An Explainable Machine Learning Approach for COVID-19’s Impact on Mood States of Children and Adolescents during the First Lockdown in Greece
Abstract
:1. Introduction
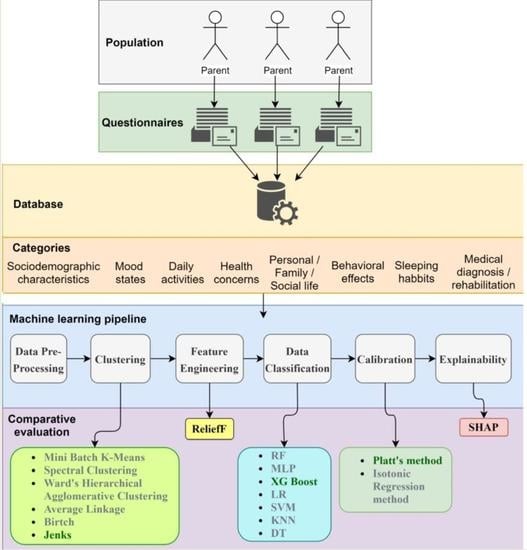
2. Background
- The use of an explainable machine learning pipeline with multiple comparative evaluations among the ML stages to guarantee the development of an accurate prediction model;
- The use of a post hoc explainability model to diagnose and interpret the most contributed factors to the prediction output of the model and thus to identify the factors that led to mood alteration or stability during the first lockdown in Greece;
- The incorporation of 71 heterogeneous features from 10 different categories, such as demographics, social life, personal life, family life, daily activities, health concerns and behavioral effects, sleep habits, mood state, and medical diagnosis/rehabilitation;
- The application to the vulnerable group of population [31], such as children and adolescents with pre-existing psychiatric and/or developmental disorders, is incorporated in order to further understand the impact of COVID-19 and its restrictions by identifying the factors that contributed most to the mood state alteration of the population under examination during the first lockdown in Greece. To achieve this, machine learning tools were employed following a post-hoc explainability analysis.
3. Materials and Methods
3.1. Data Collection
3.2. Data Preprocessing
3.3. Clustering Methods
3.4. Feature Engineering
3.5. Data Classification
3.6. Post Hoc Explainability
4. Results
4.1. Evaluation Methodology
4.2. Results
4.2.1. Clustering
4.2.2. Feature Selection
4.2.3. Classification and Calibration
4.2.4. Post-Hoc Explainability
5. Discussion
5.1. Clustering
5.2. Feature Selection
5.3. Classification and Calibration
5.4. Post Hoc Explainability
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV); World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bonardi, J.-P.; Gallea, Q.; Kalanoski, D.; Lalive, R. Fast and Local: How Did Lockdown Policies Affect the Spread and Severity of COVID-19? Covid Econ 2020, 23, 325–351. [Google Scholar]
- Ma, Z.; Idris, S.; Zhang, Y.; Zewen, L.; Wali, A.; Ji, Y.; Pan, Q.; Baloch, Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: An online survey. BMC Pediatr. 2021, 21, 95. [Google Scholar] [CrossRef]
- Abas, M.A.; Weobong, B.; Burgess, R.A.; Kienzler, H.; Jack, H.E.; Kidia, K.; Musesengwa, R.; Petersen, I.; Collins, P.Y.; Nakimuli-Mpungu, E. COVID-19 and global mental health. Lancet Psychiatry 2021, 8, 458–459. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Vizheh, M.; Qorbani, M.; Arzaghi, S.M.; Muhidin, S.; Javanmard, Z.; Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020, 19, 1967–1978. [Google Scholar] [CrossRef]
- Qin, Z.; Shi, L.; Xue, Y.; Lin, H.; Zhang, J.; Liang, P.; Lu, Z.; Wu, M.; Chen, Y.; Zheng, X.; et al. Prevalence and Risk Factors Associated with Self-reported Psychological Distress Among Children and Adolescents During the COVID-19 Pandemic in China. JAMA Netw. Open 2021, 4, e2035487. [Google Scholar] [CrossRef]
- McKune, S.L.; Acosta, D.; Diaz, N.; Brittain, K.; Beaulieu, D.J.; Maurelli, A.T.; Nelson, E.J. Psychosocial health of school-aged children during the initial COVID-19 safer-at-home school mandates in Florida: A cross-sectional study. BMC Public Health 2021, 21, 603. [Google Scholar] [CrossRef]
- Ren, H.; Luo, X.; Wang, Y.; Guo, X.; Hou, H.; Zhang, Y.; Yang, P.; Zhu, F.; Hu, C.; Wang, R.; et al. Psychological responses among nurses caring for patients with COVID-19: A comparative study in China. Transl. Psychiatry 2021, 11, 273. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Tamarit, A.; de la Barrera, U.; Mónaco, E.; Schoeps, K.; Montoya-Castilla, I. Psychological Impact of COVID-19 Pandemic in Spanish Adolescents: Risk and Protective Factors of Emotional Symptoms. Rev. Psicol. Clin. Con Ninos Y Adolesc. 2020, 7, 73–80. [Google Scholar] [CrossRef]
- Chen, X.; Qi, H.; Liu, R.; Feng, Y.; Li, W.; Xiang, M.; Cheung, T.; Jackson, T.; Wang, G.; Xiang, Y.-T. Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: A comparison of two cross-sectional studies. Transl. Psychiatry 2021, 11, 148. [Google Scholar] [CrossRef]
- Tavolacci, M.; Wouters, E.; Van de Velde, S.; Buffel, V.; Déchelotte, P.; Van Hal, G.; Ladner, J. The Impact of COVID-19 Lockdown on Health Behaviors among Students of a French University. Int. J. Environ. Res. Public Health 2021, 18, 4346. [Google Scholar] [CrossRef]
- Fu, W.; Yan, S.; Zong, Q.; Anderson-Luxford, D.; Song, X.; Lv, Z.; Lv, C. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2020, 280, 7–10. [Google Scholar] [CrossRef]
