Exploring and Monitoring the Reasons for Hesitation with COVID-19 Vaccine Based on Social-Platform Text and Classification Algorithms
Abstract
:1. Introduction
1.1. Background
1.2. Literature Review
1.3. Objectives and Methodology
1.4. Results and Contributions
2. Methods
2.1. Data Collection
2.2. Structuring COVID-19 Vaccine Hesitancy Reasons
2.3. Text Preprocessing
2.4. Training Classifier
3. Results
4. Conclusions
5. Contributions and Future Work
5.1. Academic Contribution
5.2. Practical Significance
5.3. Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Domachowske, J.B.; Suryadevara, M. Practical approaches to vaccine hesitancy issues in the United States 2013. Hum. Vaccines 2013, 9, 2654–2657. [Google Scholar] [CrossRef] [Green Version]
- Kling, S. Vaccine hesitancy: May i refuse to treat the child? Curr. Allergy Clin. Immunol. 2020, 33, 48–51. [Google Scholar]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef] [PubMed]
- Feleszko, W.; Lewulis, P.; Czarnecki, A.; Waszkiewicz, P. Flattening the Curve of COVID-19 Vaccine Rejection—An International Overview. Vaccines 2021, 9, 44. [Google Scholar] [CrossRef] [PubMed]
- Aygun, E.; Tortop, H. Investigation of Parents’ Vaccine Hesitation Levels and Reasons of Vaccine Refusal. Guncel Pediatri.-J. Curr. Pediatr. 2020, 18, 300–316. [Google Scholar]
- Charron, J.; Gautier, A.; Jestin, C. Influence of information sources on vaccine hesitancy and practices. Med. Mal. Infect. 2020, 50, 727–733. [Google Scholar] [CrossRef]
- Baumgaertner, B.; Ridenhour, B.J.; Justwan, F.; Carlisle, J.E.; Miller, C.R. Risk of disease and willingness to vaccinate in the United States: A population-based survey. PLoS Med. 2020, 17, e1003354. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, L.; Baumgartner, J.N.; Moses, S.; Ngadaya, E.; Mfinanga, S.G.; Ostermann, J. Parental concerns and uptake of childhood vaccines in rural Tanzania-a mixed methods study. BMC Public Health 2020, 20, 1573. [Google Scholar] [CrossRef]
- Beraud, G. Shortages without Frontiers: Antimicrobial Drug and Vaccine Shortages Impact Far Beyond the Individual! Front. Med. 2021, 8, 593712. [Google Scholar] [CrossRef]
- Kilincarslan, M.G.; Sarigül, B.; Toraman, C.; Melih, E. Development of Valid and Reliable Scale of Vaccine Hesitancy in Turkish Language. Konuralp Tip Derg. 2020, 12, 420–429. [Google Scholar] [CrossRef]
- Guidry, J.P.; DAustin, L.L.; O’Donnell, N.H.; Coman, I.A.; Lovari, A.; Messner, M. Tweeting the flushot: Beliefs, Barriers, and Threats During Different Periods of the 2018 to 2019 Flu Season. J. Prim. Care Community Health 2020, 11, 2150132720932722. [Google Scholar] [CrossRef]
- Basch, C.H.; Meleo-Erwin, Z.; Fera, J.; Jaime, C.; Basch, C.E. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Hum. Vaccines Immunother. 2021, 17, 2373–2377. [Google Scholar] [CrossRef] [PubMed]
- Moyer-Guse, E.; Robinson, M.J.; Mcknight, J. The Role of Humor in Messaging about the MMR Vaccine. J. Health Commun. 2018, 23, 514–522. [Google Scholar] [CrossRef]
- Onnela, J.; Landon, B.E.; Kahn, A.; Ahmed, D.; Verma, H.; O’Malley, A.J.; Bahl, S.; Sutter, R.W.; Christakis, N.A. Polio vaccine hesitancy in the networks and neighborhoods of Malegaon, India. Soc. Sci. Med. 2016, 153, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. No Populations Left Behind: Vaccine Hesitancy and Equitable Diffusion of Effective COVID-19 Vaccines. J. Gen. Intern. Med. 2021, 36, 2130–2133. [Google Scholar] [CrossRef]
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X.R. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef] [PubMed]
- Eguia, H.; Vinciarelli, F.; Bosque-Prous, M.; Kristensen, T.; Saigí-Rubió, F. Spain’s Hesitation at the Gates of a COVID-19 Vaccine. Vaccines 2021, 9, 170. [Google Scholar] [CrossRef]
- Preto, C.; de Mello, A.M.; Maluf, E.M.C.P.; Krainski, E.T.; Graeff, G.; de Sousa, G.A.; da Silva, L.R.; da Costa-Ribeiro, M.C.V.; Buffon, M.D.M.; Shimakura, S.E. Vaccination coverage and adherence to a dengue vaccination program in the state of Parana, Brazil. Vaccine 2021, 39, 711–719. [Google Scholar] [CrossRef]
