Abstract
Background
This study was aimed to assess the efficacy and safety of tocilizumab (TCZ) and to investigate the factors related to the progress and mortality of patients with a secondary cytokine release syndrome caused by SARS-CoV-2.
Methods
A retrospective descriptive observational study of hospitalised patients with a positive polymerase chain reaction (PCR) result for SARS-CoV-2 and whose clinical evolution required the administration of one or more doses of TCZ was conducted. Demographic variables, clinical evolution, radiologic progress and analytical parameters were analysed on days 1, 3 and 5 after administration the first dose of TCZ.
Results
A total of 75 patients with a clinical history of Accurate Respiratory Distress Syndrome (ARDS) were analysed, among whom, 19 had mild ARDS (25.3%), 37 moderate ARDS (49.4%) and 19 severe ARDS (25.3%). Lymphocytopenia and high levels of PCR, d-Dimer and IL-6 were observed in almost all the patients (91.8%). Treatment with TCZ was associated with a reduction of lymphocytopenia, C-reactive protein (CRP) levels, severe ARDS cases and fever. Although a better evolution of PaO2/FiO2 was observed in patients who received two or more doses of TCZ (38/75), there was an increase in their mortality (47.4%) and ICU admission (86.8%). The 30-day mortality rate was 30.7% (20.5–42.4% CI) being hypertension, high initial d-dimer levels and ICU admission the only predictive factors found.
Conclusion
Based on our results, treatment with TCZ was associated with a fever, swelling and ventilator support improvement. However, there is no evidence that the administration of two or more doses of TCZ was related to a mortality decrease.
Similar content being viewed by others
Introduction
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is an emerging infectious process first described in Wuhan, China, which has spread rapidly to other countries since December 2019.
Most patients have mild cases whose symptoms are usually self-limiting (fever, dry cough, dyspnoea, nausea, diarrhoea, and rhinorrhoea) [1]. However, some patients progress rapidly to more severe (13.8%) and critical states (6.1%) developing Acute Respiratory Syndrome, septic shock and/or multiorgan failure [1, 2].
The mortality rate [Case Fatality Rate (CFR): number of deaths/number of confirmed cases] varies widely worldwide: Italy, 14.5%; the United Kingdom, 14%; Spain, 11.1%; Germany, 4.7%; China, 5.5%; and the United States, 5.4% [3]. Mortality increases with age (> 80 years, CFR 21.9%) and the presence of comorbidities: 13.2% in patients with cardiovascular disease, 9.2% in patients with diabetes and 8.4% in patients with hypertension [1].
Pneumonia caused by SARS-CoV-2 is characterised by the hyperactivation of effector T cells and a systemic inflammatory response caused by the excessive production of pro-inflammatory cytokines, especially Interleukin 6 (IL-6). This reaction, known as a “cytokine storm”, has been previously described in patients in response to iatrogenic or infectious stimuli. IL-6 and other cytokines produced in the cytokine storm contribute to the pathological process with increased vascular permeability and disseminated intravascular coagulation [4].
In the event of viral infection, the above processes contribute to the increased spread of the virus, thus providing a metabolic environment that can trigger patient death [2]. This process described in patients with COVID-19 relates to the clinical and analytical characteristics observed in cytokine release syndrome (CRS) [5, 6]. That is why several authors have proposed the blocking of IL-6 as adjunct therapy in patients who begin to develop the cytokine storm to reduce inflammation, inflammation-associated lung damage and Intensive Care Unit (ICU) hospitalisation [2, 7,8,9].
Tocilizumab (TCZ) is a humanised recombinant IgG1 monoclonal antibody that binds to interleukin 6 receptors both soluble and membrane-attached (IL-6Rs and IL-6Rm) and inhibits IL-6 mediated signalling. Currently, TCZ is indicated in CRS and other inflammatory processes related to the release of IL-6 such as rheumatoid arthritis, juvenile idiopathic arthritis, or Giant Cell Arteritis (GCA) [10].
Preliminary data from an observational study in China of 21 severe COVID-19 patients receiving TCZ showed clinical and radiological improvement with a decrease in C-reactive protein (84.2%) and an increased lymphocyte count (52.6%) [9].
