Abstract
Background: At the start of the COVID-19 pandemic we introduced a Virtual Fracture Clinic (VFC) in our orthopaedic department in which clinical records and imaging were reviewed by an orthopaedic consultant and physiotherapist / nurse without the patient being physically present. All patients received a copy of the clinic note outlining an agreed management plan. VFC’s have been successfully trailed in other orthopaedic departments, however, no study has reported on the process of setting up a VFC during a pandemic, nor the frequency and types of injuries seen in the clinic.
Objectives: The aims were to document and report the frequency and types of injuries reviewed in VFC and to determine the impact in terms of efficiency (frequency of decreased face to face contacts, cost avoidances), clinical governance and effectiveness (SOS contacts, complaints and adverse effects).
Method: We recorded the type of injury, discharge data, face to face urgent and non-urgent fracture clinic consultations, patients admitted for surgery, SOS queries and any complaints for all patients reviewed in VFC between March -September 2020, we also documented the perceived benefits and less positive features for this new way of working.
Results: In the first 7 months the overall rate of discharge was 2021/3035 patients (66%). Of these 49/3035 (2%) re-contacted under an SOS code with on-going or new problems. There were no formal complaints about the VFC during the study period. 973 patients (31%) were reviewed in the general fracture clinic or subspecialty clinics. Only 41 patients (1.5 %) presenting to the VFC required admission for surgery. The re-design resulted in substantial annual cost avoidance of around £129,000. There were over 100 different types of injuries reviewed.
Conclusion: Our redesigned clinic during the COVID-19 pandemic has proved to be an efficient and safe method to manage fracture patients. It also provides substantial cost savings. Whilst we have not identified any concerns in relation to safety from this way of working, future studies are still needed (and on-going) to add to the growing body of evidence in relation to the VFC model in the longer term.
Introduction
The COVID-19 pandemic has caused delivery of orthopaedic services to require extra consideration and substantial revision. Alternative ways to manage patients with urgent injuries have been instigated to minimize patient’s exposure to the disease, spread within the hospital system and reduce the overall impact on stretched resources.
Following the British Orthopaedic Association guidelines [1] a series of changes were made to our standard clinical pathway. The emphasis was to manage patients with non-operative strategies and minimize outpatient visits using augmented reality methods and a “Virtual Fracture Clinic” model (VFC).
Literature Review
Prior to pathway adjustment we conducted a review of the literature to determine the current evidence in relation to the designs, efficiency and effectiveness of virtual fracture clinics. We searched the following databases Medline, Embase and Google Scholar using the search criteria shown in Table 1.
| Criteria | Results |
|---|---|
| (fracture* adj5 clinic*).ti,ab. | 8495 |
| exp Telemedicine/ | 28004 |
| exp Telerehabilitation/ or exp Remote Consultation/ | 5108 |
| virtual.ti. | 15705 |
| 2 or 3 or 4 | 43175 |
| 1 and 5 | 33 |
Table 1: Search criteria and results for a literature review of virtual fracture clinics.
No restrictions were placed on the type of papers to be included in the review compensating for the paucity of literature on virtual fracture clinics. All reviews, reports, guidelines and clinical trials that contained details regarding virtual fracture clinics were included. Papers that included hip fractures and outpatient clinics were excluded. Thirty-three papers were included in the final review. The literature could be grouped according to design/ efficiency of VFC and effectiveness/safety. The former is described first.
Virtual Fracture Clinics are not new and were initially pioneered and introduced in the UK by the Glasgow Royal Infirmary group in 2011 [2]. The Glasgow model includes the immediate discharge of 7 “simple” fractures from the Emergency Department (ED). All other fractures are reviewed in a consultant led Multi-Disciplinary Team (MDT) VFC. In the Glasgow model the patients’ history from the ED notes and x-rays are reviewed and the orthopaedic consultant decides on one of three management outcomes for the patient 1) discharged via phone call from a specialist nurse 2) follow up in nurse lead fracture clinic 3) follow up in a specialist clinic. The Glasgow team reported that this model and way of working dramatically improved the efficiency of their service with a 60% discharge rate from ED and VFC. This resulted in a decrease in the number of face-face reviews, use of staff resources and overall costs.
Since the introduction and publication of the Glasgow model 53 other centers throughout the UK have set up a VFC [2] and several have reported similar results in terms of efficiency and cost-effectiveness [3-11].
