Abstract
Study design
Focused literature review.
Objectives
Objective of the study was to perform a literature search and summarise the clinical features and prognosis of persons with spinal cord injury (SCI) infected with COVID-19 from the published articles.
Setting
India.
Methods
PubMed, CENTRAL and MEDLINE were systematically searched using specific keywords. The study assessed 2747 scientific studies involving COVID-19 and SCI for possible inclusion in a meta-analysis of SCI and SARS-COV-2. Studies involving persons with SCI who were tested positive for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in the nasopharyngeal or throat swab polymerase chain reaction were included.
Results
Out of 2747 articles, 11 articles (206 participants), including six case reports, were included in this review. Fever was the most frequently observed symptom of COVID-19 infection in the SCI population. C-reactive protein (CRP) and lymphocytopenia were common abnormal laboratory parameters. The most common radiological finding in COVID-19 infection was ground glass opacities in lung fields. Prophylactic/therapeutic anticoagulation was given in a significant number of SCI persons infected with COVID-19. Persons with SCI who were diagnosed early showed good outcomes.
Conclusions
Based on the few studies published on COVID-19 and SCI populations since 2019, this study determined fever, elevated CRP, lymphocytopenia and ground glass opacities, which indicated inflammation, compromised immune response, and lung edema, as the main clinical features of COVID-19 infection in SCI population. Though COVID-19 infection reported an increased number of deaths in few studies, a significant number of SCI populations with positive RT-PCR were treated successfully and discharged at home.
Similar content being viewed by others
Introduction
The coronavirus disease-2019 (COVID-19) is a serious health concern caused by a novel virus named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) [1]. At the time of the drafting of this review, more than 220 countries and 76,382,044 persons around the world have been diagnosed with COVID-19, and 1,702,128 persons have died from it [2]. SARS-CoV-2 was first reported in December 2019 in Wuhan municipality, China [3]. The World Health Organization declared this COVID-19/SARS-CoV-2 disease as pandemic on March 11, 2020 [2].
Though SARS-CoV-2 is a respiratory disease, studies have shown it can affect multiple organs and cause systemic diseases and blood coagulation disorders. Risk factors for severe illness in COVID-19 infection are not yet completely clear, although male gender, older persons, and those with a higher number of comorbid medical conditions appear to be at high risk for developing severe illness [4,5,6].
Persons with spinal cord injury (SCI) of any duration of injury (acute versus chronic) are at increased risk of developing respiratory complications [7]. Studies [8,9,10,11,12,13,14,15] have shown that hypertension (HTN) (prevalence in SCI, 25.9%) [9], diabetes (prevalence in SCI, 20%) [9, 10, 15], coronary artery disease (prevalence in SCI, 64%) [14, 16], overweight/obesity (prevalence in SCI, 83%) [9], urinary infections (incidence in SCI, 20%) [17] and thromboembolic disorders (incidence in SCI, 3–12%) [13] are common comorbidities in persons with chronic SCI, and are also recognised to increase the risk of COVID-19 infection [18]. In addition to that, due to noradrenergic over-activation and excess glucocorticoid release, persons with SCI may have systemic immunosuppression, which can further contribute to COVID-19 infection [19, 20].
Much has been documented in the literature regarding the clinical presentations and impact of the SARS-CoV-2 virus on the general population. However, the quantum of articles and research related to the persons with SCI during this pandemic at the time of this review is woefully low compared to the others. This article aims to segregate the relevant publications related to COVID-19 specific to the SCI and to provide a synopsis of the information regarding their presenting symptoms and clinical course published or known to date. It is hoped that this article will help physicians and health care workers to get an objective idea of what is being done or is needed for taking care of the persons with SCI during this pandemic.
Methods
Search strategy
We searched on PubMed, CENTRAL and MEDLINE with a strategy “Coronavirus”[MeSH] OR coronavirus[tiab] OR SARS-Cov-2[tiab] OR COVID-19[tiab] AND “Spinal cord Injury”[MeSH] OR “SCI”[MeSH] OR “Paraplegia”[MeSH] OR “Paraparesis”[MeSH] OR “Tetraplegia”[MeSH] OR “Tetraparesis” [MeSH] OR “Quadriplegia”[MeSH] OR “Quadriparesis”[MeSH] OR “spinal cord injury” [tiab] OR “SCI” [tiab] OR “paraplegia” [tiab] OR “tetraplegia” [tiab] OR “quadriplegia” [tiab], which revealed total of 2747 articles. The authors assessed the titles and abstracts of each article for screening and inclusion. Articles evaluating COVID-19 infections in persons with SCI were reviewed in full text. We also searched manually and reviewed relevant references in of identified articles.