Evidence to date shows that CRS occurs in a large number of severe patients with COVID-19, being one of the leading causes of death. IL-6 is a key molecule in the process, therefore, antagonising the IL-6 receptor with TCZ may be an attractive strategy in the treatment of patients with COVID-19. Several clinical trials are currently underway globally to evaluate the efficacy and safety of TCZ in COVID-19 treatment.
The aim of this study is to evaluate the safety and efficacy of TCZ treatment through the evolution of clinical and analytical parameters, as well as to investigate the factors influencing the prognosis and mortality of patients with CRS secondary to SARS-CoV-2 infection.
Methods
A retrospective, descriptive and observational study was conducted on patients hospitalised between the 18 March 2020 and the 18 April 2020 with a PCR COVID-19 positive test result for SARS-CoV-2 and whose clinical evolution required the administration of TCZ. The study was approved by the Ethics Committee for Drug Research at the Segovia Care Complex. The consent of all participants was obtained and reflected in the clinical records.
Patients were selected based on the following inclusion criteria: age between 18 and 85 years, evidence of pneumonia with imaging tests (chest X-ray or chest CT scan) and deterioration of the clinical situation during admission which required targeted TCZ treatment. The administration of TCZ was carried out following the recommendations of the hospital protocol: interstitial pneumonia with severe respiratory failure (SCORE ≥ 2), rapid respiratory deterioration that requires non-invasive or invasive ventilation (saturation ≤ 92% in ambient air or alveolar oxygen pressure ratio (PaO2)/Fraction of Inspired Oxygen (FiO2) ≤ 300 mmHg), presence of another organ failure (shock or a SOFA scale score ≥ 3), criteria of severe Systemic Inflammatory Response, high levels of IL-6 (> 40 pg/ml) (or alternatively: d-dimer levels (> 1.5 µg/ml) or progressively increased d-dimer) or radiological progression. Patients were excluded if they had: baseline levels of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) > 5 times the normal upper limit, neutrophils < 0.5 × 103/µl, platelets < 50 × 103/mm3, documented sepsis caused by other pathogens, presence of comorbidity that could lead to poor prognosis according to clinical judgment, complicated diverticulitis, intestinal perforation or ongoing skin infection. Concomitant therapy with antibiotics, corticosteroids, lopinavir/ritonavir, and hydroxychloroquine was permitted.
TCZ was administered intravenously (central or peripheral) at fixed doses of 600 mg (patients ≥ 75 kg) and 400 mg (patients < 75 kg) over 1-h periods. Patients experiencing worsening analytical parameters, respiratory status or partial clinical improvement received a second and/or third administration of TCZ 12 and 24 h after the first infusion.
The following demographic variables were analysed: age, sex, comorbidities (arterial hypertension, dyslipidemia, Diabetes Mellitus, obesity, smoking, stroke, ischaemic heart disease, asthma and chronic obstructive pulmonary disease (COPD)) and time elapsed from the onset of symptoms until hospital admission.
Analyses were carried out of the values of total lymphocytes, C-reactive protein (CRP), d-dimers and ferritin on days 0 (basal) and 1, 3 and 5 after administration of the first dose of TCZ, as well as the levels of IL-6 before treatment with TCZ. The clinical evolution of patients was analysed using: the disappearance of fever (> 38 °C), radiological improvement (chest X-ray), the evolution of Acute Respiratory Distress Syndrome (ARDS) by means of the PaO2/FiO2 ratio, whether admission to ICU was required or not, hospital admission duration and mortality rate after 30 days. The safety of the treatment was analysed through the adverse reaction log, which was reflected in the medical history. Procalcitonin levels prior to TCZ administration were analysed to avoid the occurrence of possible co-infections.
The data were analysed using the SPSS version 22.0 (SPSS Inc. IBM) software. Quantitative variables were described using absolute frequency and percentage tables, with 95% Confidence Intervals estimate (95% CI). The statistical normality adjustment of quantitative variables was tested with the Kolmogorov–Smirnov Test and categorised using the Cochran and McNemar Test. For the study of the influence of the data collected on mortality, a univariate analysis was carried out using the Chi-square and Kaplan–Meier log-rank Test. Values p < 0.05 (5%) were considered statistically significant.