In terms of effectiveness and safety the literature is less comprehensive. The review found that 16 studies have investigated the safe and effective discharge of 10 injuries from VFC. These injuries include; 5th metatarsal fractures [4,12-14]; radial head fractures [4,15]; torus fractures [16-20]; children’s clavicle fractures [16-18,21], stable forearm fractures in children [22]; 5th metacarpal [4,23] proximal humeral fractures in adults [24]; clavicle fractures in adults [25,26]; weber B ankle fractures [17,27,28]; and Achilles ruptures [29]. No study has reported the frequency of specific fracture types seen or described the variety of the different fractures managed in the VFC. This information would be useful in terms of prioritizing protocols for the most common and pressing fracture types. To date the studies on safety do not appear to cover all the potential fractures that are likely to be seen in a VFC.
Aim and Objectives
The aim of this study was to determine the impact of a redesigned COVID-19 fracture clinic service on patients and institution in terms of efficiency, clinical governance and effectiveness. In addition, a qualitative evaluation of positive and negative aspects of the new pathway between March 2020 and September 2020 at a single institution was conducted.
Specific objectives were to evaluate and report:
1) Efficiency: Report of the frequency (decreased) of face-to-face contacts in fracture clinic including consideration of patients returning to clinic with further problems (SOS). These findings were compared and bench marked against existing VFC models in the UK.
2) Costs: Compare the cost-of-service delivery of treating patients using the new COVID-19 urgent orthopaedic service (VFC) to the costs of the service pre-Covid-19.
3) Report the incidence of the different types of fractures and pattern of referral to VFC to help guide future decision making in relation to the monitoring governance and developing protocols.
4) Identification and discussion of the positive & negatives of the new pathway.
Material and Methods
The historic clinical pathway
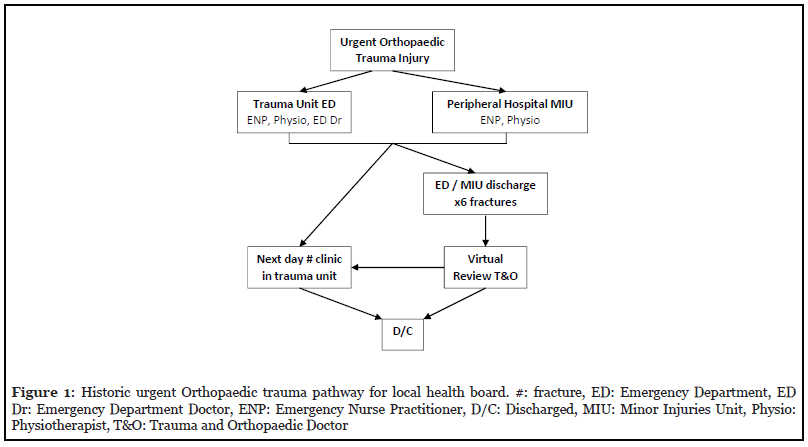
The historic way of working was mapped out (Figure 1). The Pre COVID-19 care pathway process consisted of patients with 6 “simple fractures” (mallet finger, 5th metatarsal fractures, 5th metacarpal neck fractures, pediatric clavicle fractures, torus/buckle distal radius fractures, radial head / neck fractures) being discharged from ED with written advice, their x-rays were then reviewed the next day by an orthopaedic consultant to check the diagnosis was correct in ED. All other patients with fractures were referred to the next working day fracture clinic for a faceface consultation with an orthopaedic doctor (consultant, orthopaedic associate or orthopaedic surgery trainee).
Redesign clinical pathway for COVID-19
The pathway was redesigned to account for the British Orthopaedic Association (BOA) COVID -19 guidelines and the likely resources available following the reconfiguration of parts of the hospital to deal with the pandemic. The fracture clinic space at the acute hospital was converted into an intensive care unit resulting in the redeployment of all fracture clinic and minor injuries staff to a different hospital.