Inclusion criteria and study selection
Studies were deemed eligible for inclusion if they (1) were observational studies or case series, or case reports; (2) were confirmed with reverse transcriptase-polymerase chain reaction (RT-PCR) on nasal exudate or sputum sample; (3) were on persons with SCI due to any aetiology; (4) reported clearly regarding either clinical features, complications and or outcomes. Correspondences or letters which were fulfilling the aforementioned criteria were included in this review.
The exclusion criteria were as follows: (1) duplicate studies; (2) abstract-only studies; (3) meta-analyses, review articles, consensus documents, comments, opinion articles and letters not presenting the original data; (4) publications with suspected COVID-19 cases but not confirmed with RT-PCR test; (5) articles written in languages other than English.
Study selection
Two reviewers (AB and SSR) independently searched the titles and abstracts of each article according to the inclusion and exclusion criteria. Full-text articles were obtained for evaluation. Any discrepancies during the selection were resolved by discussion and consensus.
Data extraction
Two reviewers (AB and SSR) extracted the data independently with a standardised data collection form, including (1) demographic information (age and gender), (2) basic information regarding SCI (aetiology, level of SCI, completeness of injury), (3) clinical symptoms, (4) abnormal blood test reports, (5) radiological findings, (6) therapies and (7) outcomes.
Data analysis
For continuous outcome, data were presented in mean (standard deviation (SD)). For dichotomous outcomes, the total number of events and total participants were extracted. If mean and SD were not reported in the particular study, it was calculated manually from the reported indicators. If data were not available or reported in an unusable way, the particular study was excluded from meta-analysis, and then data were presented descriptively.
Results
The outcome of the electronic search
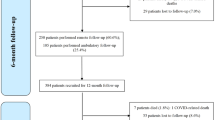
A total of 2747 articles were retrieved for the time frame January 2020 to January 2021. After excluding irrelevant (not matching the inclusion and exclusion criteria) and duplicate articles, 30 full-text articles were assessed (Fig. 1). Ultimately 11 articles [5, 21,22,23,24,25,26,27,28,29,30], out of which six were case reports [5, 26,27,28,29,30], were included in this review. Among the included articles, one was a cohort study (7 participants) [21], one case-control study (15 participants) [22], one case series (7 participants) [25] and two were retrospective data analyses (177 participants) [23, 24].
Characteristics of the included observational studies/case series
Epidemiological characteristics
A total of 206 persons with SCI with COVID-19 were reported from the five studies [21,22,23,24,25]. The mean age of the persons with SCI across these five studies [21,22,23,24,25] was 57.3(11.7) years. The level of injury was reported in 111 persons (four articles) [21,22,23, 25]. Burns et al. [23] did not mention the level of injury in 58 persons. However, he reported neurological classification in the remaining 82 cases. Among the 111 cases [21,22,23, 25], 40.54% persons with SCI (n = 45) sustained a cervical injury, 57.65% (n = 64) sustained thoracic injury (Table 1). Rodriguez-Cola et al. [21] in their study included four persons with SCI on tracheostomy tubes.
Median diagnostic time (the period from the onset of symptoms to confirmed COVID-19 infection with RT-PCR test) was reported only in one study [21]. The median diagnostic time was 4 days (interquartile range, 1–10 days). The other four studies [22,23,24,25] did not report mean diagnostic time.
Comorbidities were reported in three studies (n = 29) [21, 22, 25]. Pooling data from these three studies, it was found diabetes mellitus was present in 6(20.69%), dyslipidemia in 12(41.38%), HTN in 13(44.83%), chronic heart disease in 4(13.79%) and lung diseases were present in 6(20.69%) persons. Only one study [22] mentioned metabolic syndrome (n = 6, 40%).
