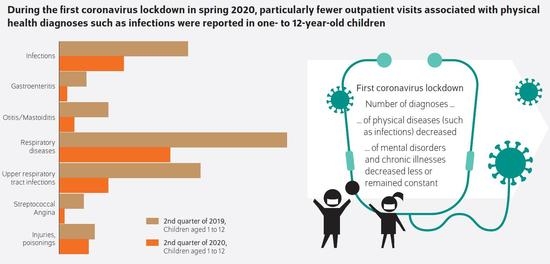
COVID-19 Associated Contact Restrictions in Germany: Marked Decline in Children’s Outpatient Visits for Infectious Diseases without Increasing Visits for Mental Health Disorders
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Levy, E.R.; Blumenthal, J.; Chiotos, K. Coronavirus disease 2019 in children. Curr. Opin. Infect. Dis. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Koletzko, B.; Holzapfel, C.; Schneider, U.; Hauner, H. Lifestyle and body weight consequences of the COVID-19 pandemic in children: Increasing disparity. Ann. Nutr. Metab. 2021, 77, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Censi, L.; Ruggeri, S.; Galfo, M.; Buonocore, P.; Roccaldo, R. Eating behaviour, physical activity and lifestyle of Italian children during lockdown for COVID-19. Int. J. Food Sci. Nutr. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Schranz, M.; Ullrich, A.; Rexroth, U.; Hamouda, O.; Schaade, L.; Diercke, M.; Boender, S. Die Auswirkungen der COVID-19-Pandemie und assoziierter PublicHealth-Maßnahmen auf andere meldepflichtige Infektionskrankheiten in Deutschland. Epid. Bull. 2021, 7, 3–7. [Google Scholar]
- Pelletier, J.H.; Rakkar, J.; Au, A.K.; Fuhrman, D.; Clark, R.S.B.; Horvat, C.M. Trends in US Pediatric Hospital Admissions in 2020 Compared With the Decade Before the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2037227. [Google Scholar] [CrossRef] [PubMed]
- Indolfi, G.; Stivala, M.; Lenge, M.; Naderi, R.D.; McIntosh, J.; Llandrich, R.C.; Gannon, J.; McGreevy, K.S.; Trapani, S.; Miettinen, P.; et al. Impact of SARS-CoV-2 Pandemic and Strategies for Resumption of Activities During the Second Wave of the Pandemic: A Report From Eight Paediatric Hospitals From the ECHO Network. Front. Public Health 2021, 9, 630168. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.; Krause, M.C.; Pethe, K.; Caddle, S.; Finkel, M.; Glassman, M.E.; Kostacos, C.; Robbins-Milne, L.; Bracho-Sanchez, E.; Soren, K.; et al. Managing the COVID-19 Pandemic Using Quality Improvement Principles: A New York City Pediatric Primary Care Experience. Pediatr. Qual. Saf. 2021, 6, e402. [Google Scholar] [CrossRef] [PubMed]
- Bundesministerium-für-Gesundheit. Mitglieder und Versicherte der Gesetzlichen Krankenversicherung (GKV); Bundesministerium für Gesundheit: Berlin, Germany, 2021. [Google Scholar]
- Statista-GmbH. Anzahl der Geburten in Deutschland von 1991 bis 2020; Statista GmbH: Hamburg, Germany, 2021. [Google Scholar]
- Bundesinstitut-für-Arzneimittel-und-Medizinprodukte. Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme; German Modification, ICD-10-GM Version 2021; Bundesinstitut für Arzneimittel und Medizinprodukte: Bonn, Germany, 2021. [Google Scholar]
- Verband-der-Ersatzkassen-e.V. vdek-Basisdaten des Gesundheitswesens 2021; 25. Auflage; Verband der Ersatzkassen e.V.: Berlin, Germany, 2021. [Google Scholar]
- Bundesministerium für Familie, Senioren, Frauen und Jugend. Kindertagesbetreuung Kompakt; Bundesministerium für Familie, Senioren, Frauen und Jugend: Berlin, Germany, 2017. [Google Scholar]
- Angoulvant, F.; Ouldali, N.; Yang, D.D.; Filser, M.; Gajdos, V.; Rybak, A.; Guedj, R.; Soussan-Banini, V.; Basmaci, R.; Lefevre-Utile, A.; et al. Coronavirus Disease 2019 Pandemic: Impact Caused by School Closure and National Lockdown on Pediatric Visits and Admissions for Viral and Nonviral Infections—A Time Series Analysis. Clin. Infect. Dis. 2021, 72, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Hölling, H.; Schlack, R.; Löffler, C.; Hurrelmann, K.; Otto, C. Quality of Life and Mental Health in Children and Adolescents during the First Year of the COVID-19 Pandemic in Germany: Results of a Two-Wave Nationally Representative Study (5 March 2021). SSRN Unreviewed Preprint. 2021. Available online: https://ssrn.com/abstract=3798710 (accessed on 10 July 2021).