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef]
- Gunes, N. Parents’ Perspectives about Vaccine Hesitancies and Vaccine Rejection, in the West of Turkey. J. Pediatr. Nurs. 2020, 53, E186–E194. [Google Scholar] [CrossRef] [PubMed]
- Krasnicka, J.; Krajewska-Kulak, E.; Klimaszewska, K.; Cybulski, M.; Guzowski, A.; Kowalewska, B.; Jankowiak, B.; Rolka, H.; Doroszkiewicz, H.; Kulak, W. Mandatory and recommended vaccinations in Poland in the views of parents. Hum. Vaccines Immunother. 2018, 14, 2884–2893. [Google Scholar] [CrossRef] [Green Version]
- Bradshaw, A.S.; Treise, D.; Shelton, S.S.; Cretul, M.; Peek, D. Propagandizing anti-vaccination: Analysis of Vaccines Revealed documentary series. Vaccine 2020, 38, 2058–2069. [Google Scholar] [CrossRef] [PubMed]
- Tandy, C.B.; Tree, J.M.J. Attitudes of East Tennessee residents towards general and pertussis vaccination: A qualitative study. BMC Public Health 2021, 21, 446. [Google Scholar] [CrossRef] [PubMed]
- Goss, M.D.; Temte, J.L.; Barlow, S.; Temte, E.; Chen, G. An assessment of parental knowledge, attitudes, and beliefs regarding influenza vaccination. Vaccine 2020, 38, 1565–1571. [Google Scholar] [CrossRef] [PubMed]
- Motta, M. Can a COVID-19 vaccine live up to Americans’ expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc. Sci. Med. 2021, 272, 113642. [Google Scholar] [CrossRef]
- Figueroa-Parra, G.; Esquivel-Valerio, J.A.; Santoyo-Fexas, L.; Moreno-Salinas, A.; Gamboa-Alonso, C.M.; De Leon-Ibarra, A.L.; Galarza-Delgado, D.A. Knowledge and attitudes about influenza vaccination in rheumatic diseases patients. Hum. Vaccines Immunother. 2021, 17, 1420–1425. [Google Scholar] [CrossRef] [PubMed]
- Hopp, F.R.; Fisher, J.T.; Cornell, D.; Huskey, R.; Weber, R. The extended Moral Foundations Dictionary (eMFD): Development and applications of a crowd-sourced approach to extracting moral intuitions from text. Behav. Res. Methods 2021, 53, 232–246. [Google Scholar] [CrossRef]
- Van Buynder, P.G.; Van Buynder, J.L.; Menton, L.; Thompson, G.; Sun, J. Antigen specific vaccine hesitancy in pregnancy. Vaccine 2019, 37, 2814–2820. [Google Scholar] [CrossRef]
- Clarke, R.M.; Paterson, P.; Sirota, M. Determinants of satisfaction with information and additional information-seeking behaviour for the pertussis vaccination given during pregnancy. Vaccine 2019, 37, 2712–2720. [Google Scholar] [CrossRef]
- Bouchez, M.; Ward, J.K.; Bocquier, A.; Benamouzig, D.; Peretti-Watel, P.; Seror, V.; Verger, P. Physicians’ decision processes about the HPV vaccine: A qualitative study. Vaccine 2021, 39, 521–528. [Google Scholar] [CrossRef]
- Ryan, K.A.; Filipp, S.L.; Gurka, M.J.; Zirulnik, A.; Thompson, L.A. Understanding influenza vaccine perspectives and hesitancy in university students to promote increased vaccine uptake. Heliyon 2019, 5, e02604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, R.; Fintan, B. Fear, knowledge, and vaccination behaviors among women in Northern Nigeria. Hum. Vaccines Immunother. 2020, 16, 2438–2448. [Google Scholar] [CrossRef]
- Baxter, A.L.; Cohen, L.L.; Burton, M.; Mohammed, A.; Lawson, M.L. The number of injected same-day preschool vaccines relates to preadolescent needle fear and HPV uptake. Vaccine 2017, 35, 4213–4219. [Google Scholar] [CrossRef] [PubMed]
- Tavoschi, L.; Quattrone, F.; D’Andrea, E.; Ducange, P.; Vabanesi, M.; Marcelloni, F.; Lopalco, P.L. Twitter as a sentinel tool to monitor public opinion on vaccination: An opinion mining analysis from September 2016 to August 2017 in Italy. Hum. Vaccines Immunother. 2020, 16, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Chau, M.; Li, T.M.H.; Wong, P.W.C.; Xu, J.J.; Yip, P.S.F.; Chen, H. Finding People with Emotional Distress in Online Social Media: A Design Combining Machine Learning and Rule-Based Classification. Mis Q. 2020, 44, 933–955. [Google Scholar] [CrossRef]