- Xiao, H.; Shu, W.; Li, M.; Li, Z.; Tao, F.; Wu, X.; Yu, Y.; Meng, H.; Vermund, S.H.; Hu, Y. Social Distancing among Medical Students during the 2019 Coronavirus Disease Pandemic in China: Disease Awareness, Anxiety Disorder, Depression, and Behavioral Activities. Int. J. Environ. Res. Public Health 2020, 17, 5047. [Google Scholar] [CrossRef] [PubMed]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors associated with mental health disorders among College students in France confined during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Ren, Z.; Xin, Y.; Ge, J.; Zhao, Z.; Liu, D.; Ho, R.C.M.; Ho, C.S.H. Psychological Impact of COVID-19 on College Students After School Reopening: A Cross-Sectional Study Based on Machine Learning. Front. Psychol. 2021, 12, 641806. [Google Scholar] [CrossRef] [PubMed]
- Cost, K.T.; Crosbie, J.; Anagnostou, E.; Birken, C.S.; Charach, A.; Monga, S.; Kelley, E.; Nicolson, R.; Maguire, J.L.; Burton, C.L.; et al. Mostly worse, occasionally better: Impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur. Child Adolesc. Psychiatry 2021, 6, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.-J.; Wang, L.-L.; Yang, R.; Yang, X.-J.; Zhang, L.-G.; Guo, Z.-C.; Chen, J.-C.; Wang, J.-Q.; Chen, J.-X. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020, 74, 39–47. [Google Scholar] [CrossRef]
- Islam, A.; Barna, S.D.; Raihan, H.; Alam Khan, N.; Hossain, T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS ONE 2020, 15, e0238162. [Google Scholar] [CrossRef]
- Yeasmin, S.; Banik, R.; Hossain, S.; Hossain, M.N.; Mahumud, R.; Salma, N.; Hossain, M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: A cross-sectional study. Child. Youth Serv. Rev. 2020, 117, 105277. [Google Scholar] [CrossRef] [PubMed]
- De Avila, M.A.G.; Filho, P.T.H.; Jacob, F.; Alcantara, L.R.S.; Berghammer, M.; Nolbris, M.J.; Olaya-Contreras, P.; Nilsson, S. Children’s Anxiety and Factors Related to the COVID-19 Pandemic: An Exploratory Study Using the Children’s Anxiety Questionnaire and the Numerical Rating Scale. Int. J. Environ. Res. Public Health 2020, 17, 5757. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Sciberras, E.; Patel, P.; Stokes, M.A.; Coghill, D.; Middeldorp, C.M.; Bellgrove, M.A.; Becker, S.P.; Efron, D.; Stringaris, A.; Faraone, S.V.; et al. Physical Health, Media Use, and Mental Health in Children and Adolescents With ADHD during the COVID-19 Pandemic in Australia. J. Atten. Disord. 2020, 1087054720978549. [Google Scholar] [CrossRef] [PubMed]
- Ge, F.; Zhang, D.; Wu, L.; Mu, H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: A Longitudinal Study Using a Machine Learning. Neuropsychiatr. Dis. Treat. 2020, 16, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Prout, T.A.; Zilcha-Mano, S.; Doorn, K.A.-V.; Békés, V.; Christman-Cohen, I.; Whistler, K.; Kui, T.; Di Giuseppe, M. Identifying Predictors of Psychological Distress During COVID-19: A Machine Learning Approach. Front. Psychol. 2020, 11, 586202. [Google Scholar] [CrossRef] [PubMed]
- Rens, E.; Smith, P.; Nicaise, P.; Lorant, V.; Broeck, K.V.D. Mental Distress and Its Contributing Factors Among Young People During the First Wave of COVID-19: A Belgian Survey Study. Front. Psychiatry 2021, 12, 575553. [Google Scholar] [CrossRef] [PubMed]
- Blakemore, S.-J.; Mills, K.L. Is Adolescence a Sensitive Period for Sociocultural Processing? Annu. Rev. Psychol. 2014, 65, 187–207. [Google Scholar] [CrossRef]
- Peng, K.; Leung, V.C.M.; Huang, Q. Clustering Approach Based on Mini Batch Kmeans for Intrusion Detection System Over Big Data. IEEE Access 2018, 6, 11897–11906. [Google Scholar] [CrossRef]
- Von Luxburg, U. A tutorial on spectral clustering. Stat. Comput. 2007, 17, 395–416. [Google Scholar] [CrossRef]
- Ward, J.H., Jr. Hierarchical Grouping to Optimize an Objective Function. J. Am. Stat. Assoc. 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Murtagh, F.; Legendre, P. Ward’s Hierarchical Agglomerative Clustering Method: Which Algorithms Implement Ward’s Criterion? J. Classif. 2014, 31, 274–295. [Google Scholar] [CrossRef] [Green Version]
- Sokal, R.R.; Michener, C.D. A Statistical Method of Evaluating Systematic Relationships. Univ. Kans. Sci. Bull. 1958, 38, 1409–1438. [Google Scholar]
- Yim, O.; Ramdeen, K.T. Hierarchical Cluster Analysis: Comparison of Three Linkage Measures and Application to Psychological Data. Quant. Methods Psychol. 2015, 11, 8–21. [Google Scholar] [CrossRef]
- Zhang, T.; Ramakrishnan, R.; Livny, M. BIRCH: An efficient data clustering method for very large databases. ACM SIGMOD Rec. 1996, 25, 103–114. [Google Scholar] [CrossRef]
- Zhang, T.; Ramakrishnan, R.; Livny, M. BIRCH: A New Data Clustering Algorithm and Its Applications. Data Min. Knowl. Discov. 1997, 1, 141–182. [Google Scholar] [CrossRef]
- Anchang, J.; Ananga, E.O.; Pu, R. An efficient unsupervised index based approach for mapping urban vegetation from IKONOS imagery. Int. J. Appl. Earth Obs. Geoinf. 2016, 50, 211–220. [Google Scholar] [CrossRef]