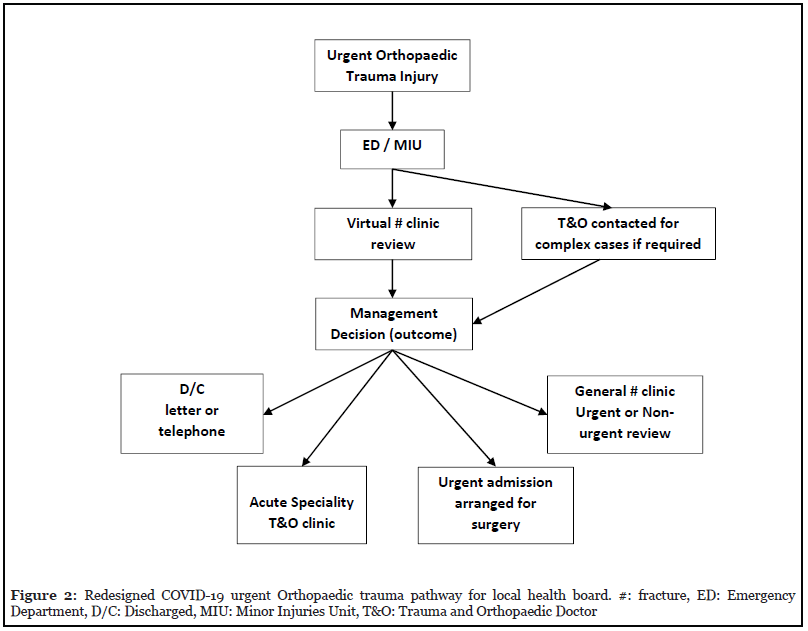
The new process comprised of 3 main components. Enhanced orthopaedic support in MIU and ED particularly at the start of COVID-19 pandemic in March. This enhanced support enabled a definitive management plan including the possibility of discharge of the patient. Patients with the stable self-limiting fractures (as listed above “simple 6 fractures”) were given an advice sheet, discharged from ED and the case was reviewed in VFC to check the diagnosis was correct. All other fractures that did not require immediate admission were referred to the VFC.
The VFC is a multidisciplinary team (MDT) run clinic, the personnel include an orthopaedic consultant, a physiotherapist or nurse and a clerical worker. All patients’ notes (usually a completed proformas, an example of a hand proforma can be seen in appendix one) and x-rays are reviewed within three days of the patient being referred. The clinicians agree the management plan and all patients receive a copy of the clinic note outlining this plan. There are five possible management options for the patient;
1. Discharge via telephone advice or written letter advice
2. An urgent review (same day or next day)
3. Non urgent review (week or so later) in the consultant led general fracture clinic
4. A review in a sub-specialty clinic (pediatrics, hands, shoulders, knees, hips and foot & ankle)
5. Admission for surgery.
All patients are given contact details so that they can contact the clinic if they have any concerns or queries, all calls and queries are recorded as SOS contacts. See Figure 2 for a summary flow chart of the re designed pathway.
Where possible patients were placed in casts or supports which they were asked to remove themselves at home at the appropriate time. Due to the pandemic limited rehabilitation services were available, so the use of written information, web-based information (Brighton and Sussex virtual fracture clinic plans) [30] and physiotherapy telephone consultations (physio direct) were maximized.
Evaluation of the service redesign
Outcome measurements: The following measures were collected prospectively from patient’s records between March 2020 and the end of September 2020.
1) Efficiency: we recorded the number of discharges from ED and VFC, face to face urgent and non-urgent fracture clinic consultations, patients admitted for surgery, SOS queries and any complaints.
2) Costs: we calculated the unit cost per patient in the old and new system.
3) A record of each patient’s injury was recorded on a detailed database.
Statistical analysis
All data was analyzed using Statistical Package for Social Sciences (SPSS) Version 21 (SPSS Inc., Chicago, Illinois).
1) All data in relation to number of discharges; face to face consultation’s, SOS’s; complaints; and operations were collated as frequencies. To bench mark our service they were compared to the Glasgow results.
2) The financial impact of the pathway was analyzed using an elementary health economics evaluation; comparison was made of the costs per patient if they had been seen in the historic system to the cost per patient in the new VFC.
3) A content analysis of themes evident in relation to fracture types is described.
Results
In the first 7 months the overall rate of discharge from ED and VFC was 2021 of 3035 patients (66%). Of these 49/3035 (2%) re-contacted under an SOS code with ongoing or new problems. There were no formal complaints about the VFC during the study period. 973 patients (31%) were reviewed in the general fracture clinic or subspecialty clinics. Only 41 patients (1.5 %) presenting to the VFC required admission for surgery. Figure 3 demonstrates the pathway and numbers of the patients through the redesign. The cost of reviewing these patients in a consultant led fracture clinic would have been £36.61 per patient. Under the redesign the overall cost was £3.67 per patient leading to a total cost avoidance of £75,280.51 for the study period. Which equates to a potential annual cost avoidance of £129,052.