- Yildirim, E. Compulsory Vaccination and the Turkish Constitutional Court. Eur. J. Health Law 2020, 27, 476–494. [Google Scholar] [CrossRef]
- Akwataghibe, N.N.; Ogunsola, E.A.; Broerse, J.E.W.; Popoola, O.A.; Agbo, A.I.; Dieleman, M.A. Exploring Factors Influencing Immunization Utilization in Nigeria-A Mixed Methods Study. Front. Public. Health 2019, 7, 392. [Google Scholar] [CrossRef]
- Kumar, D.; Chandra, R.; Mathur, M.; Samdariya, S.; Kapoor, N. Vaccine hesitancy: Understanding better to address better. Isr. J. Health Policy Res. 2016, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Thaker, J. The Persistence of Vaccine Hesitancy: COVID-19 Vaccination Intention in New Zealand. J. Health Commun. 2021, 26, 104–111. [Google Scholar] [CrossRef]
- Kennedy, J. Vaccine Hesitancy: A Growing Concern. Pediatr. Drugs 2020, 22, 105–111. [Google Scholar] [CrossRef]
- Townsend, M.J.; Kyle, T.K.; Stanford, F.C. COVID-19 Vaccination and Obesity: Optimism and Challenges. Obesity 2021, 29, 634–635. [Google Scholar] [CrossRef] [PubMed]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef] [PubMed]
- Slovic, P. The Perception of risk. Risk Soc. Policy 2000, 69, 112. [Google Scholar]
- Chen, Y.; Feng, J.; Chen, A.; Lee, J.E.; An, L. Risk perception of COVID-19: A comparative analysis of China and South Korea. Int. J. Disaster Risk Reduct. 2021, 61, 102373. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, L.C.; Soveri, A.; Lewandowsky, S.; Karlsson, L.; Karlsson, H.; Nolvi, S.; Karukivi, M.; Lindfelt, M.; Antfolk, J. Fearing the disease or the vaccine: The case of COVID-19. Pers. Individ. Differ. 2021, 172, 110590. [Google Scholar] [CrossRef]
- Narayana, G.; Pradeepkumar, B.; Ramaiah, J.D.; Jayasree, T.; Yadav, D.L.; Kumar, B.K. Knowledge, perception, and practices towards COVID-19 pandemic among general public of India: A cross-sectional online survey. Curr. Med. Res. Pract. 2020, 10, 153–159. [Google Scholar] [CrossRef]
- Amanat, F.; Thapa, M.; Lei, T.; Ahmed, S.M.S.; Adelsberg, D.C.; Carreño, J.M.; Strohmeier, S.; Schmitz, A.J.; Zafar, S.; Zhou, J.Q.; et al. SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD, and S2. Cell 2021, 184, 3936–3948. [Google Scholar] [CrossRef]
- Quinn, S.C.; Lama, Y.; Jamison, A.; Freimuth, V.; Shah, V. Willingness of Black and White Adults to Accept Vaccines in Development: An Exploratory Study Using National Survey Data. Am. J. Health Promot. 2021, 35, 571–579. [Google Scholar] [CrossRef]
- Hayakawa, S.; Komine-Aizawa, S.; Takada, K.; Kimura, T.; Yamada, H. Anti-SARS-CoV-2 vaccination strategy for pregnant women in Japan. J. Obstet. Gynaecol. Res. 2021, 47, 1958–1964. [Google Scholar] [CrossRef]
- MacDougall, T.; Cunningham, S.; Whitney, L.; Sawhney, M. Improving pediatric experience of pain during vaccinations: A quality improvement project. Int. J. Health Care Qual. Assur. 2019, 32, 1034–1040. [Google Scholar] [CrossRef]
- Chung, E.H. Vaccine allergies. Clin. Exp. Vaccine Res. 2014, 3, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Eler, D.M.; Grosa, D.; Pola, I.; Garcia, R.; Correia, R.; Teixeira, J. Analysis of Document Pre-Processing Effects in Text and Opinion Mining. Information 2018, 9, 100. [Google Scholar] [CrossRef] [Green Version]
- Salton, G.; Fox, E.A.; Wu, H. Extended boolean information retrieval. Commun. ACM 1983, 26, 1022–1036. [Google Scholar] [CrossRef]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- Burges, C.J.C. A tutorial on Support Vector Machines for pattern recognition. Data Min. Knowl. Discov. 1998, 2, 121–167. [Google Scholar] [CrossRef]




| The Content of Texts | Example Sentences | Keep/Delete |
|---|---|---|
| Mention one or more types of reasons for the COVID-19 vaccine hesitancy (among 12 types, shown in Table 2 below). | The main reason for my hesitation is that I really don’t know whether the vaccine is safe or not, and the validity period after vaccination is only half a year, so I have no courage. I am really afraid that the side effects will be too serious. One of my colleagues got vaccinated and had a fever every two days. | Keep |
