Abstract
Purpose
Spain has been one of the most affected countries by the COVID-19 pandemic, being among the countries with worse numbers, including the death rate. However, most patients are asymptomatic, although they are very contagious. The objective of this study was to investigate the incidence in oncological patients infected with SARS-CoV-2 that are asymptomatic for COVID-19 and at home and that undergo PET/CT for oncologic indications, nonrelated to COVID-19, finding in the PET/CT lung alterations that are suggestive of SARS-CoV-2 infection.
Methods
During the period of maximum incidence of the global pandemic in one of the most affected regions of Spain, there were 145 patients that met inclusion and exclusion criteria and were included in the study. Imaging findings previously described such as ground-glass opacities with low [18F]-FDG uptake were considered images suspicious for SARS-CoV-2 infection. Patients with these findings were referred to RT-PCR testing and close follow-up to confirm the presence or absence of COVID-19.
Results
Suspicious lung imaging findings were present in 7 of 145 patients (4.8%). Five of these 7 patients were confirmed as presenting SARS-CoV-2 infection, this is, COVID-19. In the remaining two, it was not possible to confirm the presence of COVID-19 with RT-PCR, although in one of them, PET/CT allowed an early diagnosis of a lung infection related to a bacterial pneumonic infection that was promptly and adequately treated with antibiotics.
Conclusion
These results confirm that the prevalence of SARS-CoV-2 infection is higher than suspected and that there are asymptomatic patients that are attending imaging departments to be explored for their baseline oncologic processes. In these patients, PET/CT allows an early diagnosis of COVID-19.
Similar content being viewed by others
Introduction
In 3 months, the infection by COVID-19 virus (also named “severe acute respiratory syndrome coronavirus 2” or SARS-CoV-2) has become the first global pandemic of the new millennium. The first cases were reported in Wuhan, the capital of the Chinese province of Hubei, in December 2019 [1]. The World Health Organisation (WHO) declared coronavirus disease-19 (COVID-19) a health emergency at the end of January 2020, spreading quickly to many countries by community transmission, a global pandemic being declared a global pandemic the 11th of March [2]. In Spain, the first case of COVID-19 was confirmed in the Canary Islands the 31st of January, spreading fast to the rest of Spain. The region of Madrid is the one that accumulates a highest number of cases and the region of La Rioja is the one with the highest incidence rate, with over 1500 cases per 100,000 inhabitants. La Rioja region presents 4054 confirmed cases of SARS-CoV-2 infection in a population of 316,798 (January 2020), giving a known prevalence of 12.8/1000 confirmed cases of SARS-CoV-2 in La Rioja region [3].
The diagnosis of the disease has been mainly clinical based on the symptomatology referred by the patients and confirmed by a real-time reverse transcriptase-polymerase chain reaction (RT-PCR) test. A low percentage of patients develop respiratory distress with a fatal outcome in some of them. However, most infected patients remain asymptomatic or present very mild symptoms. It is probably this group of patients that has contributed to the expansion of the disease.
Medical imaging departments, including Nuclear Medicine, have not been unconnected to this disease. As the rest of specialities, patients have continued attending the diagnostic and therapeutic procedures when indicated. This implies that it was to be expected that patients with SARS-CoV-2 infection, although asymptomatic, have attended their appointments without a previous diagnosis of COVID-19. In these patients, the imaging findings of the Nuclear Medicine procedures has provided the diagnosis of COVID-19, as in our previously published case [4].
The aim of this study was to retrospectively analyse the incidence of suspicious imaging findings of COVID-19 in PET/CT performed in asymptomatic patients referred to our Department with oncologic indications.
Materials and methods
We retrospectively analysed PET/CT studies performed from the day of the first diagnosed COVID-19 patient in La Rioja region, the 2nd of March 2020, to the 22nd of April 2020. Inclusion criteria were the following: (a) outpatients referred to Nuclear Medicine for whole-body PET/CT, (b) with [18F]-FDG or [18F]-fluorocholine, (c) referral was due only to oncologic indications, and (d) patients were asymptomatic for SARS-CoV-2 infection. Exclusion criteria were the following: (a) inpatients, (b) non-oncologic indications, (c) non-whole-body PET/CT, and (d) symptomatic or suspicion of COVID-19. Finally, 145 patients were included.