- North, M.A. A Method for Implementing a Statistically Significant Number of Data Classes in the Jenks Algorithm. In Proceedings of the 2009 Sixth International Conference on Fuzzy Systems and Knowledge Discovery, Tianjin, China, 14–16 August 2009; Volume 1, pp. 35–38. [Google Scholar]
- Zhang, L.; Zhang, X.; Yuan, S.; Wang, K. Economic, Social, and Ecological Impact Evaluation of Traffic Network in Beijing–Tianjin–Hebei Urban Agglomeration Based on the Entropy Weight TOPSIS Method. Sustainability 2021, 13, 1862. [Google Scholar] [CrossRef]
- Robnik-Šikonja, M.; Kononenko, I. Theoretical and Empirical Analysis of ReliefF and RReliefF. Mach. Learn. 2003, 53, 23–69. [Google Scholar] [CrossRef] [Green Version]
- Spolaôr, N.; Cherman, E.A.; Monard, M.C.; Lee, H.D. ReliefF for Multi-Label Feature Selection. In Proceedings of the 2013 Brazilian Conference on Intelligent Systems, Fortaleza, Brazil, 19–24 October 2013; pp. 6–11. [Google Scholar]
- Alelyani, S. Stable bagging feature selection on medical data. J. Big Data 2021, 8, 11. [Google Scholar] [CrossRef]
- Huang, Y.; McCullagh, P.J.; Black, N.D. An optimization of ReliefF for classification in large datasets. Data Knowl. Eng. 2009, 68, 1348–1356. [Google Scholar] [CrossRef]
- Kilicarslan, S.; Adem, K.; Celik, M. Diagnosis and classification of cancer using hybrid model based on ReliefF and convolutional neural network. Med. Hypotheses 2020, 137, 109577. [Google Scholar] [CrossRef]
- Kononenko, I. Estimating Attributes: Analysis and Extensions of RELIEF. In Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 1994; Volume 784, pp. 171–182. [Google Scholar]
- Kononenko, I.; Robnik-Sikonja, M.; Robnik, M.; Pompe, U. ReliefF for Estimation and Discretization of Attributes in Classification, Regression, and ILP Problems. Artif. Intell. Methodol. Syst. Appl. 1996, 31–40. [Google Scholar]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. Prediction of Joint Space Narrowing Progression in Knee Osteoarthritis Patients. Diagnostics 2021, 11, 285. [Google Scholar] [CrossRef]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. A Machine Learning Pipeline for Predicting Joint Space Narrowing in Knee Osteoarthritis Patients. In Proceedings of the 2020 IEEE 20th International Conference on Bioinformatics and Bioengineering (BIBE), Cincinnati, OH, USA, 26–28 October 2020; pp. 934–941. [Google Scholar]
- Liu, M.; Xu, X.; Tao, Y.; Wang, X. An Improved Random Forest Method Based on RELIEFF for Medical Diagnosis. In Proceedings of the 2017 IEEE International Conference on Computational Science and Engineering (CSE) and IEEE International Conference on Embedded and Ubiquitous Computing (EUC), Guangzhou, China, 21–24 July 2017; Volume 1, pp. 44–49. [Google Scholar]
- Jamshidi, A.; Pelletier, J.-P.; Martel-Pelletier, J. Machine-learning-based patient-specific prediction models for knee osteoarthritis. Nat. Rev. Rheumatol. 2018, 15, 49–60. [Google Scholar] [CrossRef]
- Harimoorthy, K.; Thangavelu, M. Multi-disease prediction model using improved SVM-radial bias technique in healthcare monitoring system. J. Ambient. Intell. Humaniz. Comput. 2020, 12, 3715–3723. [Google Scholar] [CrossRef]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. Identification of most important features based on a fuzzy ensemble technique: Evaluation on joint space narrowing progression in knee osteoarthritis patients. Int. J. Med. Inform. 2021, 156, 104614. [Google Scholar] [CrossRef]
- Shaik, A.B.; Srinivasan, S. A Brief Survey on Random Forest Ensembles in Classification Model. In Proceedings of the International Conference on Innovative Computing and Communications, Technical University of Ostrava, Ostrava, Czech Republic, 21–22 March 2019; Bhattacharyya, S., Hassanien, A.E., Gupta, D., Khanna, A., Pan, I., Eds.; Springer: Singapore, 2019; pp. 253–260. [Google Scholar]
- Ogunleye, A.A.; Wang, Q.-G. XGBoost Model for Chronic Kidney Disease Diagnosis. IEEE/ACM Trans. Comput. Biol. Bioinform. 2019, 17, 2131–2140. [Google Scholar] [CrossRef]
- Dreiseitl, S.; Ohno-Machado, L. Logistic regression and artificial neural network classification models: A methodology review. J. Biomed. Inform. 2002, 35, 352–359. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Chung, F.-L.; Wang, S. A SVM based classification method for homogeneous data. Appl. Soft Comput. 2015, 36, 228–235. [Google Scholar] [CrossRef]
- Mucherino, A.; Papajorgji, P.J.; Pardalos, P.M. K-Nearest Neighbor Classification. In Data Mining in Agriculture; Mucherino, A., Papajorgji, P.J., Pardalos, P.M., Eds.; Springer Optimization and Its Applications; Springer: New York, NY, USA, 2009; pp. 83–106. ISBN 978-0-387-88615-2. [Google Scholar]
- Kotsiantis, S.B. Decision trees: A recent overview. Artif. Intell. Rev. 2011, 39, 261–283. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A Unified Approach to Interpreting Model Predictions. In Proceedings of the Advances in Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017; Curran Associates, Inc.: New York, NY, USA, 2017; Volume 30. [Google Scholar]