- Krass, P.; Dalton, E.; Doupnik, S.K.; Esposito, J. US Pediatric Emergency Department Visits for Mental Health Conditions During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e218533. [Google Scholar] [CrossRef] [PubMed]
- Cooper, K.; Hards, E.; Moltrecht, B.; Reynolds, S.; Shum, A.; McElroy, E.; Loades, M. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. J. Affect. Disord. 2021, 289, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Cappa, C.; Jijon, I. COVID-19 and violence against children: A review of early studies. Child Abus. Negl. 2021, 116, 105053. [Google Scholar] [CrossRef] [PubMed]
- Sachser, C.; Olaru, G.; Pfeiffer, E.; Brähler, E.; Clemens, V.; Rassenhofer, M.; Witt, A.; Fegert, J.M. The Immediate Impact of Lockdown Measures on Mental Health and Couples’ Relationships during the COVID-19 Pandemic-Results of a Representative Population Survey in Germany. Soc. Sci. Med. 2021, 278, 113954. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, G.J.; Siflinger, B.M. The Effects of Day Care on Health during Childhood: Evidence by Age; Institute for Evaluation of Labour Market and Education Policy: Uppsala, Sweden, 2020. [Google Scholar]
- Heinrich, J.; Koletzko, B. Kinderbetreuung und Kindergesundheit bei unter Dreijährigen. Mon. Kinderheilkd. 2008, 156, 562–568. [Google Scholar] [CrossRef]
- Stiftung-Kindergesundheit. Kinder Gesund Betreut: Curriculum zur Gesundheitsförderung in der Kinderbetreuung für Kinder unter drei Jahren Hannover; Friedrich Verlag: Hannover, Germany, 2015. [Google Scholar]
- Gesetz zur Weiterentwicklung der Qualität und zur Teilhabe in der Kindertagesbetreuung. Bundesgesetzblatt 2018, 19, 2696–2699.
- Ponka, A.; Nurmi, T.; Salminen, E.; Nykyri, E. Infections and other illnesses of children in day-care centers in Helsinki. I: Incidences and effects of home and day-care center variables. Infection 1991, 19, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Grosch, C.; Niebsch, G. Vergleich des Gesundheitszustandes von Kleinkindern, die in der Krippe bzw. ausschließlich in der Familie erzogen werden. In Hygiene des Kindes- und Jugendalters, Bd 10, Beurteilung von Gesundheit und Entwicklung und die Prophylaktische Betreuung in der Frühen Kindheit; Schmidt-Kolmer, E., Niebsch, G., Tonkowa-Jampolskaja, R., Eds.; Volk und Gesundheit: Berlin, Germany, 1987; pp. 78–82. [Google Scholar]
- Abrahamsen, S.A.; Ginja, R.; Riise, J. School Health Programs: Education, Health, and Welfare Dependency of Young; University of Bergen: Bergen, Norway, 2019; pp. 1–21. [Google Scholar]



| Age | 1–2 Years | 3–5 Years | 6–10 Years | 11–12 Years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | 2019 | 2020 | P CI | 2019 | 2020 | P CI | 2019 | 2020 | P CI | 2019 | 2020 | P CI |
| Raw means ± SD | OLS | Raw means ± SD | OLS | Raw means ± SD | OLS | Raw means ± SD | OLS | |||||