Results
A total of 75 patients were included, 55 men (73.3%) and 20 women (26.7%), with positive PCR test results for SARS-CoV-2. The mean age was 64 years (range from 24 to 84). Most patients had a diagnosis of bilateral pneumonia (72/75; 96%). Forty-three patients (57.3%) had one or more cardiovascular risk factors (arterial hypertension 26.7%, dyslipidemia 26.7%, diabetes mellitus 16%, obesity 20% and/or smoking 8%), 7 patients (9.3%) had 1 or more cardiovascular diseases (ictus 4%, ischaemic heart disease 6.7%) and 13 patients (17.3%) had at least a lung disease (COPD 4%, asthma 5.3%, others 9.3%) (Table 1).
Prior to administration of TCZ, 23/75 patients (30.6%) had a fever (> 38 °C), and all patients had received corticosteroids (methylprednisolone 250 mg) 1–3 days before TCZ administration. The PaO2/FiO2 ratio mean at the start of treatment was 145.5 mmHg (range 55–416 mmHg) with 19/75 patients with mild ARDS (25.3%), 37/75 with moderate ARDS (49.4%) 19/75 with severe ARDS (25.3%). In the analysis prior to the administration of TCZ, most patients (91.8%) had a decreased lymphocytic count (mean: 0.7 ± 0.4 × 103/µl) and all of them had elevated CRP levels (mean: 15.7 ± 11.4 mg/dl). d-Dimer and ferritin were also elevated with means prior to treatment of 2.2 µg/ml (range from 0.3 to > 20.0 µg/ml) and 1446 ng/ml (range from 79 to 11,445 ng/ml), respectively. IL-6 levels in serum prior to the administration of TCZ could be determined in 16 patients with a mean of 83 pg/ml (range from 5.3 to 487 pg/ml).
Thirty-seven patients (49.3%) received a single dose of TCZ and 38 (50.7%) received 2 or more doses. The mean of the first and second administered dose of TCZ were 600 mg and 400 mg, respectively. Due to the clinical situation, nine patients (12%) received a third dose of TCZ with a mean dose of 400 mg. The mean time from the onset of symptoms to the administration of the first dose of TCZ was 12.6 ± 6.5 days (CI 11.3–13.9).
Owing to clinical deterioration, 47/75 patients (62.7%) had to be admitted to the ICU. The mean time spent in ICU was 18.9 ± 14.2 days. The univariate analysis showed obesity (p = 0.032), the value of the initial d-dimer number > 1.5 µg/ml (p = 0.03) and a severe initial PaO2/FiO2 ratio (p < 0.05) as predictive factors for ICU admission. None of the patients who were admitted to the ICU had COPD. In fact, the statistical analysis showed COPD as a protective factor (p < 0.05) of ICU admission.
The 30-day mortality rate was 30.7% (23/75; CI 20.5–42.4%). Treatment with TCZ was associated with a statistically significant reduction in lymphocytopenia (p < 0.01), CRP value (p < 0.01), cases with severe ARDS (p < 0.01) and fever (p < 0.01) on day 5 after its administration (Table 2). No significant variation in d-dimer and ferritin values was found after treatment with TCZ.
Inferential analysis segmenting into two subgroups according to the number of TCZ doses showed greater statistical significance in the improvement of PaO2/FiO2 ratio in patients receiving two or more doses (p < 0.01 vs p < 0.05). The decrease in lymphocytopenia, however, could only be demonstrated in the group of patients receiving a single dose of TCZ (Table 3). In the associative inferential analysis of TCZ doses and the analytical and clinical variables collected, a statistically significant relationship was observed between the doses of TCZ received and the baseline PaO2/FiO2 ratio: patients with severe and moderate ARDS received two or more doses (p < 0.01). Similarly, higher mortality (47.4% vs 13.5%; p < 0.01) and ICU admission (86.8% vs 38.8%; p < 0.01) were observed in patients receiving two or more doses of TCZ compared to those receiving a single dose. The number of TCZ doses received and an improvement in chest X-ray or fever could not be linked.