Clinical characteristics
Out of five articles [21,22,23,24,25], three studies (n = 29) [21, 22, 25], reported the clinical symptoms of COVID-19 infection. Among them (n = 29), six (20.69%) persons remained asymptomatic throughout the disease. Pooled analysis from these three studies [21, 22, 25] showed that among the symptomatic persons (n = 23), fever (n = 19, 82.61%) was the most common presentation of COVID-19, followed by cough (n = 16, 69.56%), asthenia/fatigue (n = 7, 30.44%), dyspnoea (n = 9, 39.13%) (Table 2). Dhakal, in their study, cited fever as the most common presenting feature of COVID-19 infection in their SCI population (n = 37).
Chest imaging findings were reported in 29 persons (three articles) [21, 22, 25]. Among them (n = 29), 19 persons had abnormal chest imaging findings. Ground glass opacities (n = 10, 34.48%) were the most common radiological features, followed by uni- and/or multi-lobar pneumonia (n = 8, 27.59%). Of note, ten persons (34.48%) had no obvious radiological abnormalities (Table 2).
Two studies (n = 14) [21, 25] reported laboratory variables related to COVID-19 infection. Increased C-reactive protein (n = 14, 100%) was reported from all persons, followed by lymphocytopenia (n = 12, 85.71%), thrombocytopenia (n = 8, 57.14%) and increased ferritin (n = 7, 50%) showing increased inflammation and compromised immune function.
Treatments and outcomes
Two articles (n = 22) [22, 25] reported treatments of COVID-19 infection. Ventilator support in ICU was needed for three persons. Oxygen therapy was required in 13 persons (59.1%). Seventeen (77.27%) persons with SCI received low molecular weight (LMW) heparin at the time of hospital stays. There was only one case-control study [22], which compared the management strategies of COVID pneumonia between SCI and non-SCI populations. In their case-control study (n = 22), D’ Andrea et al. [22] did not find any difference in the management strategies of COVID-19 infection of persons with SCI (cases) from persons with able-bodied healthcare workers (control) with COVID pneumonia. In this study [22], participants recruited in both groups (SCI versus healthcare workers) were older (58 years versus 45 years). However, there were no significant differences in clinical features (p = 0.21) between these two groups [22].
Burns et al. [23] reported a case fatality rate of 19% (26 out of 140 persons) among veterans affected by SCI and COVID-19. In their study, Galea et al. [25] reported three deaths (42.86%) in SCI persons who were treated in veterans’ administration hospital. These three deceased persons were in critical condition, presented with multiple organ failure, including respiratory failure, septic shock, and renal disease. The average age of these three persons was 76.3(8.65) years, duration of injury was 13(7.55) years, body mass index was 30.0(4.45) kg/m3, the number of comorbidities was 7(1.00). These SCI persons were on mechanical ventilation and were admitted to COVID-19 ICU. However, Galea et al. [25] did not find any correlation of mortality with the level and completeness of SCI. Other than these two studies, the other three studies (n = 59) [21, 22, 24] did not report any death. In these three studies, all [21, 22, 24] persons with SCI, including 37 persons, reported from Nepal were treated successfully.
Case reports
There were a total of six articles (n = 6) [5, 26,27,28,29,30] that reported one individual in each case for a total of six case studies. The average age of the six persons was 54.3(17.19) years. Korupolu et al. [30] reported that the diagnosis of COVID-19 in their case was delayed by 2 weeks from the initial onset of fevers. Righi and Del Popolo [5] reported that their diagnosis was delayed by 8 days from the onset of fever. In both cases, both persons were initially treated for urinary tract infection (UTI). Five articles [5, 26,27,28, 30] mentioned COVID-19 symptoms in their cases. One article [29] did not mention COVID-19 symptoms. All five articles [5, 26,27,28, 30] reported that their cases (five persons, 100%) presented with fever (Table 3). In addition to fever, three articles [26,27,28] mentioned back pain and or muscle pain at initial presentation. Three persons [5, 27, 28] reported dyspnoea. One person [26] developed extensive bilateral deep vein thrombosis (DVT) even after chemoprophylaxis. One person [29] reported deterioration of neurological deficits after 6 weeks of COVID-19. Four persons [5, 26, 28, 30] developed ground glass opacities, and bilateral/unilateral pneumonic consolidation on chest radiograph. Three persons [5, 26, 28] reported abnormal laboratory variables, increased C-reactive protein, ferritin, ESR, D-dimer, lymphocytopenia, leucopenia and thrombocytopenia. Four articles [5, 26,27,28] discussed treatment during hospitalisation. Most reported cases were treated with oxygen therapy, antiviral therapy, hydroxychloroquine, LMW heparin, antibiotics and immunoglobulin. Prophylactic/therapeutic anticoagulation was administered in three reported cases [26,27,28]. Among six persons reported from six case reports, one person [27] expired. This person (28 years) had acute SCI (motorcycle accident), was diagnosed with having a C5-C6 burst fracture (C5 AIS A tetraplegia). Four days after surgical fixation of the cervical spine, he was diagnosed with having COVID-19 infection. On post-op day 10 (7 days after diagnosis of COVID-19 infection), this person was found unconscious. Cervical spine injury was indicated as a cause of death in legal documentation, and COVID-19 pneumonia was indicated as a comorbid condition [27]. Out of six case reports, one study [29] did not mention anything about the outcome of the person. Other reported cases [5, 26, 28,29,30] were treated successfully.