| Only express hesitation without mentioning specific reasons. | The community has told us to get vaccinated, but I’m still on the fence. | Delete |
| Personal attacks or invective. | Those who do not want to be vaccinated should die! | Delete |
| Express that someone was vaccinated, without any hesitation. | I got vaccinated last week, and I’ll be there on time for the second dose. | Delete |
| Discuss the status of the epidemic or the origin of the virus. | The epidemic is currently under control, although there are occasional clusters of cases in some areas. | Delete |
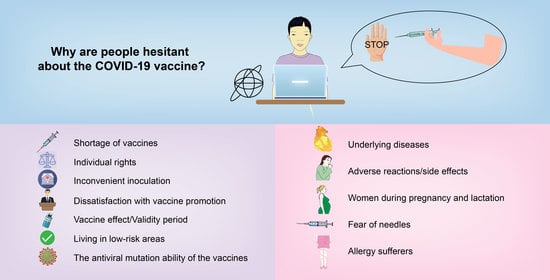
| Types | Names | Example Sentences | References |
|---|---|---|---|
| 1 | Shortage of vaccine | I received the first dose, and the second dose was always out of stock, so I was informed to reinoculate after the time. | literature [9] |
| 2 | Individual rights | Voluntary to mandatory? Vaccination or not depends on personal desire. Why morally blackmail?! | literature [36] |
| 3 | Inconvenient inoculatio | In small cities, the COVID-19 vaccines are available every working day, but not on weekends. Office workers have to take time off for the vaccine, and many of them were not vaccinated until now. | literature [37,38] |
| 4 | Dissatisfaction with vaccine promotion | (1) Is he a doctor or a social media influencer now? Shouldn’t scientists be serious about their research? (2) I thought the slogan was terrible and it didn’t convince me to get vaccinated. | literature [13,39,40] |
| 5 | Vaccine effect/Validity period | Is our vaccine safe and effective? This is the point that experts should pay attention to, right? Otherwise, when all people are vaccinated, some people will be injured. | literature [41,42] |
| 6 | Living in low-risk areas | After vaccination, it can only protect against the virus for a few months. I am in a low-risk area, so it’s truly unnecessary. | literature [43,44,45] |
| 7 | The antiviral-mutation ability of the vaccines | The current vaccine is developed against the previous virus. Is it effective against mutated viruses? | literature [46,47] |
| 8 | Underlying diseases | I truly want to get vaccinated, but I cannot. Eczema, chronic urticaria, diabetes... | literature [48] |
| 9 | Adverse reactions/side effects | My husband was vaccinated. He has a low fever for two days. He is lethargic and weak. It took him about a week to recover. | literature [42] |
| 10 | The women during pregnancy and lactation | I’m preparing for pregnancy, so I cannot get vaccinated, and then I cannot get vaccinated during breastfeeding. So I cannot get vaccinated within two years. | literature [49] |
| 11 | The fear of needles | In addition to I’m afraid of injections, nothing can stop my vaccination. | literature [33,50] |
| 12 | Allergic sufferers | I am a man of poor immunity, over the years I have allergic rhinitis, especially when the autumn, so I dare not vaccinated recently. | literature [51] |
| Classifier Name | Overall Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|
| SVM | 0.872422 | 0.871475 | 0.870964 | 0.868373 |
| LR | 0.833206 | 0.844130 | 0.832090 | 0.833418 |
| NBC | 0.746117 | 0.745158 | 0.744181 | 0.727212 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Lu, S.; Lu, C. Exploring and Monitoring the Reasons for Hesitation with COVID-19 Vaccine Based on Social-Platform Text and Classification Algorithms. Healthcare 2021, 9, 1353. https://doi.org/10.3390/healthcare9101353
Liu J, Lu S, Lu C. Exploring and Monitoring the Reasons for Hesitation with COVID-19 Vaccine Based on Social-Platform Text and Classification Algorithms. Healthcare. 2021; 9(10):1353. https://doi.org/10.3390/healthcare9101353
Chicago/Turabian StyleLiu, Jingfang, Shuangjinhua Lu, and Caiying Lu. 2021. "Exploring and Monitoring the Reasons for Hesitation with COVID-19 Vaccine Based on Social-Platform Text and Classification Algorithms" Healthcare 9, no. 10: 1353. https://doi.org/10.3390/healthcare9101353