There were 3035 patients reviewed in this study period. The majority of injuries seen in the VFC were adult wrist and hands injuries 956/3053 (31%), followed by pediatrics 752/3053 (25%) and then adult foot and ankle patients 728/3053 (24%). A detailed breakdown based on anatomical region in adults can be seen in Tables 1-3.
| TOTAL | 2351 (adult injuries) | % of total | |
|---|---|---|---|
| Upper Limb | 1413 | 60% | |
| Shoulder | 303 | 13 % | |
| ACJ | 21 | ||
| Clavicle | 70 | ||
| Dislocation | 63 | ||
| Prox humerus | 83 | ||
| Hum Shaft | 9 | ||
| Soft Tissue | 47 | ||
| Scapula | 10 | ||
| Elbow | 147 | 6 % | |
| Radial Head / neck | 72 | ||
| Soft Tissue | 52 | ||
| Supracondylar | 6 | ||
| Olecranon | 5 | ||
| Distal humerus | 12 | ||
| Forearm | All | 7 | 0.3 % |
| Wrist & Hand | 956 | 41 % | |
| Distal radius displaced | 64 | ||
| Distal radius MUA | 61 | ||
| Distal Radius un-displaced | 147 | ||
| Carpals | 31 | ||
| Mallet | 36 | ||
| Metacarpal | 158 | ||
| Phalangeal | 153 | ||
| Scaphoid | 30 | ||
| Scaphoid | 89 | ||
| Soft tissue | 151 | ||
| Thumb | 17 | ||
| Buckle | 6 | ||
| Dislocation | 13 |
Table 2: Frequency of anatomical regions/type of injury seen in VFC: Upper Limb adults.
| TOTAL | 2351 (adult injuries) | ||
|---|---|---|---|
| Lower Limb | 929 | 39 % | |
| Hip | 32 | 1 % | |
| Pubic rami | 14 | ||
| Soft tissue | 7 | ||
| NOF | 5 | ||
| Stress Fracture | 2 | ||
| Peri-prosthetic | 2 | ||
| Prosthetic | 2 | ||
| Knee | 149 | 6 % | |
| PFJ dislocation | 14 | ||
| Patella | 7 | ||
| Femoral condyle avulsion | 2 | ||
| Soft Tissue | 110 | ||
| Tibia Plateau | 11 | ||
| Red Flag swelling | 5 | ||
| Ankle | 290 | 12 % | |
| Achilles | 12 | ||
| Weber A | 90 | ||
| Weber B | 51 | ||
| Weber C | 11 | ||
| Soft tissue | 98 | ||
| Syndesmosis | 6 | ||
| Malleolus | 22 | ||
| Foot | 438 | 19% | |
| Calcaneus | 17 | ||
| Hallux | 64 | ||
| Phalanx | 43 | ||
| Soft Tissue | 99 | ||
| 5th MT un-displaced | 108 | ||
| Metatarsal | 39 | ||
| Tarsal | 16 | ||
| Talus / calcaneus avulsions | 27 | ||
| Talus | 3 | ||
| Stress | 9 | ||
| Toe dislocation | 3 | ||
| Sesamoid | 1 | ||
| Lisfranc | 3 | ||
| Other | 6 | ||
| Shin | 20 | ||
| All | 20 | 1 % |
Table 3: Frequency of anatomical regions/type of injury seen in VFC: Lower Limb adults.
| Spine | 9 (adult injuries) | 0.5% | |
|---|---|---|---|
| OA | 2 | ||
| Syndesmophyte | 1 | ||
| Wedge L | 3 | ||
| Wedge T | 3 |
Table 4:Frequency of anatomical regions/type of injury seen in VFC: Spine adults.
Discussion
The COVID-19 pandemic forced a rapid and evolving redesign of the fracture management service at our institution with a VFC introduced, to reduce the number of face-to-face consultations for orthopaedic injuries ordinarily referred to the fracture clinic. The aim of this study was to capture the impact of this redesigned COVID-19 fracture clinic service on patient satisfaction, efficiency, safety and effectiveness. In addition, a qualitative comment (reflective evaluation) is included in this discussion that outlines the positive and negative aspects of the new pathway.