Discussion
We conducted a review of published research articles (till January 2021) on clinical presentations and the impact of the SARS-CoV-2 virus in SCI populations. For that, an extensive literature search was conducted in the various database using relevant keywords. Eleven articles, out of retrieved 2747 articles, fulfilled the inclusion criteria. Among them, six articles (n = 6) were case reports. Ultimately, 212 persons with SCI, who were diagnosed with COVID-19 infection, were included in this review. Most articles cited fever as the most common presenting feature of COVID-19 in persons with SCI. The other symptoms were cough, fatigue, dyspnoea, expectoration, diarrhoea and anosmia. In many persons with SCI, diagnosis of COVID-19 infection was delayed, as fever was attributed to the symptom of UTI instead of the initial symptom of COVID-19-infection. The most common abnormal laboratory parameters were raised C-reactive protein and lymphocytopenia. Ground glass opacities (on chest radiograph) were the most commonly seen radiological features of COVID pneumonia. Persons with SCI with COVID pneumonia were treated with oxygen therapy, antiviral therapy, hydroxychloroquine, LMW heparin and antibiotics. Prophylactic/therapeutic anticoagulation was advised in most of the admitted persons with SCI, along with other medications. With treatment, 91.2% (n = 182) persons with SCI with COVID-19 were successfully managed and discharged from the hospital setup. Injury at the spinal cord was not the criteria for admission and or transfer of the person in ICU set up. None of the authors suggested or recommended the admission at a higher setup or critical care unit based on the level and completeness of SCI (American Spinal Injury Association impairment score/ISCoS International Standards for Neurological Classification of Spinal Cord Injury [31].
Thermoregulatory dysfunction, lack of the typical febrile response and respiratory muscle weakness are usually encountered in persons with SCI lesions at thoracic level 8 or above. Due to diaphragmatic and thoracoabdominal muscle weakness, persons with SCI may present with impaired cough reflex, reduced lung volume, retention of oral secretions and autonomic dysfunctions [32, 33]. For these reasons, many authors expected that fever and cough, which are the main clinical features of COVID-19 in the normal population, would be impaired or might not be evident in the SCI population. However, in this review, we did not find very different presentations of COVID-19 from the normal population. Stillman et al. [34] conducted an international online survey (from March 23, 2020 to March 27, 2020) to investigate the health care professionals’ (SCI medical community) experience and or engagement in assessing, screening and treating persons with SCI with suspected and or confirmed COVID-19 cases. In this survey, a total of 783 SCI clinicians from six continents submitted their responses on the experience of COVID-19 infection among the SCI population. Out of 783 clinicians, only 4.4% reported that they had encountered persons with SCI with COVID-19 (till March 23, 2020). Other clinicians (till March 23, 2020) had not seen and or encountered an SCI person with COVID-19. According to this survey, commonly reported symptoms of COVID-19 in SCI were fever (86.2%), dyspnoea (62.1%), body aches, worsening pain (20.7%), sweats (20.7%) and chest pain (13.8%). Increased spasticity (10.3%) and rigour (6.9%) were also reported as atypical presentations of COVID-19. Similarly, Gustafson et al. [35] conducted another online international survey from May 21, 2020 to June 10, 2020, to assess the health care professionals’ experiences, knowledge and concerns of the COVID-19 pandemic SCI. Three hundred and sixty-six professionals (among them 63.1% were rehabilitation physicians) participated. Out of 366 professionals, only 12.1% responded that they had patients with SCI with COVID-19 infection. In this review [35], the most frequently cited presenting symptoms were fever (7.9%), shortness of breath (6.8%), sweats (1.6%), increased spasticity (1.6%), increased pain (1.4%), rash/peripheral lesions (1.4%) and anosmia (1.1%). In both surveys [34, 35]), the cough was not reported as a common presenting feature of COVID pneumonia in SCI. In their case-control study, D’ Andrea et al. [22] evaluated the differences in clinical features and evolution of COVID-19 between persons with SCI and normal health care workers. The study did not find any significant difference in presenting symptoms of COVID-19 infection among persons with SCI and health care workers. Also, in the laboratory (RT-PCR) and radiographic findings, D’ Andrea et al. [22] did not find any significant difference between these two groups.
