Prealbumin: A New Biomarker for Predicting Prognosis in Patients with Severe COVID-19
By Kubilay Issever1, Ahmed Cihad Genc2, Deniz Cekic3, Ilhan Yildirim4, Ahmed Bilal Genc3, Selcuk Yaylaci5Affiliations
doi: 10.29271/jcpsp.2021.07.99ABSTRACT
Objective: To analyse whether prealbumin could be a new biomarker for predicting mortality in severe COVID-19 patients.
Study Design: An observation study.
Place and Duration of Study: Intensive care units (ICU) of Sakarya University Training and Research Hospital, Sakarya, Turkey, from October 2020 to December 2020.
Methodology: The data of 149 patients, who were admitted to the ICU were collected and analysed retrospectively. Routine blood samples were collected from all patients at the time of admission to the ICU; and 102 patients with the mortal course and 47 patients with the non-mortal course were included in the study. The data obtained from these patients were analyzed in the biostatistics programme.
Results: The median age of all patients was 68 years; while 94 of them were males (63.1%) and 55 of them were females (36.9%). Median levels of potassium (K) (p=0.04), uric acid (p=0.001), C-reactive protein (CRP) (p=0.004), and procalcitonin (PCT) (p<0.001) were significantly higher and median level of prealbumin (p=0.002) was significantly lower in the deceased group. The cut-off level of prealbumin for mortality was found as 0.085 g/L (p=0.002). Further analysis revealed that the risk of mortality was found as 2.193 times more in patients with prealbumin levels of <0.085 g/L (Odds Ratio (OR): 2.193, 95% CI: 1.084-4.434).
Conclusion: As a result of this study, it was found that patients with lower levels of prealbumin at the time of admission to the ICU have a higher risk for mortality. It was showed that prealbumin can be a useful biomarker for predicting mortality in patients with severe COVID-19.
Key Words: Prealbumin, COVID-19, Mortality, Prognostic biomarkers, Severe disease.
INTRODUCTION
In 1942, a protein showing itself onwards of albumin in the electrophoresis of cerebrospinal fluid and human plasma samples was detected and entitled as ‘prealbumin.’ Afterward, it was discovered that this protein could bind to both thyroid hormones and retinol-binding protein (RBP) and thus renamed as transthyretin (TTR).1 It can be synthesised from the choroid plexus as well as the liver.2 Lately, new impacts of this protein in proteolysis and several functions in the nervous system, such as the roles in behavior, cognition, and axonal growth have been discovered.1
Along with albumin, serum prealbumin usually takes part in the evaluation of malnutrition and nutritional support in daily practice.3 Prealbumin has been widely used as a nutritional biomarker, especially in older patients; and the assessment of refeeding syndrome. Since prealbumin has a shorter half-life compared to albumin (2-3 days vs. 20 days), its use in acute changes of the nutritional state is accepted as superior to the use of albumin. Another advantage of prealbumin is that it can be used safely as a biomarker in patients with protein-losing enteropathy, since its levels are not affected by protein losses in the intestines.3,4 Serum prealbumin concentrations less than 0.1 g/L are associated with malnutrition.5
Prealbumin levels may decrease in conditions such as overhydration, infections, physiological stress, malnutrition, and liver dysfunction; whereas, its levels may increase in the setting of fluid loss, steroid treatment, and renal impairment.6 The role of albumin and prealbumin in diagnosing malnutrition in patients with inflammatory diseases has been a matter of debate since their levels are affected by inflammation. When there is evidence of an acute phase response, concentrations of plasma proteins such as prealbumin and albumin that are known as “reverse acute phase reactants” may not reflect malnutrition.3 In a study, it was revealed that a prealbumin level of < 0.11 g/L was associated with increased mortality and length of stay. Furthermore, an increase of less than 0.04 g/L per week indicated failure of nutritional therapy.6 The role of prealbumin in predicting prognosis in different pathological states, such as cardiovascular diseases, lung cancer, and gastric cancer, has been reported by several publications so far.3,4
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) has spread worldwide causing a wide range of symptoms from mild (fever, cough, myalgia, and anosmia) to severe (respiratory failure, multiple organ dysfunction syndrome, coma, and death). Although the lung is the main organ attacked by SARS-CoV-2, extrapulmonary organ injuries might be also observed in these patients.7 Liver injury has been reported in previous studies on COVID-19; high rates of abnormal alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total bilirubin (TB) levels were reported in patients with COVID-19.8-13
It has been increasingly reported that malnutrition, which is associated with poor clinical outcomes, is frequently seen in patients with severe COVID-19. Since there is no certain curative treatment and enough percentage of vaccinated populations for COVID-19 yet, biomarkers that might provide a combined assessment of the processes partaking in the pathophysiology of COVID-19 such as malnutrition, liver injury, and inflammation might be useful with respect to appropriate clinical decisions and predictive capacity.14 For this reason, the aim of this study was to analyse whether prealbumin could be a new biomarker to predict prognosis in patients with severe COVID-19.