- SMOTE|Overcoming Class Imbalance Problem Using SMOTE. Available online: https://www.analyticsvidhya.com/blog/2020/10/overcoming-class-imbalance-using-smote-techniques/ (accessed on 16 August 2021).
- Douzas, G.; Bacao, F.; Last, F. Improving imbalanced learning through a heuristic oversampling method based on k-means and SMOTE. Inf. Sci. 2018, 465, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Hornor, G. Resilience. J. Pediatr. Health Care 2017, 31, 384–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koome, F.; Hocking, C.; Sutton, D. Why Routines Matter: The Nature and Meaning of Family Routines in the Context of Adolescent Mental Illness. J. Occup. Sci. 2012, 19, 312–325. [Google Scholar] [CrossRef]
- Masten, A.S. Resilience Theory and Research on Children and Families: Past, Present, and Promise. J. Fam. Theory Rev. 2018, 10, 12–31. [Google Scholar] [CrossRef] [Green Version]
- Zolkoski, S.M.; Bullock, L.M. Resilience in children and youth: A review. Child. Youth Serv. Rev. 2012, 34, 2295–2303. [Google Scholar] [CrossRef]
- Masten, A.S. Global Perspectives on Resilience in Children and Youth. Child Dev. 2013, 85, 6–20. [Google Scholar] [CrossRef]
- Masten, A.S.; Barnes, A.J. Resilience in Children: Developmental Perspectives. Children 2018, 5, 98. [Google Scholar] [CrossRef] [Green Version]
- Masten, A.S.; Motti-Stefanidi, F. Multisystem Resilience for Children and Youth in Disaster: Reflections in the Context of COVID-19. Advers. Resil. Sci. 2020, 1, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Bouter, D.; Zarchev, M.; de Neve-Enthoven, N.; Ravensbergen, S.; Kamperman, A.M.; Hoogendijk, W.; Grootendorst, N. A Longitudinal Study of Mental Health in Adolescents before and during the COVID-19 Pandemi 2021. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Lopez-Serrano, J.; Díaz-Bóveda, R.; González-Vallespí, L.; Santamarina-Pérez, P.; Bretones-Rodríguez, A.; Calvo, R.; Lera-Miguel, S. Psychological impact during COVID-19 lockdown in children and adolescents with previous mental health disorders. Rev. Psiquiatr. Y Salud Ment. 2021. [Google Scholar] [CrossRef]
- Penner, F.; Ortiz, J.H.; Sharp, C. Change in Youth Mental Health During the COVID-19 Pandemic in a Majority Hispanic/Latinx US Sample. J. Am. Acad. Child Adolesc. Psychiatry 2020, 60, 513–523. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prati, G.; Mancini, A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Diminich, E. Annual Research Review: Positive adjustment to adversity-trajectories of minimal-impact resilience and emergent resilience. J. Child Psychol. Psychiatry 2012, 54, 378–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masten, A.S. Resilience of children in disasters: A multisystem perspective. Int. J. Psychol. 2020, 56, 1–11. [Google Scholar] [CrossRef]
- Giuntella, O.; Hyde, K.; Saccardo, S.; Sadoff, S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2016632118. [Google Scholar] [CrossRef]


















| Type of Measures | Measures | Explanation |
|---|---|---|
| International Measures | Curfew | The effective date when a country announced a restriction on the movement of individuals within a given time of the day |
| State of emergency | The effective date when a country announced a state of emergency | |
| Within-country regional lockdown | The effective date when a region within a country announced a total lockdown | |
| Partial selective lockdown | The earliest effective date for the partial restriction of the movement of people, i.e. school closures or limitations regarding the number of gathered people allowed | |
| External measures | Selective international border closures | The earliest effective date when a country decided to close its borders with a region or country that has been significantly affected by COVID-19 |
| Selective border closures | The earliest effective date following the selective international border closure, when a country closed its border to individuals from one or multiple other countries that have been significantly affected by COVID-19 | |
| International lockdown | The effective date when a country banned all flights, rail, and automotive movements internationally |
| Study | Country | Population | Target | Method |
|---|---|---|---|---|
| [2] | China | 8079 Chinese students aged 12–18 | To identify correlations between sociodemographic features and mental health problems in Chinese adolescents during the outbreak of COVID-19 | Multivariable logistic regression analysis |
| [4] | China | 668 Chinese children aged 7–15 | To identify the main factors that contribute to the education and the mental health of Chinese children during COVID-19 | Multiple logistic regression analysis |
| [25] | China | 584 youths | To study the effects of COVID-19 on youth mental health | Univariate analysis and univariate logistic regression |