[18F]-FDG PET/CT and [18F]-fluorocholine PET/CT were performed following the European Association of Nuclear Medicine (EANM) procedure guidelines [5] and Spanish guidelines [6]. The studies were analysed by two nuclear medicine physician experts in PET/CT, independently and consecutively reading the scans and then reaching a consensus, presenting both evaluations 100% concordance. A special emphasis was done on the known lung findings described in asymptomatic patients with SARS-CoV-2 infection [7]. Ground-glass opacities (GGO) have been reported as primary CT findings in COVID-19 [8, 9], whereas pleural effusions and the tree-in-bud sign are atypical in COVID-19, possibly related to complications (pleural effusions) or superadded bacterial infection (tree-in-bud sign) [9, 10]. Also, the grade of radiotracer uptake in these lung lesions was investigated. In the patients in which lung lesions suspicious of COVID-19 were found, the referring physician was contacted and informed that the suspicion should be confirmed with RT-PCR or clinical follow-up.
An independent ethical committee for clinical research (Comité de Ética de Investigación con medicamentos de La Rioja, CEImLar) approved the study design (Ref. CEImLAR P.I. 431) in Spain.
Results
One hundred forty-five patients (50 men, average age 60.8 years, range 21–89) met the inclusion and exclusion criteria and were finally included in the study. The radiotracer used was [18F]-FDG in 132 (91%) patients and [18F]-fluorocholine in 13 (9%) patients. The characteristics of the patients studied are presented in Table 1, including known primary tumours and the oncological indications of the PET/CT.
In 7 patients of the 145 included (4.8%), lung imaging findings suspicious of SARS-CoV-2 infection were found. All 7 patients corresponded to [18F]-FDG PET/CT studies; no [18F]-fluorocholine PET/CT showed imaging findings suspicious of COVID-19. The characteristics of these findings are described in Table 2. Five of the seven patients, all five presenting GGOs, (71.4%) were confirmed by the clinicians as presenting COVID-19, being confirmed as positive for SARS-CoV-2 infection by RT-PCR in 4 (one of them following a single RT-PCR and the other three needed two successive RT-PCR to obtain a positive result). The other one developed a rapidly progressing lung consolidation and died 15 days later, with two RT-PCR tests resulting negative during the short hospitalisation, although the clinical and analytical (high ferritin and inflammation markers) suspicion of COVID-19 was always very high. The remaining two of the seven patients (28.6%) presented imaging findings suspicious of SARS-CoV-2 infection, one of them presented bilateral GGOs and the other presented lung consolidations (suspicious of a more advanced COVID-19) but not GGOs, but confirmation of the disease was not obtained. One of them was diagnosed with a bacterial pneumonia and was treated with antibiotics. In the other one, two RT-PCR tests were negative and after a clinical follow-up of 38 days, the patient remains asymptomatic and with no evidence of SARS-CoV-2 infection.
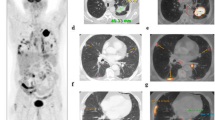
All 7 patients showed lung findings both in CT and [18F]-FDG PET (Table 2). The most frequent finding was multiple GGOs (6 of the 7 patients presented GGOs, the other one presented lung consolidations) that coincided with low [18F]-FDG uptake (Fig. 1). The average SUVmax value of the GGOs was 4.1 (range 2.6–5.2). In most patients, the lung lesions were bilateral (Fig. 2) and the clinical evolution was worse in those with more extensive disease (Fig. 3). The worse evolution related to the extent of the disease is evident when analysing the evolution of the five patients confirmed by the clinicians as presenting COVID-19. As mentioned above, the evolution was fatal in the patient presenting the most extensive disease in the form of rapidly progressing lung consolidation, dying 15 days after the [18F]-FDG PET/CT. With regard to the other four patients confirmed as presenting COVID-19, they only presented GGOs and clinically remained asymptomatic; two of them were hospitalised and the other two were sent home and asked to isolate. One of the two hospitalised patients received hydroxychloroquine and was discharged when the RT-PCR test was negative. The other hospitalised patient did not require treatment. With regard to the two patients sent home after being evaluated by the clinicians following the [18F]-FDG PET/CT incidental findings, they remained isolated at home, one of them being operated of an ovarian cancer after the RT-PCR resulted negative. Figure 4 presents the maximum intensity projections (MIPs) with the same SUV scale of the seven patients that were considered suspicious for SARS-CoV-2 infection based on the PET/CT findings.