METHODOLOGY
The medical records of the patients who were admitted to the ICU of Sakarya University Training and Research Hospital with the diagnosis of COVID-19 between October 2020 and December 2020 were analysed, retrospectively. Nasopharyngeal swab PCR test positivity was accepted as the gold standard for the diagnosis of COVID-19. Patients who were below the age of 18 and had a negative PCR test result were excluded from the study. One hundred and two patients with mortal outcomes and 47 patients with favourable outcomes were included in the study. Prealbumin levels along with other lab parameters of all these patients, which had already been studied at the time of admission to ICU, were analysed. Demographical data, such as age, gender, and comorbidities of the patients were recorded. Obtained data were analysed in the biostatistical programme.
Descriptive analyses were performed to provide information on general characteristics of the study population. Visual (probability plots, histograms) and analytical methods (Kolmogorov-Simirnov/Shapiro-Wilk’s tests) were used to determine whether or not they are normally distributed. Mann-Whitney U-test used for non normally numeric variables between two groups. Descriptive analyses were presented using medians and 25-75th percentile for the non normally distributed variables. Chi-square tests were used to compare the categorical variables between two groups. The categorical variables were presented as the frequency (% percentage). A p-value <0.05 was considered significant. The performance of prealbumin was assessed using receiver operating characteristic (ROC) curve analysis and by calculating the area under the curve (AUC) of the ROC curve. When a significant cut-off value was observed, the sensitivity, specificity values were presented. Analyses were performed using SPSS statistical software (IBM SPSS Statistics, Version 21.0. Armonk, NY: IBM Corp.).
RESULTS
The median age of all patients was 68 years; 94 of them (63.1%) were males and 55 of them (36.9%) were females. The median age of the deceased patients was 69.5 (IQR: 64-76); whereas, the median age of discharged patients was 64 (IQR: 57-72), and this difference was statistically significant (p=0.004). Ninety-eight of the 100 intubated patients died and only two of these patients survived, which revealed a strong relationship of intubation with mortality (p<0.001). No significant difference was found between survivor and nonsurvivor patients, who received non-invasive mechanical ventilation (NIMV) and high flow nasal cannula (HFNC) therapy (p=0.051 and p=0.849, respectively). Median levels of K (p=0.04), UA (p=0.001), CRP (p=0.004), and PCT (p<0.001) were significantly higher and median level of prealbumin (p=0.002) was significantly lower in the deceased group. However, no significant difference was found between the survivor and the nonsurvivor group in terms of plasma sodium (Na), d-dimer, sedimentation levels and duration of intubation (p>0.05, Table I).
The cut-off value of prealbumin for COVID-19 was determined as 0.085 g/L. 61 of 80 patients with prealbumin levels below this value died, while only 19 of them survived. This analysis showed that prealbumin levels <0.085 g/L have a significant association with mortality (p=0.027, Table I).
The cut-off value of prealbumin for COVID-19 was determined as 0.085 g/L in this centre. Sensitivity and specificity were 59.8% and 59.6%, area under curve (AUC) was 65.6%, 95% confidence interval (CI) was 56.5%-74.7%, and p-value was 0.002. Patients were divided into two groups according to the cut-off value of prealbumin, as the ones with prealbumin levels <0.085 g/L and the ones with prealbumin levels ≥0.085. A 2.193 times higher mortality risk for the patients with prealbumin levels <0.085 g/L was found as a result of further analysis (Odds Ratio (OR): 2.193, 95% CI: 1.084 - 4.434) (Figure 1).