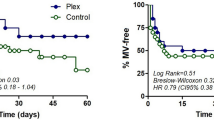
A univariate analysis of the various mortality factors collected was carried out, revealing a significant relation in patients with a clinical history of arterial hypertension (p = 0.029), initial values of d-dimer > 1.5 µg/ml (p = 0.048) and admitted to the ICU (p < 0.05). However, it was not possible to develop a joint predictive model.
The hospital stay mean was 21 days (range from 5 to 71). Four patients experienced a temporary increase in ALT/AST liver enzymes after TCZ administration. No other adverse effects attributable to TCZ were described.
Discussion
Given the current global situation, many Medicine Agencies are trying to seek effective treatment for SARS-CoV-2 or a vaccine capable of curbing its transmission. To date, however, no drug treatment has proved to be effective in the management of ARDS in patients with COVID-19 [11]. This study describes our experience with TCZ treatment in 75 severe and critical patients with COVID-19 admitted to a secondary level hospital in Spain.
Treatment with TCZ was significantly associated with an elevated lymphocyte count and reduced CRP and fever on day 5 after administration of TCZ. In addition, a significant increase in PaO2/FiO2 ratio was observed, with improvements in patients with severe and moderate ARDS. These findings coincide with those reported by the other authors [9, 11,12,13,14]. Unlike Luo et al. and Alattar et al., we were unable to find any significant differences in radiographic improvement after treatment with TCZ [11, 12].
In patients with COVID-19, especially those with a more severe pathology, there is a massive release of pro-inflammatory mediators and cytokines such as IL-1, IL-2, IL-6, IL-7, granulocyte colony-stimulating factor, macrophage inflammatory protein1-alpha, tumour necrosis factor α (TNFα), CRP, ferritin and d-dimer [15,16,17,18,19]. This cytokine storm, in addition to the patient’s aberrant immune response, is associated with viral replication and lung damage, with the formation of alveolar exudates that hinder gas exchange and favour the appearance of the ARDS, which can trigger multiorgan failure [17, 19, 20]. Based on these clinical parameters, it has been suggested that the immunological profile of the disease in severe COVID-19 patients resembles that of the CRS [21, 23]. Therefore, the use of immunomodulatory strategies, such as those used in CRS may interfere with cytokine signalling and reduce hyperinflammation [21,22,23]. Several immunomodulatory therapies have been proposed, including specific (IL-1 and IL-6 receptor antagonists, Janus Kinase inhibitors, anti-TNFα and convalescent plasma) and nonspecific immunomodulators (corticosteroids, human immunoglobulin, interferons, hydroxychloroquine/chloroquine and prostaglandin D2 modulators) [21,22,23].
A study conducted by Wang et al. in 11 critical patients showed a significant increase in IL-6 as an early indicator of CRS-like reactions in pneumonia produced by SARS-CoV-2 [24]. The other authors suggest that the severity of the infection could be related to elevated IL-6 values, so it could be an appropriate candidate in monitoring patients during the infection, even after administration of TCZ [25,26,27]. Our study could only determine previous IL-6 levels in 16 patients due to a lack of reactive laboratory material up to the 3rd week after the pandemic started as it was not a regular analytical test. More than half of the patients had higher IL-6 levels than the normal limit (> 40 pg/ml). Given the low number of samples, nevertheless, no relation could be found with high values of CRP, lymphocytopenia, d-dimer or ferritin [25].
Approximately half of the patients received a single intravenous dose and the rest of the patients received two or more doses with an interval of 12 h or 24 h since the first dose. The dosage regimen of TCZ is very variable throughout the studies, not having an exact regimen [11,12,13,14, 28]. The recommended dosage in Juvenile Idiopathic Arthritis and CRS is 8 mg/kg up to a maximum of 800 mg [10]. Nevertheless, given the lack of experience in patients with COVID-19 and the shortage of TCZ in March, our country’s Ministry of Health established recommendations based on the guidelines collected for other known pathologies and data published up to that time [9, 29,30,31,32]. Some authors suggest that, in patients with severe ARDS, a single TCZ dose of 400 mg may not uniformly block all IL-6Rs, especially if there is a large amount of IL-6/IL-6R complex circulation that reduces the efficacy of TCZ [12, 33]. However, it is currently unknown which dose or route of administration could be associated with better results.