A 65-year-old male patient with locally advanced rectal cancer who came for [18F]-FDG PET/CT for initial staging. Axial, sagittal and coronal CT slices (a) and fused [18F]-FDG PET/CT (b) show the most frequent imaging finding in COVID-19 patients; this is GGOs (black arrows) coinciding with an area of intense [18F]-FDG uptake, peripherally localised, with an homogeneous [18F]-FDG uptake
A 72-year-old female patient who was referred for [18F]-FDG PET/CT for initial staging of ovarian cancer. Axial CT (a) and fused [18F]-FDG PET/CT (b) show GGOs coinciding with an area of intense [18F]-FDG uptake in the left lung and a low uptake in the right lung, corresponding to a quickly resolved infiltrate
A 66-year-old female patient with head and neck tumour, referred for [18F]-FDG PET/CT for suspected recurrence. Axial CT (a and b) and fused [18F]-FDG PET/CT (c and d) show extensive disease in both lungs with pleural effusion (broad arrow), hilar infiltrates (arrow heads) and nodules (long arrows). GGOs were also present in this patient but are not included in the image presented
Discussion
The rapid spread of this global pandemic and the urgency in attending patients and initiating treatments in symptomatic patients have made impossible in many cases to do RT-PCR tests of pharyngeal swabs. The difficulties in reaching the diagnosis have been increased by the high rate of false negatives of this technique [11, 12]. These circumstances have contributed to consider the presence of radiological signs in the lung of the patients with a bad evolution as highly suspicious for SARS-CoV-2 infection even with a negative RT-PCR [13].
The limitations in the diagnosis of COVID-19, together with the fact that most of the patients infected with SARS-CoV-2 are asymptomatic or present scarce symptoms, were the reason for initiating this retrospective study analysing patients scanned with PET/CT in which there were suspicious lung findings for SARS-CoV-2 infection. We decided to initiate the revision from the day of the first diagnosed COVID-19 patient in La Rioja region, the 2nd of March 2020, until the 22nd of April 2020. As a preventive measure, from the 2nd of March 2020 onwards, patients were interviewed by telephone the day before the study to confirm the absence of symptoms related to COVID-19. Therefore, our findings are in asymptomatic patients without a previous diagnosis of COVID-19. Regarding the inclusion and exclusion criteria in this study, the aim was to reduce as much as possible the pre-test probability of COVID-19 in the included patients. Inpatients are at a higher risk of infection, especially during the pandemic. On the other hand, we aimed at reducing the presence of confounding findings in the PET/CT that could appear if patients with suspected inflammatory (i.e., sarcoidosis, large vessel vasculitis) or infectious (i.e., suspected infective endocarditis or fever of unknown origin) processes were included. Therefore, only patients with oncologic indications were included in the study.
The design of this study is undoubtedly related to the development of the COVID-19 crisis in those months. On one hand, the normal clinical activity in most hospitals in Spain during the COVID-19 global pandemic was influenced by the unfolding global health crisis and most efforts were dedicated to address this crisis, as also occurred in the rest of European countries with similar levels of incidence by the pandemic. On the other hand, many patients were not willing to attend their scheduled citations because of fear of becoming infected by SARS-CoV-2 when being at the hospital, so some of them cancelled their visit. As mentioned above, in all cases, patients were contacted by phone the day before the imaging procedure to ensure they did not present clinical suspicion of COVID-19, cancelling their citation if there was minimal clinical suspicion of COVID-19. Only those urgent or oncologic patients that referred no clinical suspicion of SARS-CoV-2 infection the day before the procedure were told to come for the PET/CT procedure.
There are few publications on the findings of PET/CT in COVID-19 patients and most of them are in symptomatic patients already diagnosed with COVID-19 [7, 14]. The GGO finding was the most frequent finding in our study, similarly to the study by Qin et al. [7]. Most of our patients presented more than one lobe affected. On the other hand, Setti et al. [15] have recently presented the typical [18F]-FDG PET/CT findings in patients with clinical suspicion of COVID-19 infection, although in the absence of a definitive diagnosis. The population included by Setti et al. work clearly differs from the sample included in our work, in which there was no suspicion of infectious disease. In another case report, Lui et al. [16] report the pattern of lung involvement in a patient with suspected systemic symptoms of COVID-19.