DISCUSSION
In this study, which was conducted with 149 patients followed up in ICU, 102 of whom with the mortal outcome and 47 of whom with the favorable outcome, the median age was found as 68 and 63.1% of the patients were males. Congruently, the median age was 63 and male predominance (82%) was seen in a demographic study which was conducted with 1591 ICU patients in Italy.15
Table I: Distribution of the demographic, laboratory, and clinical parameters among the survivor and nonsurvivor patients with severe COVID-19.|
Parameters |
Nonsurvivors |
Survivors |
Total |
p-value |
|
Age (median, 1st-3rd) |
69.5 (64-76) |
64 (57-72) |
68 (62-75) |
0.004 |
|
Males (n, %) |
65 (%63.7) |
29 (%61.7) |
94 (%63.1) |
0.812 |
|
Females (n, %) |
37 (%36.3) |
18 (%38.3) |
55 (%36.9) |
|
|
Na (median mmol/L, 1st-3rd) |
138 (133-143) |
138 (135- 140) |
138 (133-142) |
0.522 |
|
K (median mmol/L, 1st-3rd) |
4.5 (4-4.9) |
4.1 (3.9-4.7) |
4.4 (4-4.9) |
0.04 |
|
UA (median mg/dl, 1st-3rd) |
7 (4.9-9.4) |
5.2 (4.1-6.1) |
6.1 (4.6-8.7) |
0.001 |
|
D-dimer (median µgFEU/L, min-max) |
1760 (659-4620) |
1750 (653-3610) |
1755 (658.5-4500) |
0.696 |
|
CRP (median mg/L, 1st-3rd) |
121 (74.6-185) |
73.4 (32.3-149) |
111 (60.9-174) |
0.004 |
|
PCT (median ng/ml, 1st-3rd) |
0.83 (0.29-2.75) |
0.26 (0.1-0.58) |
0.58 (0.2-1.88) |
<0.001 |
|
Sedimentation (median mm/hour, 1st-3rd) |
66 (41-79.5) |
66 (44-85) |
66 (42-84) |
0.726 |
|
Prealbumin (median g/L, 1st-3rd) |
0.08 (0.04-0.1) |
0.09 (0.07-0.13) |
0.08 (0.05-0.11) |
0.002 |
|
Prealbumin <0.085 g/L (n, %) |
61 (%59.8) |
19 (%40.4) |
80 (%53.7) |
0.027 |
|
Intubation (n, %) |