In the analysis of the results obtained based on the administered doses, a greater improvement in PaO2/FiO2 ratio was observed in patients receiving two or more doses compared to those receiving a single dose. This effect coincides with what has recently been described by the other authors, suggesting that the benefit could be in patients at higher risk of death or mechanical ventilation [34].
In analysing baseline differences between the two groups of patients, it was observed that those receiving two or more doses of TCZ had a lower PaO2/FiO2 ratio, with a higher proportion of patients with severe and moderate ARDS. Similarly, on day 5, after administration of TCZ, all patients administered two or more doses maintained d-dimer values greater than 0.5 µg/ml, so they were in a more serious clinical situation. Given the baseline situation of this group of patients, it is reasonable to find higher mortality and admission to ICU than in those patients who received a single administration. In a recently published retrospective study, Campochiaro et al. also noted that patients receiving TCZ and with a higher baseline PaO2/FiO2 ratio were associated with clinical improvement. However, as other authors, they found no differences between patients who had received one or more doses of TCZ [28, 35].
The 30-day mortality rate was comparable to that reported in Milan in 45 patients with severe SARS-CoV-2 pneumonia treated with intravenous TCZ and similar inclusion criteria (mortality 27%) [13]. COVID-19 mortality has been highly variable (10–45%), with most estimates at about 30% [36]. Some of these variations may be related to age difference, health-care delivery and a higher prevalence of comorbidities (cardiovascular disease, hypertension, and diabetes mellitus) [1, 36,37,38].
In our study, we did not find age-related differences, but we did find a statistically significant increase in mortality in patients with arterial hypertension and those with baseline d-dimer levels greater than 1.5 µg/ml. A prospective, multicentre study with 63 severe COVID-19 patients receiving intravenous (8 mg/kg) or subcutaneous (324 mg) TCZ were able to link baseline d-dimer levels to mortality [HR 5.01; 95% CI 1.04–29.17]. The authors concluded that treatment with TCZ managed to reduce mortality 6 days after treatment [HR 2.2; 95% CI 1.3–6.7 p < 0.05] on improving PaO2/FiO2 ratio and PCR, ferritin, d-number and lymphocyte count levels [39].
Since a joint predictive model could not be reached, the variables that influenced the admission of patients to ICU were studied. The only comorbidity that was significantly associated with ICU admission was obesity. A descriptive study of COVID-19 critical patients in the Seattle region was one of the first to analyse the influence of body mass index (BMI) on patient prognosis. In this study, the authors observed that 85% of obese patients required mechanical ventilation and 62% died. These proportions were higher than those of non-obese patients, in which 64% required mechanical ventilation and 36% died [40]. Conversely, and unlike what has been reported in other articles, COPD patients were associated with a lower ICU admission [1, 37, 38].
As part of our hospital protocol, patients received antivirals (lopinavir/ritonavir 400/100 mg BID for 7 days) and hydroxychloroquine (200 mg BID for 5 days). However, over time, antiviral and immunomodulatory treatment with hydroxychloroquine was removed from the protocol due to new publications showing the lack of benefit of this treatment beyond the standard of care in COVID-19 [41, 42].
As adjunct therapy for hyperinflammation, patients received methylprednisolone 250 mg for 3 days before the administration of TCZ. Corticosteroids are involved in a high number of key physiological processes including the immune response and inflammation [21, 27]. The rationale for its use is to downregulate pro-inflammatory cytokine transcription and decrease host inflammatory responses in the lungs, particularly in advanced stages of the disease [21, 22]. However, their use in COVID-19 patients is a much-debated topic due to their adverse events, including delayed viral clearance and an increased of secondary infections [21,22,23]. Recently, preliminary results of the RECOVERY trial reported that the administration of dexamethasone 6 mg/day for 10 days resulted in a lower mortality rates among patients requiring oxygen or mechanical ventilation [HR 0.64; 95% CI 0.50–0.82; p < 0.01] [43]. Consequently, the last interim guidance of the World Health Organization (WHO) recommends the use corticosteroids in the treatment of patients with severe and critical COVID-19 [44]. In addition, Ramiro et al. showed that in 172 patients with COVID-19-associated cytokine storm syndrome, the use of high-dose intravenous methylprednisolone (250 mg on day 1 followed by 80 mg on days 2–5) and TCZ (8 mg/kg body weight, single infusion) in 86 patients was associated with less mortality [HR 0.35; 95% CI 0.19–0.65] and less invasive mechanical ventilation [HR 0.29; 95% CI 0.14–0.65] than methylprednisolone alone (control group) [45].