| [14] | China | Two cross-sectional studies of 9554 and 3886 participants | To evaluate the factors that contribute to depression and anxiety among Chinese adolescents during COVID-19 | Multivariable logistic regression analyses |
| [19] | China | 1,199,320 school-aged children and adolescents | To assess the prevalence and the risk factors associated with self-reported psychological distress | Multivariate logistic regression |
| [21] | China | 11,835 Chinese adolescents and young adults (12–29 years) | To identify sleeping problems during COVID-19 | Binomial logistic regression analysis |
| [28] | China | 2009 Chinese undergraduate students | To predict anxiety and insomnia during COVID-19 | XGBoost model |
| [26] | China | 746,217 Chinese university students | To examine variables associated with mental health problems during COVID-19 | Univariate and hierarchical logistic regression analyses |
| [16] | China | 89,588 Chinese university students | To identify the risk factors for anxiety symptoms during COVID-19 | Multivariate logistic regression models |
| [17] | China | 933 medical students | To evaluate the impact of COVID-19 on anxiety | Multivariate logistic regression |
| [18] | France | 69,054 French university students | To study mental health issues due to COVID-19 | Multivariate logistic regression |
| [15] | France | 3671 participants | To identify the risk factors for depression during the COVID-19 pandemic | Multivariate logistic regression |
| [22] | Bangladesh | 476 university students | To identify the risk factors for depression due to COVID-19 | Binary logistic regression |
| [23] | Bangladesh | 384 parents with at least one child aged 5–15 | To identify mental health disturbances during COVID-19 | Binary logistic regression |
| [20] | Canada | 1013 children and adolescents aged 6–18, with or without pre-existing diagnoses | To evaluate the effects on mental health during COVID-19 | Multinomial logistic regression |
| [24] | Brazil | 157 girls and 132 boys aged 6–12 | To examine the prevalence of anxiety during COVID-19 | Logistic regression |
| [13] | Spain | 523 adolescents (13–17 years) | To examine the association between sociodemographic factors and COVID-19-related variables and their effect on depression, anxiety, and stress | Multivariable logistic regression |
| [27] | Australia | Parents of 213 children and adolescents aged 5–17 who have been diagnosed with ADHD | To identify the impact of COVID-19 restrictions | Adjusted logistic regression analyses |
| [19] | China | 478 college students after school reopening | To examine the psychological impact of COVID-19 | Multivariate logistic regression |
| [30] | Belgium | 2008 young people aged 16–25 | To examine mental distress and its contributing factors | Bivariate and multivariable logistic regression analyses |
| [29] | Cross-sectional study | 2787 participants aged 18–85 | To identify predictors of psychological distress during COVID-19 | Random forest machine learning algorithm and regression trees |
| [10] | Florida, USA | 280 school-aged children | To examine mental health during COVID-19 | Bivariate analysis and logistic and multinomial logistic regression models |
| Sociodemographic Characteristics | Population (%) |
|---|---|
| Age, Mean ± Standard Deviation | 10.7 ± 4.1 |
| Sex Male Female Not willing to answer | 466 (62.63%) 273 (36.7%) 5 (0.67%) |
| Participant parent Mother Father Other (grandparents, uncle/aunt, foster parents, other) | 588 (79.7%) 142 (19.2%) 8 (1.1%) |
| Parent’s ethnicity Greek Other | 725 (98.2%) 13 (1.8%) |
| Health insurance type National/Military Private Other None | 650 (87.7%) 63 (8.7%) 9 (1.3%) 16 (2.3%) |
| Residential area City Suburbs of a city Town/village Rural area Island | 382 (51.8%) 200 (27.1%) 131 (17.7%) 10 (1.4%) 15 (2.0%) |
| Reporting parent’s educational level Compulsory 9 years’ education Senior high school Institute of Vocational Training Technical College or University degree Postgraduate degree (M.Sc./PhD) | 26 (3.5%) 146 (19.8%) 118 (16.0%) 280 (37.9%) 168 (22.8%) |
| Second parent’s educational level Compulsory 9 years’ education Senior high school Institute of Vocational Training Technical College or University degree Postgraduate degree (M.Sc., PhD) | 80 (10.8%) 221 (29.9%) 105 (14.3%) 211 (28.6%) 121 (16.4%) |
| Essential worker (yes): healthcare, delivery worker, store worker, security, building maintenance | 321 (43.5%) |
| Worker in a facility treating COVID-19 (yes) | 105 (14.2%) |
| Job loss during the pandemic (yes) | 38 (5.1%) |
| Limited ability to earn money (yes) | 81 (10.9%) |
| Category | Features | Description |
|---|---|---|
| Demographics | age_group | Age group of child |
| gender_child | Gender of child | |
| parent_area_live | Area of residence | |
| gender_parent | Gender of the parent or guardian | |
| parenteducation | Education level of parent or guardian | |
| school_child | School enrolment and attendance | |