98 (%96.1) |
2 (%4.3) |
100 (%67.1) |
<0.001 |
|
Duration of intubation (median days, 1st-3rd) |
5 (1-9) |
3.5 (3-4) |
5 (1-9) |
0.66 |
|
NIMV (n, %) |
22 (%21.6) |
4 (%8.5) |
26 (%17.4) |
0.051 |
|
HFNC (n, %) |
14 (%13.7) |
7 (%14.9) |
21 (%14.1) |
0.849 |
|
MWU and Chi-square tests were used and the results were determined as median, 1st and 3rd quarters, numbers, and percentages. |
||||
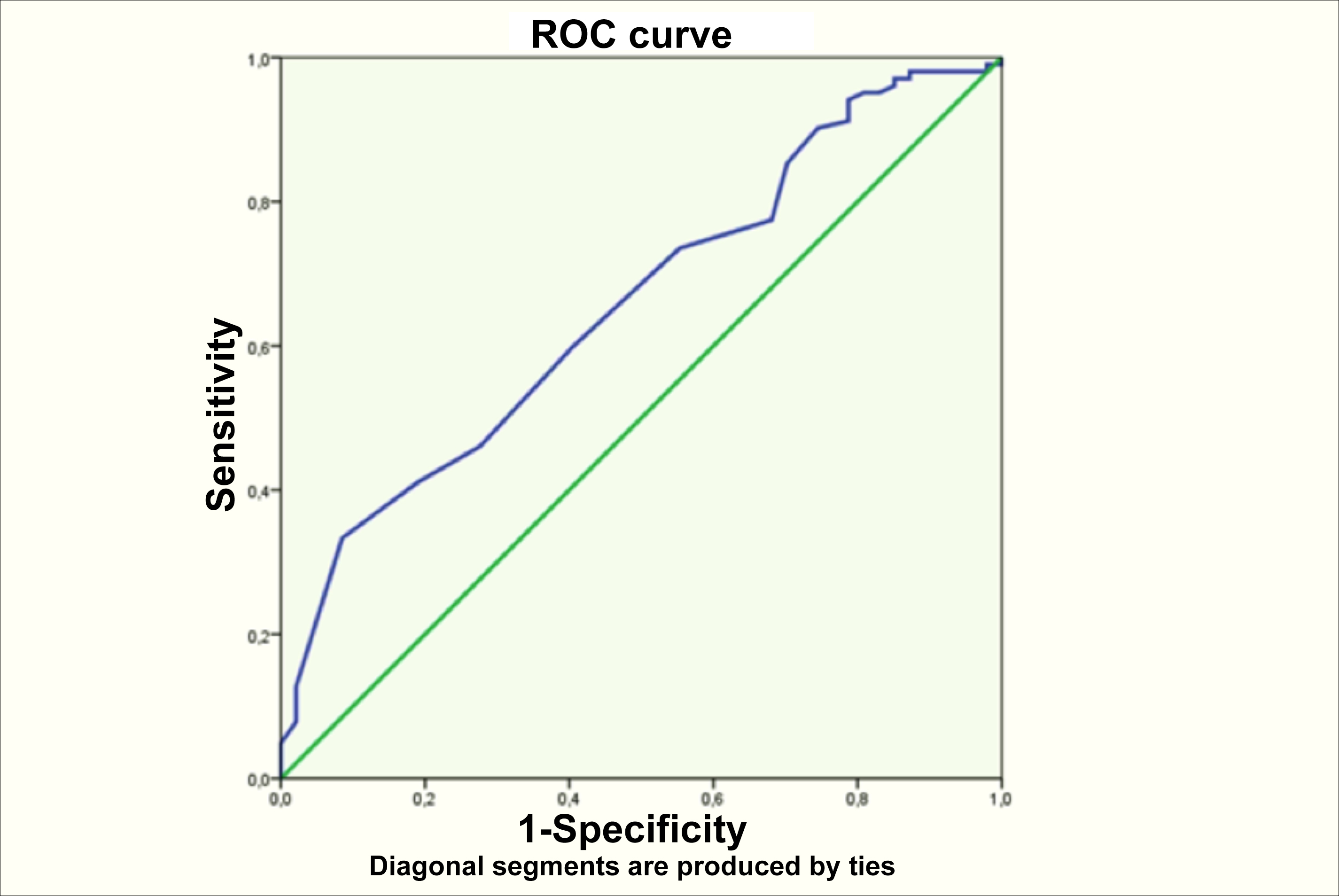 Figure 1: ROC curve of prealbumin for COVID-19 mortality.
Figure 1: ROC curve of prealbumin for COVID-19 mortality.
Median ages were 63 and 68; percentages of males were 74 and 74 in other studies conducted with large populations of patients.16,17 When viewed from this aspect, the present findings are compatible with the similar studies partaking in the literature. Older age is a risk factor for mortality in all of these studies as the same result was seen in the present study.
Although the p-value was very close to significance for NIMV (p=0.051), both NIMV and HFNC treatments were found not to be associated with mortality in our study. Controversially, the 90-day mortality rate was lower for the group treated with HFNC than the group treated with NIMV in another study, which was conducted with 4,244 critically ill COVID-19 patients.16 The authors consider that fewer number of patients who received these therapies in this study group (26 for NIMV, 21 for HFNC) could be the reason for this different result. Invasive mechanical ventilation, on the other hand, was very strongly associated with mortality as the same result can be seen in all of the beforementioned studies.