In their study, Rodriguez-Cola et al. [21] observed that >50% of persons with SCI showed either only one or two symptoms at the time of COVID-19 confirmation and all these SCI persons followed benign outcomes [21]. None of the persons with SCI with COVID-19 from studies [21, 22, 24] needed ICU care during the hospital stay. However, based on these reported studies, it is very difficult to conclude that persons with SCI demonstrate less COVID-associated symptoms and follows a benign course. A major number of SCI people are unable to walk independently and depend on caretakers for their daily activities. Even for seeking medical treatment or visiting the hospital for their difficulties, persons with SCI are dependent on others. Therefore, there is a high possibility that persons with SCI, due to fear of isolation or separation from their family members, may underreport their COVID-associated symptoms. Due to this COVID-19 pandemic and or lockdown in their local areas, SCI persons are already living with fear, anxiety and or uncertainty about their future [36]. The Modified Early Warning System (MEWS) is a scoring system, which helps in assessing the deterioration risk in hospitalised patients based on abnormal changes in physiological parameters such as vital signs or mental status [37]. MEWS score of ≥3 indicates severe COVID-19 [22]. Rodriguez-Cola et al. [21], in their study, recorded MEWS scores in their SCI persons. According to the MEWS scoring, five persons (out of seven) were categorised under the “severe” category [21]. However, all persons (n = 7) in their study (Rodriguez-Cola et al.) [21] recovered gradually from the COVID infection.
Many authors [5, 28, 30, 36] reported that diagnosis of COVID-19 in their SCI persons was delayed as initial fever was attributed to either UTI or sepsis. It is evident from the literature that persons with SCI with COVID-19 infection may pose a unique diagnostic challenge in the current pandemic environment as many symptoms of COVID-19 infections may overlap with the complications of SCI. Common complications of SCI, like UTI, bacteremia, pneumonia, DVT and autonomic dysreflexia, can also cause a rise in body temperature and altered mental status. COVID-19 symptoms can sometimes overlap with the signs of respiratory failure due to SCI. Besides these, there is also a lack of knowledge about the challenge of identifying, monitoring and or recognising longer-term symptoms of COVID-19. All of these factors can complicate the accurate clinical diagnosis and management of persons with COVID-19. Burns et al. [23] reported mortality 2.4 times higher due to COVID-19 in the SCI population compared to the non-SCI population. However, in this study [23], only the veteran population with an average age of 67.0 years were included. In the literature, there are few reports of serious complications of COVID infection in SCI if it was not diagnosed and treated at an early stage. There is an increased risk of venous thromboembolic disorders following COVID infection, secondary to its associated hypercoagulable state. Pisano et al. [26] demonstrated a person with T11 (AIS-A) paraplegia who developed extensive bilateral lower limb DVT even after chemoprophylaxis. Pattanakuhar et al. [27] reported the sudden death of his case after initial improvement due to cardiac arrest.
This is the first review article related to COVID-19 and SCI. This study gives an idea of the current pattern of clinical presentation of COVID-19 in the SCI population, which can provide valuable information regarding accurate diagnosis and early management.