Due to the absence of a control group in our study, we cannot establish conclusions about the synergistic role of corticosteroids and TCZ in severe patients. Additional data are required for TCZ patients who had previously received corticosteroids.
Treatment with TCZ was well tolerated; only four patients experienced a temporary increase in ALT/AST liver enzymes, which was corrected by discontinuing the administration of the drug. This adverse effect is included in the medicine data sheet along as well as the onset of infections in the upper respiratory tract, nasopharyngitis, headache and hypertension [10]. Cases of elevated transaminase, thrombocytopenia and neutropenia have been reported in patients with COVID-19 receiving TCZ treatment [13, 46]. However, it is unknown whether these could be due to the effect of SARS-CoV-2 itself or the concomitant administration of other drugs [13].
Our study has some limitations. First, due to the limited number of patients, significant risk and mortality factors could not be determined using adjusted multivariate methods. Second, due to a shortage of laboratory material in March, IL-6 could only be determined in a small group of patients. Finally, due to the lack of a control group, no definitive conclusions can be drawn. All patients had received other therapies (corticosteroids, antibiotics, lopinavir/ritonavir and hydroxychloroquine), following the recommendations of the protocols and guidelines available at the start of the pandemic. It is, therefore, difficult to draw definitive conclusions regarding the benefit of TCZ in these patients. Randomised prospective studies with a greater number of patients and a control group will help to determine the effectiveness of TCZ based on severity status, as well as the dose and administration route that could provide the most benefit in patients with COVID-19.
In conclusion, treatment with tocilizumab was associated with an improvement in fever, inflammation and ventilatory support in patients with severe cases of CRS and pneumonia produced by SARS-CoV-2. Nonetheless, the patients with the most severe cases continued to show higher mortality despite having received two or more doses.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ARDS:
-
Acute Respiratory Distress Syndrome
- AST:
-
Aspartate aminotransferase
- BID:
-
Bis in die
- BMI:
-
Body mass index
- CFR:
-
Case Fatality Rate
- CI:
-
Confidence Intervals
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus Disease 2019
- CRP:
-
C-reactive protein
- CRS:
-
Cytokine release syndrome
- CT:
-
Computed tomography
- GCA:
-
Giant Cell Arteritis
- HBP:
-
High blood pressure
- HR:
-
Hazard ratio
- ICU:
-
Intensive Care Unit
- IL-1:
-
Interleukin 1
- IL-2:
-
Interleukin 2
- IL-6:
-
Interleukin 6
- IL-6Rs:
-
Interleukin 6 soluble receptor
- IL-6Rm:
-
Interleukin 6 membrane-attached receptors
- IL-7:
-
Interleukin 7
- PaO2/FiO2 :
-
Alveolar oxygen pressure/fraction of inspired oxygen
- PCR:
-
Polymerase chain reaction
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- TCZ:
-
Tocilizumab
- TNFα:
-
Tumour necrosis factor alpha
- WHO:
-
World Health Organization
References
World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed 19 June 2020.
Mingxuan X, Qiong C. Insight into novel coronavirus—an updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis. 2020;94:119–124. https://doi.org/10.1016/j.ijid.2020.03.071.
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real-time [published online the 19th of February, 2020]. Lancet Infect Dis. Last updated on the 19th of June, 2020. 2020. https://coronavirus.jhu.edu/data/mortality. Accessed 19 June
Alhazzani W, Hylander M, Arabi Y, Loeb M, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Society of Critical Care Medicines and European Society of Intensive Care Medicine. Crit Care Med. 2020;48(6):e440–69.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Ruan Q, Yan K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–8.