| 2w_essential_worker | Whether any adults living with the child are essential workers (health care, delivery services, pharmacies, law enforcement and security, store worker, cleaning services, other) | |
| Social life | 3m_outdoors | Days per week the child spent outside the house (parks, outdoor spaces) in 3 months and the past 2 weeks, respectively |
| 2w_outdoors | ||
| 2w_time_outside | Amount of time per week the child spent/dedicated out of the house (e.g., shopping, parks, etc.) | |
| 2w_event_cancellat | How difficult the cancellation of important events in the child’s life (graduation, vacation, Easter recess) was for him/her | |
| 2w_recommendations | Difficulty following recommendations regarding social distancing | |
| 2w_contact_changed | Change in the child’s contact with people outside home relatives compared to before the coronavirus/COVID-19 crisis | |
| 2w_relationships_friends | Change in the quality of the child’s relationships with his/her friends | |
| 3m_soc_media | Time spent using social media (e.g Facetime, Facebook, Instagram, Snapchat, Twitter, Tiktok) for 3 months and the past 2 weeks, respectively | |
| 2w_soc_media | ||
| Personal life | 2w_positive | Positive changes in the child’s life due to the coronavirus/COVID-19 crisis |
| Family life | Family_impact_any | If any event that affected the family occurred due to COVID-19 |
| 2w_financial_recod | Financial problems faced by the family due to the coronavirus/COVID-19 crisis | |
| 2w_relationships_family | Changes in the quality of relationships between the child and members of his/her family | |
| 2w_family_events_lost_job | Whether either of the following have happened to the child’s family members because of coronavirus/COVID-19: loss of job, loss of earnings | |
| 2w_family_events_loss_earnings | ||
| Daily activities | 3m_exercise | Days per week the child engaged in exercise (e.g., increased heart rate, breathing) for at least 30 min, for 3 months and the past 2 weeks, respectively |
| 2w_exercise | ||
| 2w_video_games | Time spent playing video games, for 3 months and the past 2 weeks, respectively | |
| 3m_video_games | ||
| 3m_tv | Time spent watching TV or digital means (e.g., Netflix, Youtube, or web surfing) for 3 months and the past 2 weeks, respectively | |
| 2w_tv | ||
| 2w_reading | How frequently the child asked questions, read, or talked about coronavirus/COVID-19 | |
| Health concerns | 2w_worry_self_infected | Child’s worry about becoming infected |
| 2w_worry_family_inf | Child’s worry about family members or friends becoming infected | |
| 2w_worry_phys_healt | Worry that physical health will be affected by coronavirus/COVID-19 | |
| 2w_worry_ment_health | Worry that the child’s mental/emotional health will be affected by coronavirus/COVID-19 | |
| Behavioral effects | 2w_stress_restrict | Stress caused by the curfew |
| 2w_stress_family | Stress caused to the child by changes in family contacts | |
| 2w_worry_food_reco | Worry about food in the family running out due to loss of income | |
| 2w_stress_social | Stress caused to the child by changes to his/her social contacts | |
| 2w_living_stability | Child’s concern about the stability of the family’s living situation | |
| 2w_hopeful_end | How hopeful the child is that the coronavirus/COVID-19 crisis will end | |
| Sleeping habits | 3m_sleep_hours | Average sleep duration on weekdays, for 3 months and the past 2 weeks, respectively |
| 2w_sleep_hours_rec | ||
| 3m_sleep_time | Sleep schedule on weekdays, for 3 months and the past 2 weeks, respectively | |
| 2w_sleep_time_reco | ||
| 3m_sleep_hours_weeke | Average sleep duration on weekends, for 3 months and the past 2 weeks, respectively | |
| 2w_sleep_hours_wee | ||
| 3m_sleep_time_weeken | Sleep schedule on weekends, for 3 months and the past 2 weeks, respectively | |
| 2w_sleep_time_week | ||
| Medical diagnosis/rehabilitation | 2w_child_health_evaluation | Parental evaluation of the child’s overall physical health before the coronavirus/COVID-19 crisis |
| 2w_mental_health_eval | Parental evaluation of the child’s overall mental/emotional health before the coronavirus/COVID-19 crisis | |
| diagnosis_1_group | Diagnosis defined by the medical expert | |
| Diagnosis_FINAL_groups | Final diagnostic category defined by the medical expert | |
| 2w_symptoms_tot | Symptoms the child had | |
| 2w_all_exposure_tot | Child exposed to someone likely to have coronavirus/COVID-19 | |
| 2w_support_activit | Supports which were in place for the child and have been disrupted | |
| 2w_family_diagnosis | Whether any members of the child’s family have been diagnosed with COVID-19 | |
| 2w_family_events_ho | Whether any of the following have happened to the child’s family members because of Coronavirus/COVID-19: Hospitalization, self-quarantine, death, physical illness; and total number of the above family events | |
| 2w_family_events_qu | ||