Limitation
This review has several limitations and confounding factors. This study included a large number of case studies. The search criteria were limited to English language articles only. There was a lack of a uniform database on morbidity and mortality statistics. This review included only those SCI persons who were tested and found positive for COVID-19. The number of spinal cord injured person in the included study was very less. A large number of asymptomatic persons or persons with minimal symptoms of COVID-19 with SCI were not included in this review. There was also a possibility that persons with SCI with symptoms of COVID-19 were misattributed to other medical conditions or complications of SCI during hospital treatment. Most of the published articles were reported from the developed countries and well-established hospital setup. Most of these SCI persons were probably rehabilitated previously and received the best care treatment for COVID-19 infection during the hospital stay. Therefore, the outcome of these SCI persons might not represent the outcome of the whole SCI population in general.
Conclusions
Based on the few studies published on COVID-19 and SCI populations since 2019, this study determined fever, elevated C-reactive protein, lymphocytopenia and ground glass opacities, which indicated inflammation, compromised immune response and lung edema, as the main clinical characteristics of COVID-19 infection among SCI population. Though COVID-19 infection reported an increased number of deaths in few studies, a major number of SCI populations with positive RT-PCR were treated successfully and discharged at home. However, there is a need for more focused research and information on the impact of the pandemic on persons with SCI.
References
Li B, Zhang S, Zhang R, Chen X, Wang Y, Zhu C. Epidemiological and clinical characteristics of COVID-19 in children: a systematic review and meta-analysis. Front Pediatr. 2020;8:591132.
World Health Organization 2020. Coronavirus disease (COVID-19)—World Health Organization. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 23 Dec 2020.
Wang C, Horby P, Hayden F, Gao G. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–3.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.
Righi G, Del Popolo G. COVID-19 tsunami: the first case of a spinal cord injury patient in Italy. Spinal Cord Ser Cases. 2020;6:22.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–9.
Cardozo CP. Respiratory complications of spinal cord injury. J Spinal Cord Med. 2007;30:307–8.
Bauman WA, Spungen AM, Raza M, Rothstein J, Zhang RL, Zhong YG, et al. Coronary artery disease: metabolic risk factors and latent disease in individuals with paraplegia. Mt Sinai J Med N Y. 1992;59:163–8.
Nash MS, Tractenberg RE, Mendez AJ, David M, Ljungberg IH, Tinsley EA, et al. Cardiometabolic syndrome in people with spinal cord injury/disease: guideline-derived and nonguideline risk components in a pooled sample. Arch Phys Med Rehabil. 2016;97:1696–705.
Duckworth WC, Solomon SS, Jallepalli P, Heckemeyer C, Finnern J, Powers A. Glucose intolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–10.
Bauman WA, Spungen AM. Metabolic changes in persons after spinal cord injury. Phys Med Rehabil Clin N Am. 2000;11:109–40.
García Leoni ME, Esclarín De Ruz A. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect. 2003;9:780–5.
Jones T, Ugalde V, Franks P, Zhou H, White RH. Venous thromboembolism after spinal cord injury: incidence, time course, and associated risk factors in 16,240 adults and children. Arch Phys Med Rehabil. 2005;86:2240–7.
Aidinoff E, Bluvshtein V, Bierman U, Gelernter I, Front L, Catz A. Coronary artery disease and hypertension in a non-selected spinal cord injury patient population. Spinal Cord. 2017;55:321–6.
Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:749–56.
Lee C-S, Lu Y-H, Lee S-T, Lin C-C, Ding H-J. Evaluating the prevalence of silent coronary artery disease in asymptomatic patients with spinal cord injury. Int Heart J. 2006;47:325–30.
Togan T, Azap OK, Durukan E, Arslan H. The prevalence, etiologic agents and risk factors for urinary tract infection among spinal cord injury patients. Jundishapur J Microbiol. 2014;7:e8905.
Henzel M, Shultz J, Dyson-Hudson T, Svircev J, DiMarco A, Gater D. Initial assessment and management of respiratory infections in persons with spinal cord injuries and disorders in the COVID‐19 era. JACEP Open. 2020;1:1404–12.
Riegger T, Conrad S, Liu K, Schluesener HJ, Adibzahdeh M, Schwab JM. Spinal cord injury-induced immune depression syndrome (SCI-IDS). Eur J Neurosci. 2007;25:1743–7.
Kasinathan N, Vanathi MB, Subrahmanyam VM, Rao JV. A review on response of immune system in spinal cord injury and therapeutic agents useful in treatment. Curr Pharm Biotechnol. 2015;16:26–34.