To the best of our knowledge, only seven papers [4, 17,18,19,20,21,22] have been published including patients asymptomatic for SARS-CoV-2 infection, but only one of them [17] is an original study reporting a series of patients, whereas five are case reports or interesting images [4, 18,19,20,21] and one is a letter to the editor [22].
The only published original article in this context is the one by Albano et al. [17], presenting a series of patients with incidental findings suggestive of COVID-19, although this series also includes patients studied with SPECT/CT. In comparison, our series includes a larger number of patients with a slightly lower incidence of the mentioned incidental findings (> 9% versus 4.8% in our series). The different detection rate may be explained based on the large number of patients studied and the exclusion of patients with non-oncologic indications or hospitalised patients in our study, as well as by the differences in incidence and prevalence between both populations.
Polverani et al. [18] published the case report of an asymptomatic patient with lung cancer studied with [18F]-FDG PET/CT as a follow-up study, evidencing as an incidental finding GGOs with diffuse and intense [18F]-FDG uptake located in the lower lobes and predominantly in the periphery, such as those evidenced in our series. Tulchinsky et al. [19] and Castanheira et al. [20] are two more case reports of patients asymptomatic for SARS-CoV-2 infection and later confirmed as COVID-19 positive, the first suspected on a bone SPECT/CT and the second on a [18F]-FDG PET/CT. Zanoni et al. [21] presents an interesting image of [18F]-FDG PET/CT for suspected lymphoma relapse in a patient with concomitant pneumococcal pneumonia during COVID-19 outbreak. [18F]-FDG PET/CT detected an unexpected SARS-Cov-2 co-infection despite double RT-PCR negativity, being confirmed in the third RT-PCR test. They recommend taking precautions in patients’ management even after first RT-PCR negativities because of RT-PCR false negatives. Moreover, they indicate that during COVID-19 pandemic, incidental findings detected by a nuclear medicine physician when reading the lung window CT component of PET/CT studies might be extremely relevant [21].
Finally, Alberts et al. [22] published a letter to the editor commenting previous publications and very briefly including their own experience. They had no findings suggestive of COVID-19 in 562 consecutive patients, indicating that this was probably due to the fact that the prevalence of asymptomatic COVID-19 patients was very low in their area.
The main limitations of our study were the retrospective design and the small study population, although it is representative of the current situation. As another limitation, given the high prevalence of SARS-CoV-2 infection in La Rioja region, these observations might not be extrapolated to other Spanish regions or other countries.
Conclusions
Our results confirm that the prevalence of SARS-CoV-2 infection is higher than the known figures, due to the relevant proportion of asymptomatic patients, some of them with lung disease, which can be diagnosed in a pre-symptomatic phase based on the incidental imaging findings in imaging procedures performed for completely different clinical indications.
Furthermore, the described incidental findings provide an early diagnosis of COVID-19, allowing the application of the most adequate patient management, immediate isolation from non-COVID patients and family, close follow-up and early initiation of treatment if necessary. In this regard, after detecting in PET/CT suspicious findings of SARS-CoV-2 infection, clinical management should include precautions even after first RT-PCR negativities because of RT-PCR false negatives. Moreover, our results underline the fact that when reading the lung window CT component of PET/CT, the nuclear medicine physician should exclude incidental findings suspicious of SARS-CoV-2 infection in all patients, even if asymptomatic, as these incidental findings might induce very significant changes in patient management decisions and in the epidemiologic control of the COVID-19 pandemic.
References
Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Rolling updates on coronavirus disease (COVID-19) www.who.int Last accessed 29 April 2020.
Red Nacional de Vigilancia epidemiológica. Informe sobre la situación del COVID en España. Instituto de Salud Calos III. En: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx Last accessed 29 April 2020.
Boulvard XLE, Romero Robles LG, Garrastachu P, Cabrera Villegas A, Albornoz Almada MC, Colletti PM, et al. [18F]-FDG PET/CT in Hodgkin lymphoma with unsuspected COVID-19. Clin Nucl Med. 2020;45:652–3. https://doi.org/10.1097/RLU.0000000000003143.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imag. 2015;42:328–54. https://doi.org/10.1007/s00259-014-2961-x.
García Garzón JR, Rodríguez Fernández A, Cabrera Villegas A. Procedimientos en medicina nuclear. Tomografía por emisión de positrones de cuerpo completo (PET/TAC) con 18F-fluorodesoxiglucosa. Rev Esp Med Nucl. 2009;28:85–9.