| 2w_family_events_di | ||
| 2w_family_events_il | ||
| 2w_family_events_to | ||
| Mood state | 3m_general_worry 2w_general_worry | How worried the child generally was, 3 months ago and over the past 2 weeks, respectively |
| 3m_sadness 2w_sadness | How happy versus sad the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_anxiety 2w_anxiety | How relaxed versus anxious the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_restlessness 2w_restlessness | How fidgety or restless the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_anhedonia 2w_anhedonia | Ability of the child to enjoy his/her usual activities, 3 months ago and over the past 2 weeks, respectively | |
| 3m_loneliness 2w_loneliness | How lonely the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_irritability 2w_irritability | How irritable or easily angered the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_concentration 2w_concentration | How well the child was able to concentrate or focus, 3 months ago and over the past 2 weeks, respectively | |
| 3m_tiredness 2w_tiredness | How fatigued or tired the child was, 3 months ago and over the past 2 weeks, respectively | |
| 3m_rumination 2w_rumination | How often the child was expressing negative thoughts, 3 months ago and over the past 2 weeks, respectively |
| Classifier | Description |
|---|---|
| Random Forest | An extended version of a decision tree that predicts the future instances with multiple classifiers, rather than a single classifier, to reach an accurate and correct prediction. RF constructs a large number of decision trees. Each decision tree denotes a class prediction, and the class with the most votes represents the model’s prediction [56]. |
| Multi-Layer Perceptron | MLP belongs in the category of Artificial Neural Networks (ANN) and it is the most common neural network. MLP is based on a supervised training procedure to generate a nonlinear model for prediction. It consists of layers, such as the input layer, output layer, and hidden layers. Thus, MLP is a layered feedforward neural network where the information is transferred unidirectionally from the input layer to the output layer through the hidden layers [29]. |
| Extreme Gradient Boosting | XG Boost is an extendible and cutting-edge application of gradient-boosting machines. Gradient boosting is an algorithm in which new models are created to predict the residuals of prior models, and then added together to make the final prediction. It uses a gradient descent algorithm to minimize the loss when adding new models [57]. |
| Logistic Regression | A mathematical model that describes the relationship of data to a dichotomous dependent variable. The model is based on the logistic function, where x ∈ (−∞, +∞) and 0 ≤ f(x) ≤ 1. Thus, regardless the value of x the model is designed to describe the data with a probability in the range of 0 and 1 in a A-shaped graph [58]. |
| Support Vector Machine | SVM is a supervised learning model based on the statistical learning framework, called VC theory. SVM targets to create a decision boundary, the hyperplane, between two classes, which enables the prediction of labels from one or more feature vectors, such that the distance between the closest points of each class, called support vectors, and the hyperplane to be maximized [59]. |
| K-Nearest Neighbor | KNN is a non-parametric classification method that tries to classify an unknown sample based on the known classification of its neighbors [60]. |
| Decision Trees | DTs are sequential models, which logically combine a sequence of simple tests. Each test compares a numeric attribute against a threshold value or a nominal attribute against a set of possible values [61]. |
| Clustering Method | Parameter Settings |
|---|---|
| Mini Batch K-Means | 3 classes |
| Spectral Clustering | 3 classes, arpack eigen solver, nearest_neighbors affinity |
| Ward’s Hierarchical Agglomerative Clustering | 3 classes, ward linkage, symmetric connectivity |
| Average Linkage | 3 classes, average linkage, cityblock affinity, symmetric connectivity |
| Birch | 3 classes |
| Jenks | 3 classes, include lowest value |
| Classification Model | Hyper Parameters Tuning |
|---|---|
| Random Forest | n_estimators = [int(x) for x in np.linspace(start = 10, stop = 500, num = 10)]; max_features = [‘auto’, ‘sqrt’]; max_depth = [int(x) for x in np.linspace(3, 10, num = 1)]; min_samples_split = [3, 4, 5, 6, 7, 10]; min_samples_leaf = [1, 2, 4]; bootstrap = [True, False]. |
| Multi-Layer Perceptron | hidden_layer_sizes = [(2, 5, 10), (5, 10, 20), (10, 20, 50)]; activation = [‘tanh’, ‘relu’]; solver = [‘sgd’, ‘adam’]; alpha = [0.0001, 0.05]; learning_rate = [‘constant’, ‘adaptive’] |
| XG Boost | max_depth = [2, 3, 4, 5, 6, 7, 8]; min_child_weight = [1, 2, 3, 4, 5, 6]; gamma = [0, 0.4, 0.5, 0.6] |