Rodríguez-Cola M, Jiménez-Velasco I, Gutiérrez-Henares F, López-Dolado E, Gambarrutta-Malfatti C, Vargas-Baquero E, et al. Clinical features of coronavirus disease 2019 (COVID-19) in a cohort of patients with disability due to spinal cord injury. Spinal Cord Ser Cases. 2020;6:39.
D'andrea S, Berardicurti O, Berardicurti A, Felzani G, Francavilla F, Francavilla S, et al. Clinical features and prognosis of COVID-19 in people with spinal cord injury: a case–control study. Spinal Cord Ser Cases. 2020;6:69.
Burns SP, Eberhart AC, Sippel JL, Wilson GM, Evans CT. Case-fatality with coronavirus disease 2019 (COVID-19) in United States Veterans with spinal cord injuries and disorders. Spinal Cord. 2020;58:1–2.
Dhakal R, O'connell C, Gurung JB, Shah RP, Adhikari HP, Chandi N, et al. A team effort in Nepal: experiences from managing a large COVID-19 rehabilitation hospital outbreak. Spinal Cord Ser Cases. 2021;7:5.
Galea MD, Gelman MA, Galea VP, Raulkar KP, Kornfeld S, Johnson-Kunjukutty S, et al. COVID-19 in spinal cord injury patients at a veterans administration hospital: a case series. J Spinal Cord Med. 2021:1–13. https://doi.org/10.1080/10790268.2020.1871254.
Pisano TJ, Joki J, Hon B, Cuccurullo S. Pulmonary embolism after acute spinal cord injury and COVID-19: a case report. Am J Phys Med Rehabil. 2020;99:982–5.
Pattanakuhar S, Tangvinit C, Kovindha A. A patient with acute cervical cord injury and COVID-19: a first case report. Am J Phys Med Rehabil. 2020;99:674–6.
Ayyildiz A, Kuran B, Altoparlak B, Dogu B, Yilmaz F. Complications of spinal cord injury can hide fever and cough associated to COVID-19. Asian J Case Rep Med Health. 2020;3:1–5.
Guadarrama-Ortiz P, Choreño-Parra JA, Pacheco-Sánchez FJ, Ponce-Sánchez JM, García-Quintero G, Rodríguez-Muñoz PE, et al. Chronic subclinical spondylotic myelopathy exacerbated by COVID-19: a case report. Interdiscip Neurosurg. 2021;23:100896.
Korupolu R, Stampas A, Gibbons C, Hernandez Jimenez I, Skelton F, Verduzco-Gutierrez M. COVID-19: screening and triage challenges in people with disability due to spinal cord injury. Spinal Cord Ser Cases. 2020;6:35 https://doi.org/10.1038/s41394-020-0284-7.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Berlly M, Shem K. Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med. 2007;30:309–18.
Galeiras Vázquez R, Rascado Sedes P, Mourelo Fariña M, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. BioMed Res Int. 2013;2013:168757.
Stillman MD, Capron M, Alexander M, Di Giusto ML, Scivoletto G. COVID-19 and spinal cord injury and disease: results of an international survey. Spinal Cord Ser Cases. 2020;6:21.
Gustafson K, Stillman M, Capron M, O'connell C, Longoni Di Giusto M, Tyagi N, et al. COVID-19 and spinal cord injury and disease: results of an international survey as the pandemic progresses. Spinal Cord Ser Cases. 2021;7:13.
North American Spinal Cord Injury Consortium 2020. COVID-19 & SCI Whitepaper—NASCIC: North American Spinal Cord Injury Consortium. 2020. https://nasciconsortium.org/covid-19-sci-whitepaper. Accessed 14 Apr 2021.
Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. QJM Mon J Assoc Physicians. 2001;94:521–6.
Author information
Authors and Affiliations
Contributions
AB was responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists and creating summary of findings tables. SSR was responsible for screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists and creating summary of findings tables. SKS was responsible for designing the writing the protocol and report, interpreting results, updating reference lists and creating summary of findings tables. JS was responsible for designing the review protocol, writing the protocol and report, interpreting results, updating reference lists and creating summary of findings tables.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barman, A., Roy, S.S., Sasidharan, S.K. et al. Clinical features and prognosis of COVID-19/SARS-CoV-2 infections in persons with spinal cord injury: a review of current literature. Spinal Cord Ser Cases 7, 58 (2021). https://doi.org/10.1038/s41394-021-00420-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00420-7