Among laboratory test results, elevated potassium, uric acid, CRP, procalcitonin, and decreased prealbumin levels were found to be associated with mortality in this study; whereas, no relationship was found between mortality and sodium, D-dimer, sedimentation, and duration of intubation. In a review in which 26 studies were analysed, lab test results associated with severe illness were determined as high lactate dehydrogenase (LDH), low lymphocyte and thrombocyte counts; whereas, tests associated with mortality were found as low CD3+ and CD8+ cell counts, higher D-dimer versus lower D-dimer, hematuria, proteinuria, and high creatinine.18 In another meta-analysis, elevated levels of white blood cell (WBC), ALT, AST, creatinine, LDH, myoglobin, cardiac troponin I, D-dimer, and acute phase reactants such as CRP, PCT, IL-6, Ferritin and decreased levels of albumin, hemoglobin, platelet and lymphocyte counts were significantly associated with fatal or severe COVID-19.19 Surprisingly, D-dimer and sedimentation levels were not associated with mortality in this study. The present study group consisted of patients with severe COVID-19, thus these levels could be high in all patients disabling us to discriminate mortal from non-mortal. On the other hand, elevated K, UA, and decreased prealbumin levels are not among the “famous” factors that are associated with mortality in patients with COVID-19. Thus, the authors consider that these analyses would be useful for the upcoming studies.
When the literature were searched, the authors, could not find much study investigating the role of prealbumin in patients with COVID-19. A meta-analysis, in which 19 studies were investigated, revealed that decreased serum prealbumin concentrations were significantly associated with increased severity and mortality for COVID-19, although in two of these studies association was not statistically significant.14 In another study analysing the abnormal liver-related biomarkers in COVID-19 patients, it was found that hypoprealbuminemia independently predicts adverse outcomes.7 In a letter to the editor, the authors made a literature search and found out that prealbumin levels were significantly lower in patients with severe illness than the patients with the milder disease.20 However, all of these studies focused on the predictive value of prealbumin on all patient populations, not only the patients followed up in ICU with COVID-19 in terms of disease severity and mortality. This study has been the first study that evaluates the predictive value of prealbumin in patients with only severe disease (ICU patients), as far as it is known.
In a study in which prealbumin and CRP levels of 31 patients with COVID-19 and 51 patients without COVID-19 but with symptoms of COVID-19 were compared, serum prealbumin levels were significantly lower in COVID-19 patients at admission to hospital compared with the control group, although the difference in serum CRP concentrations does not reach statistical significance between the groups. According to these results, the authors considered that prealbumin could act as a surrogate biomarker for the early triage of COVID-19. In addition to this, the authors performed a ROC analysis and the cut-off value of prealbumin for discriminating patients with COVID-19 from the patients without COVID-19 was found as 0.17 g/L with a sensitivity of 0.903, and a specificity of 0.863.21 This is the only study the authors could find in the literature in which ROC analysis for prealbumin was performed. The main differences from this study are that their study population was smaller than the present and they performed this analysis to determine the predictive value of prealbumin for early triage of COVID-19; whereas, the present authors tried to analyse the predictive efficiency of prealbumin for the patients with severe COVID-19 in terms of mortality. Besides, their cut-off value (0.17 g/L) was twice as this study cut-off value (0.085 g/L). This difference may be explained with the difference of study populations. They included all COVID-19 patients in their study irrespective of severity; while the present study included only patients with severe illness.
CONCLUSION
Prealbumin levels, that were studied at the time of admission to ICU, were found significantly lower for nonsurvivor patients in this study. Mortality risk was approximately twice higher for the patients who had a prealbumin level below the cut-off value of 0.085 g/L. According to these results, this protein can be stated as a good predictor of mortality in patients with severe COVID-19. The authors consider that prealbumin, as a known biomarker for inflammation, liver injury, and nutrition, deserves more significance in the daily practice of ICU and the patients with lower prealbumin levels at the time of admission to ICU must be monitored more carefully.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
ETHICAL APPROVAL:
Ethical approval was obtained from Sakarya University Ethical Committee approval on 27 April 2020, document No. 187.
PATIENTS’ CONSENT:
Consents for participation in this study were not obtained from the patients as the data were collected from the medical record system of the Hospital without disclosing the identity of the participants.