The clinic was set up based on the Glasgow model [2] with some modifications. The modification included having orthopaedic specialist support (an orthopaedic doctor) in ED / MIU to help the nurses and ED staff make a definitive decision on the patient management from the front door. Furthermore, when patients were required to attend for a face: face consultation in a general fracture clinic they were reviewed by a doctor rather than a nurse, since our nurses were not trained and therefore did not have the expertise to run the general fracture clinic. Most patients were discharged using a letter detailing to them what to do rather than a telephone call. It is thought that this contributed to a reduction in SOS calls and there were no formal complaints. However, future studies investigating patient satisfaction in relation to communication method (letter versus telephone consultation) are required.
The flow of our patients was very similar to that reported by the Glasgow team and provides us with a more efficient and cost-effective way of working. In our historic pathway model 2,511 patients would have been seen in next day fracture clinics (3035 total patients – 524 “simple 6” patients). However, with the redesigned pathway of 3035 patients, 2021 (66%) were discharged and 973 patients (32%) were brought back to clinic for a review. Only 41 patients (1.5 %) of our patients required admission for surgery. The Glasgow team reported 60 % of patients were discharged from ED / VFC, 39 % were brought back for clinic reviews and 1 % were admitted for surgery.
The costs of the new versus the old system were calculated based upon a consultant led service. We received guidance from the health boards finance department. The total cost of the consultant lead face to face appointment was estimated at £36.61 per patient, this comprised of consultant cost plus non-consultant clinic costs (nurse, plasters, supports, and radiology). The total cost per VFC patient was estimated at £3.67 per patient. This resulted in a cost saving for the study period of £75,280 equating to £129,000 per annum. This is comparable to the cost saving reported in Glasgow of £98,868-£156,171.
If SOS calls are considered a valid metric for potential threat then the results of this study indicate that, at least in the short term, this is a safe way of delivering orthopaedic trauma care for relatively minor injuries with only 52/3035 (2%) of patients contacting with problems (SOS). No patients submitted a formal or informal complaint. Any SOS reported was reviewed and changes in care implemented when necessary. In most cases SOS calls were patients enquiring about pathway concerns and self-management rather than serious clinical issues. To address this a frequently asked questions sheet for ED and MIU was produced.
A limitation to this study is the lack of long-term outcome for involved patients. This is particularly important in relation to the governance of the 66 % of patients who were advised on self-management plans and discharged. A positive aspect is the generalization and variety of fractures examined. Over 100 different types of fractures / injuries were reviewed in our VFC despite a literature search showing that only 10 fractures that have been investigated for the effectiveness of outcome using a VFC. Investigation of the outcome of our patients at 6 months’ post injury is now a priority. We then hope to be able to construct and disseminate a clinical decision-making algorithm to reduce the frequency of inappropriate referrals to VFC and to further improve the management of patients with minor injuries, thereby increase the cost savings to the hospital and the patient the cost of unnecessary visits.
Positive features of the redesign
This redesign has provided an efficient way of working, requiring less manpower, time and resulting in overall costs savings. From the patients’ perspective, it reduces an additional next day attendance at the hospital at a time when they are likely to be suffering discomfort and pain. The VFC MDT enhanced the physiotherapist; nurse, administrative staff and orthopaedic consultants working relationships. It also resulted in increased knowledge and expertise by all. The pressure of COVID-19 meant that the VFC was set up with immediate effects, without the “tsunami” of planning meetings that would have been required pre COVID-19.
Negative features of the redesign
Trainees are not currently part of the formal VFC team due to COVID rotas, however we feel this would be a valuable educational environment as man power constraints are lifted as the pandemic eases.
Barriers to implementation
Initially some of the consultants were hesitant about working virtually. Some expressed a level of discomfort around “treating x-rays and not patients”. However, ED and MIU staff completed standardized proformas to document their clinical findings which helped to reduce their anxiety around this area.
We identified variations in practice between consultants in terms of average speed of reviewing each patient case (range 2.5 - 6.5 minutes per patient) and the number of patients being discharged (range 50-85%). These differences were thought to be due to the different levels of experience of the consultants and lack of evidence to direct consistency in practice. We hope our future studies will help produce evidence-based protocols to standardize approach and reduce these variations in care.