Bonam SR, Kaveri SV, Sakuntabhai A, Gilardin L, Bayry J. Adjunct immunotherapies for the management of severity ill COVID-19 patients. Cell Rep Med. 2020;1(2):1–11.
Zhang C, Wu Z, Li J-W, Zhao H, Wang G-Q. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. 2020;55(5):105954.
Xialing X, Mingfeng H, Tiantian L et al. Effective treatment of severe COVID-19 patients with tocilizumab. https://www.ser.es/wp-content/uploads/2020/03/TCZ-and-COVID-19.pdf. Accessed 24 Mar
Ficha Técnica Roactemra 20 mg/ml. Concentrado para solución para perfusión. Agencia Española de Medicamentos y Productos Sanitarios. https://cima.aemps.es/cima/dochtml/ft/08492001/FT_08492001.html. Accessed 9 Apr
Alattar R, Ibrahim TBH, Shaar SH, et al. Tocilizumab for the treatment of severe COVID-19. J Med Virol. 2020:1–8.
Luo P, Liu Y, Qiu L, Liu X, Liu D, Li J. Tocilizumab treatment in COVID-19: a single center experience. J Med Virol. 2020;1–5.
Morena V, Milazzo L, Oreni L, Bestetti G, Fossali T, et al. Off-label use of tocilizumab for the treatment of SARS-CoV-2 pneumonia in Milan, Italy. Eur J Intern Med. 2020;76:36–42.
Uysal B, Ikitimur H, Yavuzer S, Ikitimur B, Uysal H, Islamoglu MS, Ozcan E, Aktepe E, Yavuzer H, Cengiz M. Tociluzumab challenge: a series of cytokine storm therapy experience in hospitalised Covid-19 pneumonia patients. J Med Virol. 2020. https://doi.org/10.1002/jmv.26111
Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39(5):405–7.
Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, Caporali R. COVID-19 infection and rheumatoid arthritis: faraway, so close! Autoimmun Rev. 2020;19(5):102523.
Fu B, Xu X, Wei H. Why tocilizumab could be an effective treatment for severe COVID-19? J Transl Med. 2020;18:164.
Quin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71(15):762-768.
Cardone M, Yano M, Rosenberg AS, Puig M. Lessons learned to date on COVID-19 hyperinflammatory syndrome: considerations for interventions to mitigate SARS-CoV-2 viral infection and detrimental hyperinflammation. Front Immunol. 2020;11:1131.
McGonagle D, Sharif K, O’Regan A, Bridgewood C. The Role of Cytokines, including Interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020;19(6):102537.
Rizk JG, Kalantar-Zadeh K, Mehra MR, Lavie CJ, Rizk Y, Forthal DN. Pharmaco-immunomodulatory therapy in COVID-19. Drugs. 2020;80(13):1267–92.
Bonam SR, Kaveri SV, Sakuntabhai A, Gilardin L, Bayry J. Adjunct immunotherapies for the management of severely ill COVID-19 patients. Cell Rep Med. 2020;1(2):100016.
Alijotas-Reig J, Esteve-Valverde E, Belizna C, et al. Immunomodulatory therapy for the management of severe COVID-19. Beyond the anti-viral therapy: a comprehensive review. Autoimmun Rev. 2020;19(7):102569.
Wang W, He J, Lie P et al. The definition and risks of cytokine release syndrome-like in 11 COVID-19-infected pneumonia critically ill patients: disease characteristics and retrospective analysis. medRxiv 2020.02.26.20026989; 2020 (Published 2020 the 27th of February).
Liu T, Zhang J, Yang Y, Ma H, Li, Z, Zhang J, Cheng J, Zhang X. The potential role of IL-6 in monitoring coronavirus disease 2019. SSRN: https://ssrn.com/abstract=3548761 or https://doi.org/10.2139/ssrn.3548761. Accessed 10 Mar 2020
Quartuccio L, Sonaglia A, Pecori D, Peghin M, Fabris M, Tascini C, De Vita S. Higher levels of IL-6 early after tocilizumab distinguish survivors from non-survivors in COVID-19 pneumonia: a possible indication for deeper targeting IL-6. J Med Virol. 2020. https://doi.org/10.1002/jmv.26149
Russell B, Moss C, George G, et al. Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence. Ecancermedicalscience. 2020;14:1022 (Published 2020 the 27th of March).