Qin C, Liu F, Yen TC, Lan X. 18F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. Eur J Nucl Med Mol Imaging. 2020;47:1281–6. https://doi.org/10.1007/s00259-020-04734-w.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan. China JAMA. 2020;323:1061–9. https://doi.org/10.1001/jama.2020.1585.
Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–80. https://doi.org/10.1007/s00259-020-04735-9.
Perlman S. Another decade, another coronavirus. N Engl J Med. 2020;382:760–2. https://doi.org/10.1056/NEJMe2001126.
Lan L, Xu D, Ye G, Xia C, Wang S, Li Y, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323:1502–3. https://doi.org/10.1001/jama.2020.2783.
Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med. 2020. j/cclm.ahead-of-print/cclm-2020-0198/cclm-2020-0198.xml. https://doi.org/10.1515/cclm-2020-0198.
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020;295:202–7. https://doi.org/10.1148/radiol.2020200230.
Zou S, Zhu X. FDG PET/CT of COVID-19. Radiology. 2020;6:200770. https://doi.org/10.1148/radiol.2020200770.
Setti L, Kirienko M, Dalto SC, Bonacina M, Bombardieri E. FDG-PET/CT findings highly suspicious for COVID-19 in an Italian case series of asymptomatic patients. Eur J Nucl Med Mol Imaging. 2020;47:1649–56. https://doi.org/10.1007/s00259-020-04819-6.
Liu C, Zhou J, Xia L, Cheng X, Lu D. 18F-FDG PET/CT and serial chest CT findings in a COVID-19 patient with dynamic clinical characteristics in different period. Clin Nucl Med. 2020;45:495–6. https://doi.org/10.1097/RLU.0000000000003068.
Albano D, Bertagna F, Bertolia M, Bosio G, Lucchini S, Motta F. Incidental findings suggestive of COVID-19 in asymptomatic patients undergoing nuclear medicine procedures in a high prevalence region. J Nucl Med. 2020. https://doi.org/10.2967/jnumed.120.246256.
Polverari G, Arena V, Ceci F, Pelosi E, Ianniello A, Poli E, et al. 18F-FDG uptake in asymptomatic SARS-CoV-2 (COVID-19) patient, referred to PET/CT for non-small cells lung cancer restaging. J Thorac Oncol. 2020;15:1078–80. https://doi.org/10.1016/j.jtho.2020.03.022.
Tulchinsky M, Fotos JS, Slonimsky E. Incidental CT findings suspicious for COVID-19-associated pneumonia on nuclear medicine examinations: recognition and management plan. Clin Nucl Med. 2020;45:531–3. https://doi.org/10.1097/RLU.0000000000003100.
Castanheira J, Mascarenhas Gaivão A, Mairos Teixeira S, Pereira PJ, Costa DC. Asymptomatic COVID-19 positive patient suspected on FDG-PET/CT. Nucl Med Commun. 2020;41:598–9. https://doi.org/10.1097/MNM.0000000000001221.
Zanoni L, Mosconi C, Cervati V, Diegoli M, Monteduro F, Golfieri R, et al. [18F]-FDG PET/CT for suspected lymphoma relapse in a patient with concomitant pneumococcal pneumonia during COVID-19 outbreak: unexpected SARS-Cov-2 co-infection despite double RT-PCR negativity. Eur J Nucl Med Mol Imaging. 2020;47:2038–9. https://doi.org/10.1007/s00259-020-04838-3.
Alberts I, Vollnberg B, Sachpekidis C, Mingels C, Weidner S, Afshar-Oromieh A, et al. Incidental SARS-CoV-2-related findings in asymptomatic patients in [18F]-FDG-PET/CT-potential insights. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-020-04869-w.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. An independent ethical committee for clinical research (Comité de Ética de Investigación con medicamentos de La Rioja, CEImLar) approved the study design (Ref. CEImLAR P.I. 431) in Spain.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection and inflammation
Rights and permissions
About this article
Cite this article
Cabrera Villegas, A., Romero Robles, L.G., Boulvard Chollet, X.L.E. et al. [18F]-FDG PET/CT in oncologic patients with unsuspected asymptomatic infection with SARS-CoV-2. Eur J Nucl Med Mol Imaging 48, 786–793 (2021). https://doi.org/10.1007/s00259-020-04979-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04979-5