AUTHORS’ CONTRIBUTION:
KI: Designing and drafting the work.
ACG: Analysis and interpretation of data for the work.
DC: Drafting the work.
IY: Data curation, methodology.
ABG, SY: Final approval of the version to be published.
REFERENCES
- Vieira M, Saraiva MJ. Transthyretin: A multifaceted protein. Biomol Concepts 2014; 5(1):45-54. doi: 10.1515/bmc-2013-0038.
- Park GY, Jamerlan A, Shim KH, An SSA. Diagnostic and treatment approaches ınvolving transthyretin in amyloidogenic diseases. Int J Mol Sci 2019; 20(12):2982. doi.org/10.3390/ijms20122982.
- Website [Internet]. [cited 2021 Mar 18]. Available from: https://doi.org/10.1016/j.amjmed.2015.03.032
- Keller U. Nutritional laboratory markers in malnutrition. J Clin Med Res 2019; 8(6):775. doi: 10.3390/jcm8060775.
- Beck FK, Rosenthal TC. Prealbumin: A marker for nutritional evaluation. Am Fam Physician 2002; 65(8):1575-8.
- Dellière S, Cynober L. Is transthyretin a good marker of nutritional status? Clin Nutr 2017; 36(2):364-70. doi: 10.1016/j.clnu.2016.06.004.
- Li T, Guo Y, Zhuang X, Huang L, Zhang X, Wei F, et al. Abnormal liver-related biomarkers in COVID-19 patients and the role of prealbumin. Saudi J Gastroenterol 2020; 26(5):272-8. doi: 10.4103/sjg.SJG_239_20.
- Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020; 368:m1091. doi: 10.1136/bmj.m1091.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382(18):1708-20. DOI: 10.1056/NEJMoa 2002032
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-ınfected pneumonia in Wuhan, China. JAMA 2020; 323(11):1061-9. doi: 10.1001/jama.2020.1585.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395(10229):1054-62. doi: 10.1016/S0140- 6736(20)30566-3.
- Sun J, Aghemo A, Forner A, Valenti L. COVID-19 and liver disease. Liver Int 2020; 40(6):1278-81. doi: 10.1111/liv. 14470.
- Zhang C, Shi L, Wang FS. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol Hepatol 2020; 5(5):428-30. doi: 10.1016/S2468-1253(20)30057-1.
- Zinellu A, Mangoni AA. Serum prealbumin concentrations, COVID-19 severity, and mortality: A systematic review and meta-analysis. Front Med 2021; 8:638529. doi: 10.3389/ fmed.2021.638529.
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients ınfected with SARS-CoV-2 admitted to ıcus of the lombardy region, Italy. JAMA 2020; 323(16):1574-81. doi: 10.1001/jama.2020.5394.
- COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study. Intensive Care Med 2021; 47(1):60-73.
- Haase N, Plovsing R, Christensen S, Poulsen LM, Brøchner AC, Rasmussen BS, et al. Characteristics, interventions, and longer term outcomes of COVID-19 ICU patients in Denmark-A nationwide, observational study. Acta Anaesthesiol Scand 2021; 65(1):68-75. doi: 10.1111/aas.13701.
- Setiati S, Harimurti K, Safitri ED, Ranakusuma RW, Saldi SRF, Azwar MK, et al. Risk factors and laboratory test results associated with severe illness and mortality in COVID-19 patients: A systematic review. Acta Med Indones 2020; 52(3):227-45.
- Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin Chem Lab Med 2020; 58(7):1021-8. doi: 10.1515/cclm-2020-0369.
- Mattiuzzi C, Lippi G. Serum prealbumin values predict the severity of coronavirus disease 2019 (COVID-19). J Med Virol 2021; 93(2):620-1. doi: 10.1002/jmv.26385.
- Guo XL, Zhang Y, Zeng YH, Zhao FY, Liu WP, Xiao L, et al. Serum prealbumin deserves more significance in the early triage of COVID-19 patients. Clin Chem Lab Med 2020; 58(10):e209-11. doi: 10.1515/cclm-2020-0663.