As a result of the COVID-19 pandemic the service was set up rapidly with little time for planning. There were some communication problems between staff as a result of this with some staff being unaware of the new approach. To improve the communication and receive feedback effectively weekly meetings were organized with the leads of each of the teams / departments who were considered key stakeholders; namely fracture clinic sisters, orthopaedic managers, physiotherapists, radiology staff, ED and MIU staff.
ED and MIU notes need to be electronically typed via a proforma to ensure eligibility of notes as well as comprehensive assessments and an automated database for analysis of the service is also required to avoid excess and expensive manpower for data entry.
To help patients take responsibility for their injury we have had to maximize the use of written and digital information, often using the resources that have been produced by other health boards.
Conclusion
Our redesigned clinic during the COVID-19 pandemic has proved to be an efficient way of working and provides substantial cost savings. Whilst we have not identified any concerns in relation to safety from this way of working. Futures studies are on-going to add to the growing body of evidence in relation to the governance for this system of working in the long term.
Acknowledgements
All orthopaedic consultants at Swansea Bay University Health Board as well as the nursing and administrative staff in the fracture clinic are thanked for their on-going support, help and advice with this transformation. The doctors, nurses, radiology and administrative staff in MIU and ED are also thanked for their willingness to support change during this unprecedented time. Dr Matthew Jones ED consultant and Mr Kevin Randall Consultant Nurse are acknowledged for their input with the development of the MIU and ED proformas. The Orthopaedic Secretaries and Mr Ali Mofidi orthopaedic consultant are thanked for their support with data entry. The orthopaedic service managers are thanked for their support with securing clinic space and logistics. The librarians are thanked for their support with the literature review.
Declaration of Interest
Nothing to declare
Ethical Approval
Ethical approval was not required for this project, as this was classed as an improvement project and no datasets were collected beyond routine.
References
2. Vardy J, Jenkins PJ, Clark K, Chekroud M, Begbie K, Anthony I, et al. Effect of a redesigned fracture management pathway and ‘virtual’fracture clinic on ED performance. BMJ Open. 2014 Jun 1;4(6).
3. Jenkins PJ, Morton A, Anderson G, Van Der Meer RB, Rymaszewski LA. Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care. Bone & Joint Research. 2016 Feb;5(2):33-6.
4. Mackenzie SP, Carter TH, Jefferies JG, Wilby JB, Hall P, Duckworth AD, et al. Discharged but not dissatisfied:outcomes and satisfaction of patients discharged from the Edinburgh Trauma Triage Clinic. Bone & Joint Journal. 2018 Jul;100(7):959-65.
5. McGill A, North J. An analysis of an ongoing trial of rural videoconference fracture clinics. Journal of Telemedicine and Telecare. 2012 Dec;18(8):470-2.
6. Palombo A, Ferguson J, Rowlands A, Pedley D, Fraser S. An evaluation of a telemedicine fracture review clinic.. Journal of Telemedicine and Telecare. 2003;9 Suppl 1:S31-3.
7. Ricci WM, Borrelli J. Teleradiology in orthopaedic surgery: impact on clinical decision making for acute fracture management. Journal of Orthopaedic Trauma. 2002 Jan 1;16(1):1-6.
8. Beiri A, Alani A, Ibrahim T, Taylor GJ. Trauma rapid review process: efficient out-patient fracture management. The Annals of The Royal College of Surgeons of England. 2006 Jul;88(4):408-11.
9. Murray O, Christen K, Marsh A, Bayer J. Fracture clinic redesign: improving standards in patient care and interprofessional education. Swiss Medical Weekly. 2012 Jul 26;142(2930).
10. Evans D, Hardman J, Middleton SD, Anakwe RE. Developing a virtual fracture clinic for hand and wrist injuries. Journal of Hand Surgery (European Volume). 2018 Oct;43(8):893-4.
11. White TO, Mackenzie SP, Carter TH, Jefferies JG, Prescott OR, Duckworth AD, Keating JF. The evolution of fracture clinic design: the activity and safety of the Edinburgh Trauma Triage Clinic, with one-year follow-up. The Bone & Joint Journal. 2017 Apr;99(4):503-7.
12. Egol K, Walsh M, Rosenblatt K, Capla E, Koval KJ. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot & Ankle International. 2007 May;28(5):581-3.
