou, University of Sfax, Tunisia
Copyright © 2022 Xie, Liu, Zhu, Jiang, Feng, Xiao, Wu and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ranran Song, songranran@hust.edu.cn
 Xinyan Xie
Xinyan Xie Qi Liu
Qi Liu Ranran Song
Ranran Song