| Logistic Regression | C = [0.001, 0.01, 0.1, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10]; warm_star = [True, False]; multi_class = [‘ovr’, ‘multinomial’]; solver = [‘newton-cg’, ‘lbfgs’, ‘sag’, ‘saga’] |
| Support Vector Machine | C = [0.001, 0.01, 0.1, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10]; kernel = [‘linear’, ‘sigmoid’, ‘rbf’, ‘poly’] |
| K-Nearest Neighbor | n_neighbors = [5, 7, 9, 12, 14, 15, 16, 17]; leaf_size = [1, 2, 3, 5]; weights = [‘uniform’, ‘distance’]; algorithm = [‘auto’, ‘ball_tree’, ‘kd_tree’, ‘brute’] |
| Decision Trees | max_features = [‘auto’, ‘sqrt’, ‘log2’]; min_samples_split = [2, 3, 4, 5, 6, 7, 8, 10, 12, 15]; min_samples_leaf = [1, 2, 3, 4, 5, 6, 7, 8, 10] |
| Clustering Methods | Cluster Information | Clusters | ||
|---|---|---|---|---|
| Cluster 0 | Cluster 1 | Cluster 2 | ||
| Mini Batch K-Means | Set | [−24, −4] | [−3, 4] | [5, 25] |
| Number of elements | 144 | 468 | 132 | |
| Spectral Clustering | Set | Unable to create continuous sets | ||
| Number of elements | 485 | 230 | 29 | |
| Ward | Set | [−24, −7] | [−6, 1] | [2, 25] |
| Number of elements | 66 | 418 | 260 | |
| Average Linkage | Set | [−24, −7] | [−6, 4] | [5, 25] |
| Number of elements | 66 | 546 | 132 | |
| Birch | Set | [−24, −6] | [−5, 8] | [9, 25] |
| Number of elements | 80 | 608 | 56 | |
| Jenks | Set | [−24, −5] | [−4, 3] | [4, 25] |
| Number of elements | 106 | 469 | 169 | |
| Clustering Method | Evaluation Method | Cumulative Normalized Score | ||
|---|---|---|---|---|
| Silhouette Coefficient | Calinski–Harabasz Index | Davies–Bouldin Index | ||
| Mini Batch K-Means | 0.55 | 1106.78 | 0.60 | 2.94 |
| Spectral Clustering | 0.12 | 24.95 | 14.79 | 0.00 |
| Ward | 0.54 | 989.18 | 0.58 | 2.80 |
| Average Linkage | 0.57 | 1048.06 | 0.52 | 2.94 |
| Birch | 0.55 | 784.60 | 0.49 | 2.64 |
| Jenks | 0.56 | 1112.73 | 0.58 | 2.96 |
| Features | Category | Features | Category |
|---|---|---|---|
| 1st feature | Social life | 21st feature | Daily activities |
| 2nd feature | Behavioral effects | 22nd feature | Behavioral effects |
| 3rd feature | Medical diagnosis/rehabilitation | 23rd feature | Behavioral effects |
| 4th feature | Social life | 24th feature | Social life |
| 5th feature | Personal life | 25th feature | Daily activities |
| 6th feature | Medical diagnosis/rehabilitation | 26th feature | Daily activities |
| 7th feature | Demographics | 27th feature | Medical diagnosis/rehabilitation |
| 8th feature | Family life | 28th feature | Demographics |
| 9th feature | Family life | 29th feature | Behavioral effects |
| 10th feature | Social life | 30th feature | Health concerns |
| 11th feature | Social life | 31st feature | Sleeping habits |
| 12th feature | Daily activities | 32nd feature | Social life |
| 13th feature | Daily activities | 33rd feature | Demographics |
| 14th feature | Health concerns | 34th feature | Social life |
| 15th feature | Daily activities | 35th feature | Medical diagnosis/rehabilitation |
| 16th feature | Health concerns | 36th feature | Social life |
| 17th feature | Demographics | 37th feature | Sleeping habits |
| 18th feature | Behavioral effects | 38th feature | Sleeping habits |
| 19th feature | Social life | 39th feature | Sleeping habits |
| 20th feature | Health concerns | 40th feature | Demographics |
| Models | Maximum Accuracy (%) | Number of Features for Maximum Accuracy |
|---|---|---|
| Random Forest | 66.60 | 44 |
| MLP | 57.73 | 58 |
| XG Boost | 69.47 | 40 |
| Logistic Regression | 55.44 | 50 |
| SVM | 64.05 | 49 |
| KNN | 51.28 | 3 |
| Decision Trees | 53.23 | 5 |
| Models | Log-Loss | Accuracy (%) |
|---|---|---|
| XG Boost | 1.195 | 69.47 |
| XG Boost + Isotonic | 0.513 | 72.03 |
| XG Boost + Platt | 0.489 | 76.52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ntakolia, C.; Priftis, D.; Charakopoulou-Travlou, M.; Rannou, I.; Magklara, K.; Giannopoulou, I.; Kotsis, K.; Serdari, A.; Tsalamanios, E.; Grigoriadou, A.; et al. An Explainable Machine Learning Approach for COVID-19’s Impact on Mood States of Children and Adolescents during the First Lockdown in Greece. Healthcare 2022, 10, 149. https://doi.org/10.3390/healthcare10010149
Ntakolia C, Priftis D, Charakopoulou-Travlou M, Rannou I, Magklara K, Giannopoulou I, Kotsis K, Serdari A, Tsalamanios E, Grigoriadou A, et al. An Explainable Machine Learning Approach for COVID-19’s Impact on Mood States of Children and Adolescents during the First Lockdown in Greece. Healthcare. 2022; 10(1):149. https://doi.org/10.3390/healthcare10010149
Chicago/Turabian StyleNtakolia, Charis, Dimitrios Priftis, Mariana Charakopoulou-Travlou, Ioanna Rannou, Konstantina Magklara, Ioanna Giannopoulou, Konstantinos Kotsis, Aspasia Serdari, Emmanouil Tsalamanios, Aliki Grigoriadou, and et al. 2022. "An Explainable Machine Learning Approach for COVID-19’s Impact on Mood States of Children and Adolescents during the First Lockdown in Greece" Healthcare 10, no. 1: 149. https://doi.org/10.3390/healthcare10010149