Hassoun A, Thottacherry ED, Muklewicz J, Aziz Q, Edwards J. Utilizing tocilizumab for the treatment of cytokine release syndrome in COVID-19 [Letter to the Editor]. J Clin Virol. 2020;128:104443.
Tratamientos disponibles para el manejo de la infección respiratoria por SARS-CoV-2. Agencia Española de Medicamentos y Productos Sanitarios. Ministerio de Sanidad (Published: March 10, 2020, Last updated: May 28, 2020).
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62 (Published Online on the 9th of March, 2020).
Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan. China. Allergy. 2020;75(7):1730–41 (Accepted: the 18th of February 2020).
Sociedad Española de Reumatología. Nota informativa sobre el uso de tocilizumab y eculizumab para el tratamiento de COVID-19. https://www.ser.es/nota-informativa-sobre-el-uso-de-tocilizumab-y-eculizumab-para-el-tratamiento-de-covid-19/. Accessed 14 Mar 2020
Jordan SC, Zakowski P, Tran HP, Smith EA, Gaultier C, Marks G, et al. Compassionate use of tocilizumab for treatment of SARS-CoV-2 pneumonia. Clin Infect Dis. 2020;ciaa812.
Guaraldi G, Meschiari M, Cozzi-Lepri A, Milic J, Tonelli R, Menozzi, et al. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. Lancet Rheumatol. 2020;2(8):e474–84 (Published online June 24, 2020).
Campochiaro C, Della-Torre E, Cavalli G, et al. Efficacy and safety of tocilizumab in severe COVID-19 patients: a single-centre retrospective cohort study. Eur J Intern Med. 2020;76:43–9.
Price CC, Altice FL, Shyr Y, et al. Tocilizumab treatment for cytokine release syndrome in hospitalized patients with coronavirus disease 2019: survival and clinical outcomes. Chest. 2020;158(4):1397–408.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242 (published online the 24th of February, 2020)
Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–55.
Sciascia S, Apra F, Baffa A, et al. Pilot prospective open, single-arm multicentre study on off-label use of tocilizumab in patients with severe COVID-19. Clin Exp Rheumatol. 2020;38(3):529–32. (Epub 2020, the 1st of May)
Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020;382(21):2012–22.
RECOVERY Collaborative Group, Horby P, Mafham M, et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020. https://doi.org/10.1056/NEJMoa2022926(published online ahead of print, 2020 Oct 8)
Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–99.
The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324(13):1330–41.
World Health Organization Working Group. Corticosteroids for COVID-19 living guidance. WHO reference number: WHO/2019-nCoV/Corticosteroids/2020.1 (published online the 2nd of February, 2020).
Ramiro S, Mostard RLM, Magro-Checa C, et al. Historically controlled comparison of glucocorticoids with or without tocilizumab versus supportive care only in patients with COVID-19-associated cytokine storm syndrome: results of the CHIC study. Ann Rheum Dis. 2020;79(9):1143–51.
Morrison AR, Johnson JM, Ramesh M, Bradley P, et al. Letter to the Editor: Acute hypertriglyceridemia in patients with COVID-19 receiving tocilizumab. J Med Virol. 2020. https://doi.org/10.1002/jmv.25907(published online ahead of print 2020, Apr 21).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We would like to thank to all our workmates that have been involved in the care of COVID-19 patients during all these months.
Author information
Authors and Affiliations
Contributions
All the authors have contributed equally for the study design, data interpretation and final version approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study has been approved by Ethics Committee for Drug Research at the Segovia Care Complex and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Cáceres, C., Martínez, R., Bachiller, P. et al. The effect of tocilizumab on cytokine release syndrome in COVID-19 patients. Pharmacol. Rep 72, 1529–1537 (2020). https://doi.org/10.1007/s43440-020-00186-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-020-00186-z