| Children | 1,529,063 | 1,617,556 | 2,194,429 | 2,241,386 | 3,278,228 | 3,351,685 | 1,289,184 | 1,288,880 | ||||
| Outpatient visits per child | 0.8446 ± 0.4417 | 0.7070 ± 0.4939 | <0.0001 (−0.14, −0.13) | 0.7430 ± 0.4867 | 0.5981 ± 0.5210 | <0.0001 (−0.15, −0.14) | 0.6654 ± 0.5077 | 0.5513 ± 0.5277 | <0.0001 (−0.12, −0.11) | 0.6377 ± 0.5147 | 0.5214 ± 0.5317 | <0.0001 (−0.12, −0.11) |
| Infections | ||||||||||||
| Infectious and parasitic diseases | 0.2297 ± 0.4206 | 0.1060 ± 0.3087 | <0.0001 (−0.13, −0.12) | 0.1730 ± 0.3783 | 0.0713 ± 0.2573 | <0.0001 (−0.10, −0.10) | 0.1369 ± 0.3437 | 0.0759 ± 0.2648 | <0.0001 (−0.06, −0.06) | 0.1096 ± 0.3123 | 0.0621 ± 0.2413 | <0.0001 (−0.05, −0.05) |
| Infectious intestinal diseases | 0.0512 ± 0.2205 | 0.0149 ± 0.1213 | <0.0001 (−0.04, −0,04) | 0.0383 ± 0.1920 | 0.0089 ± 0.0939 | <0.0001 (−0.03, −0.03) | 0.0274 ± 0.1632 | 0.0073 ± 0.0849 | <0.0001 (−0.02, −0.02) | 0.0235 ± 0.1515 | 0.0067 ± 0.0815 | <0.0001 (−0.02, −0.02) |
| Diseases of the middle ear and mastoid | 0.0773 ± 0.2670 | 0.0172 ± 0.1301 | <0.0001 (−0.06, −0.06) | 0.1002 ± 0.3003 | 0.0280 ± 0.1650 | <0.0001 (−0.07, −0.07) | 0.0416 ± 0.1997 | 0.0151 ± 0.1218 | <0.0001 (−0.03, −0.03) | 0.0207 ± 0.1423 | 0.0077 ± 0.0873 | <0.0001 (−0.01, −0.01) |
| Diseases of the respiratory system | 0.3730 ± 0.4836 | 0.1335 ± 0.3401 | <0.0001 (−0.24, −0.23) | 0.3230 ± 0.4676 | 0.1429 ± 0.3500 | <0.0001 (−0.19, −0.18) | 0.2393 ± 0.4267 | 0.1390 ± 0.3460 | <0.0001 (−0.10, −0.10) | 0.2174 ± 0.4125 | 0.1322 ± 0.3387 | <0.0001 (−0.09, −0.08) |
| Acute upper respiratory tract infections | 0.2699 ± 0.4439 | 0.0889 ± 0.2847 | <0.0001 (−0.18, −0.18) | 0.2084 ± 0.4061 | 0.0679 ± 0.2516 | <0.0001 (−0.14, −0.14) | 0.1344 ± 0.3411 | 0.0506 ± 0.2192 | <0.0001 (0.08, −0.08) | 0.1089 ± 0.3115 | 0.0365 ± 0.1874 | <0.0001 (−0.07, −0.07) |
| Streptococcus Angina | 0.0252 ± 0.1566 | 0.0069 ± 0.0825 | <0.0001 (−0.02, −0.02) | 0.0381 ± 0.1915 | 0.0082 ± 0.0902 | <0.0001 (−0.03, −0.03) | 0.0288 ± 0.1671 | 0.0061 ± 0.0780 | <0.0001 (−0.02, −0.02) | 0.0199 ± 0.1395 | 0.0044 ± 0.0659 | <0.0001 (−0.02, −0.02) |
| Injuries | ||||||||||||
| Injuries | 0.0402 ± 0.1965 | 0.0362 ± 0.1869 | <0.0001 (−0.00, −0.00) | 0.0387 ± 0.1929 | 0.0377 ± 0.1904 | <0.0001 (−0.01, −0.01) | 0.0434 ± 0.2039 | 0.0347 ± 0.1830 | <0.0001 (−0.01, −0.01) | 0.0564 ± 0.2306 | 0.0377 ± 0.1904 | <0.0001 (−0.02, −0.02) |
| Chronic physical diseases | ||||||||||||
| Diabetes | 0.0002 ± 0.0124 | 0.0001 ± 0.0114 | n.s. (−0.00, 0.00) | 0.0005 ± 0.0234 | 0.0005 ± 0.0232 | n.s. (−0.00, −0.00) | 0.0015 ± 0.0392 | 0.0015 ± 0.0381 | 0.0024 (−0.00, −0.00) | 0.0028 ± 0.0532 | 0.0026 ± 0.0510 | 0.0005 (−0.00, −0.00) |
| Celiac disease | 0.0005 ± 0.0221 | 0.0004 ± 0.0206 | n.s. (−0.00, 0.00) | 0.0011 ± 0.0331 | 0.0009 ± 0.0307 | <0.0001 (−0.00, −0.00) | 0.0018 ± 0.0428 | 0.0016 ± 0.0394 | <0.0001 (−0.00, −0.00) | 0.0022 ± 0.0465 | 0.0019 ± 0.0430 | <0.0001 (−0.00, −0.00) |