13. Brogan K, Bellringer S, Akehurst H, Gee C, Ibrahim N, Cassidy L, et al. Virtual fracture clinic management of fifth metatarsal, including Jones’, fractures is safe and costeffective. Injury. 2017 Apr 1;48(4):966-70.
14. Cakir H, Van Vliet-Koppert ST, Van Lieshout EM, De Vries MR, Van Der Elst M, Schepers T. Demographics and outcome of metatarsal fractures. Archives of Orthopaedic and Trauma Surgery. 2011 Feb 1;131(2):241-5.
15. Jayaram PR, Bhattacharyya R, Jenkins PJ, Anthony I, Rymaszewski LA. A new “virtual” patient pathway for the management of radial head and neck fractures. Journal of Shoulder and Elbow Surgery. 2014 Mar 1;23(3):297-301.
16. Roy SK, McDonald N, Back D. Can the introduction of a “virtual” clinic in a paediatric tertiary centre help to reduce the burden of followup for minor paediatric fractures?. Emergency Medicine Journal. 2016 Dec 1;33(12):934-5.
17. Carroll P. Vitual fracture clinic in a paediatric population: What is the evidence? Irish Journal of Medical Science. 2017;186(2 supplement 1):S109.
18. Robinson PM, Sim F, Latimer M, Mitchell PD. Paediatric fracture clinic re-design: Incorporating a virtual fracture clinic. Injury. 2017 Oct 1;48(10):2101-5.
19. Symons S, Rowsell M, Bhowal B, Dias JJ. Hospital versus home management of children with buckle fractures of the distal radius: a prospective, randomised trial. The Journal of bone and joint surgery. British Volume. 2001 May;83(4):556-60.
20. Seewoonarain S, Babu S, Sangoi D, Avasthi A, Ricketts D. Introducing a Virtual Fracture Clinic Increases Efficiency and Reduces Costs in Torus Fracture Management. Pediatric Quality & Safety. 2019 Nov;4(6).
21. Calder JD, Solan M, Gidwani S, Allen S, Ricketts DM. Management of paediatric clavicle fractures--is followup necessary? An audit of 346 cases. Annals of the Royal College of Surgeons of England. 2002 Sep;84(5):331-3.
22. Hamilton TW, Hutchings L, Alsousou J, Tutton E, Hodson E, Smith CH, et al. The treatment of stable paediatric forearm fractures using a cast that may be removed at home: comparison with traditional management in a randomised controlled trial. The Bone & Joint Journal. 2013 Dec;95(12):1714-20.
23. Bansal R, Craigen MA. Fifth metacarpal neck fractures: is follow-up required?. Journal of Hand Surgery (European Volume). 2007 Feb;32(1):69-73.
24. To C, Asif S, Chan G, Guryel E. The Virtual Fracture Clinic: A Safe and Cost-Effective Protocol for the Management of Proximal Humeral Fractures. British Journal of Surgery 2019 Sep 1 (Vol. 106, pp. 103-103). 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY.
25. McKerrow M, North J. Clavicle fracture management: A comparison of a tertiary hospital and rural telehealth sites. Journal of Telemedicine and Telecare. 2017 Dec;23(10):856-60.
26. Bhattacharyya R, Jayaram PR, Holliday R, Jenkins P, Anthony I, Rymaszewski L. The virtual fracture clinic:reducing unnecessary review of clavicle fractures. Injury. 2017 Mar 1;48(3):720-3.
27. Martin AG. Weber B ankle fracture: an unnecessary fracture clinic burden. Injury. 2004 Aug 1;35(8):805-8.
28. Bellringer SF, Brogan K, Cassidy L, Gibbs J. Standardised virtual fracture clinic management of radiographically stable Weber B ankle fractures is safe, cost effective and reproducible. Injury. 2017 Jul 1;48(7):1670-3.
29. Robertson A, Godavitarne C, Bellringer S, Guryel E, Auld F, Cassidy L, Gibbs J. Standardised virtual fracture clinic management of Achilles tendon ruptures is safe and reproducible. Foot and Ankle Surgery. 2019 Dec 1;25(6):782-4.
30. Trust BSUH. Virtual Fracture Clinic Care Plans. https://wwwfracturecarecouk/care-plans/. 2017.