| Hay fever | 0.0033 ± 0.0572 | 0.0023 ± 0.0479 | <0.0001 (−0.00, −0.00) | 0.0138 ± 0.1167 | 0.0140 ± 0.1176 | n.s. (−0.00, 0.00) | 0.0444 ± 0.2061 | 0.0431 ± 0.2032 | <0.0001 (−0.00, −0.00) | 0.0662 ± 0.2486 | 0.0609 ± 0.2391 | <0.0001 (−0.01, −0.01) |
| Mental and Behavioral Disorders | ||||||||||||
| All mental and behavioral disorders | 0.0670 ± 0.2500 | 0.0628 ± 0.2426 | <0.0001 (−0.01, −0.00) | 0.1658 ± 0.3719 | 0.1513 ± 0.3583 | <0.0001 (−0.02, −0.01) | 0.1960 ± 0.3969 | 0.1717 ± 0.3771 | <0.0001 (−0.03, −0.02) | 0.1595 ± 0.3661 | 0.1389 ± 0.3458 | <0.0001 (−0.02, −0.02) |
| Neurotic, stress and somatoform disorders | 0.0061 ± 0.0780 | 0.0058 ± 0.0758 | <0.0001 (−0.00, −0.00) | 0.0109 ± 0.1038 | 0.0097 ± 0.0982 | <0.0001 (−0.00, −0.00) | 0.0235 ± 0.1515 | 0.0205 ± 0.1418 | <0.0001 (−0.00, −0.00) | 0.0336 ± 0.1803 | 0.0282 ± 0.1656 | <0.0001 (−0.01, −0.01) |
| Personality and behavioral disorders | 0.0012 ± 0.0344 | 0.0011 ± 0.0333 | n.s. (−0.00, −0.00) | 0.0042 ± 0.0644 | 0.0036 ± 0.0598 | <0.0001 (−0.00, −0.00) | 0.0066 ± 0.0812 | 0.0053 ± 0.0729 | <0.0001 (−0.00, −0.00) | 0.0069 ± 0.0826 | 0.0055 ± 0.0741 | <0.0001 (−0.00, −0.00) |
| Developmental Disabilities | 0.0481 ± 0.2140 | 0.0449 ± 0.2072 | <0.0001 (−0.00, −0.00) | 0.1381 ± 0.3450 | 0.1264 ± 0.3323 | <0.0001 (−0.01, −0.01) | 0.1366 ± 0.3434 | 0.1197 ± 0.3246 | <0.0001 (−0.02, −0.02) | 0.0820 ± 0.2744 | 0.0727 ± 0.2596 | <0.0001 (−0.01, −0.01) |
| Behavioral and emotional disorders with onset in childhood & adolescence. | 0.0124 ± 0.1107 | 0.0119 ± 0.1085 | <0.0001 (−0.00, −0.00) | 0.0353 ± 0.1846 | 0.0323 ± 0.1768 | <0.0001 (−0.00, −0.00) | 0.0842 ± 0.2777 | 0.0744 ± 0.2624 | <0.0001 (−0.01, −0.01) | 0.0936 ± 0.2913 | 0.0832 ± 0.2762 | <0.0001 (−0.01, −0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barschkett, M.; Koletzko, B.; Spiess, C.K. COVID-19 Associated Contact Restrictions in Germany: Marked Decline in Children’s Outpatient Visits for Infectious Diseases without Increasing Visits for Mental Health Disorders. Children 2021, 8, 728. https://doi.org/10.3390/children8090728
Barschkett M, Koletzko B, Spiess CK. COVID-19 Associated Contact Restrictions in Germany: Marked Decline in Children’s Outpatient Visits for Infectious Diseases without Increasing Visits for Mental Health Disorders. Children. 2021; 8(9):728. https://doi.org/10.3390/children8090728
Chicago/Turabian StyleBarschkett, Mara, Berthold Koletzko, and C. Katharina Spiess. 2021. "COVID-19 Associated Contact Restrictions in Germany: Marked Decline in Children’s Outpatient Visits for Infectious Diseases without Increasing Visits for Mental Health Disorders" Children 8, no. 9: 728. https://doi.org/10.3390/children8090728