- Pancreas Center, The First Affiliated Hospital with Nanjing Medical University, Nanjing, China
Objective: To explore the level of care burden and its influencing factors of caregivers of pancreatic cancer patients during hospitalization under the background of COVID-19.
Methods: From September 2021 to December 2021, in Jiangsu Province Hospital, the convenience sampling method was used to investigate the care burden level of family caregivers of pancreatic cancer patients, and univariate and multivariate analysis methods were used to analyze the influencing factors. The survey tools included the General Information Questionnaire, the Family Caregiver Care Burden Scale, the Hospital Anxiety and Depression Scale, the Benefit Discovery Rating Scale, and the General Self-Efficacy Scale.
Results: A total of 100 subjects were included in this study, of which 45% were male and 55% were older than 50 years. In the Context of COVID-19, the care burden of caregivers of pancreatic cancer patients was at a mild level, and the main influencing factors were family economic status (p < 0.001), anxiety and depression level (p < 0.001) and self-efficacy (p < 0.001).
Conclusion: Medical staff should pay attention to the caregivers of pancreatic cancer with a heavy family burden, and pay attention to their anxiety and depression, and take corresponding measures to improve the self-efficacy of the caregivers, so as to reduce the care burden.
Introduction
Pancreatic cancer is one of the common malignant tumors of the digestive system. In 2018, the number of new cases of pancreatic cancer worldwide reached 458,918, and the number of deaths reached 432,242, with the number of deaths approximately equal to the number of cases (Bray et al., 2018). The incidence of pancreatic cancer in China is also increasing year by year, rising from the tenth to the seventh among all cancers (Sun, D. et al., 2020). Pancreatic cancer has a poor prognosis, with a 5-year survival rate of only 2–9%, ranking the lowest among all cancer types. Moreover, the quality of life of pancreatic cancer patients is significantly lower than that of other cancer types, which not only brings serious impact to patients, but also brings great impact to caregivers (Chu et al., 2017; Mcguigan et al., 2018).
In the process of caring for pancreatic cancer patients, caregivers generally have different degrees of care load, which will not only reduce the quality of life of caregivers themselves, but also affect the quality of care and thus reduce the quality of life of patients (Ansari et al., 2016). After the massive outbreak of COVID-19 at the end of 2019, major hospitals across the country implemented closed management and implemented “one person, one companion” to control the epidemic, and were not allowed to change caregivers at will. Studies have found that the panic caused by the epidemic, the heavy care task, the worry caused by the change of patients’ condition, and the psychological pressure caused by the hospital environment have doubled the burden of family caregivers (Bauer et al., 2018; Cohen et al., 2020). However, few studies have investigated the burden level of caregivers of pancreatic cancer patients and its influencing factors under the background of normalized COVID-19 prevention and control.
Therefore, this study aimed to investigate the current situation of the care burden of the main caregivers of pancreatic cancer patients during the COVID-19 outbreak in Nanjing in September 2021 and explore its influencing factors, so as to provide a theoretical basis for reducing the care burden of the main caregivers of pancreatic cancer patients under the closed management of the epidemic.
Materials and methods
Patient recruitment and exclusion criteria
From September 2021 to December 2021, 100 family caregivers of pancreatic cancer patients were selected by convenience sampling in Jiangsu Provincial People’s Hospital as the research objects. Inclusion criteria: ① Family caregivers of pancreatic cancer patients diagnosed by clinicopathological results; ② The family member who was designated by the pancreatic cancer patient to take care of them the most during the epidemic period; ③ Informed consent and willingness to participate in this study. Exclusion criteria: ① Family caregivers accompanied by serious physical or psychological diseases, such as cancer or obvious depression; ② The caregiver’s care time is less than 3 days.
General information questionnaire
The general information questionnaire was made by the researchers, including the patient’s name, age, gender, duration of illness, type of disease, caregiver’s age, gender, duration of care, educational background, family monthly income, number of children, relationship with the patient, work status, family economic pressure, etc.
Caregiving burden scale
The Caregiver Burden Scale of Cancer Patients (CBS-CP) contains 31 items, the last two of which evaluate the overall burden. In this study, the first 29 items were used for investigation, which were divided into 5 factor dimensions: physical burden (factor 1), economic burden (factor 2), psychological burden (factor 3), social burden (factor 4) and disease concept burden (factor 5). The SCALE is scored 0 points for “NEVER,” 1 point for “occasionally,” 2 points for “sometimes,” 3 points for “often” and 4 points for “always.” The total score of burden ≤29 is no burden; 29 < total score ≤ 58 is considered as mild burden; 59 < total score ≤ 87 is considered as moderate burden; A total score of >87 is considered as severe burden. Cronbach’s α coefficient of CBS-CP total scale and 5 factors fluctuated between 0.70 and 0.96, indicating good reliability.
Caregiver benefit discovery scale
The Caregiver Benefit Discovery Scale can be used to assess whether cancer patients and caregivers experience or benefit from positive aspects in coping with cancer challenges, including strengthened relationships with family members, personal growth as patients or caregivers, and healthier lifestyles inspired by cancer diagnosis and treatment (Li et al., 2017). The scale consists of 17 items on a 5-point scale, with 1 being “not at all” and 5 being “very much.” The higher the score, the more benefit the patient perceived on that item. Cronbach’s α coefficient of the overall benefit discovery scale and the three dimensions was ≥0.891, indicating good reliability.
Hospital anxiety and depression scale
Hospital Anxiety and Depression Scale is mainly used for rapid assessment of patients’ anxiety and depression, and is one of the tools for screening anxiety and depression in clinical practice. The scale has 14 items, including 7 items for anxiety and 7 items for depression. Each item was scored at 4 levels from 0 to 3, with each subscale scoring from 0 to 21. The total score of 8–10 was classified as mild anxiety/depression, 11–14 as moderate anxiety/depression, and ≥ 15 as severe anxiety/depression (Bjelland et al., 2002).
General self-efficacy scale
The General Self-efficacy Scale (GSES), compiled by German psychologist Ralf Schwarzwe (Schröder et al., 1997), consists of 10 items and is scored by the 4-point Likert Scale. “Completely incorrect” counts for 1 point, while “somewhat correct” counts for 2 points. “Mostly correct” counts for 3 points and “exactly correct” counts for 4 points. The higher the total score, the higher the self-efficacy of the subject. The Cronbach’s α coefficient of the scale was 0.87.
Data collection methods and quality control
Data were collected by two professionally trained nurses. The General Information Questionnaire, Care Burden Scale, Caregiver Benefit Discovery Scale, and General Self-efficacy Scale were distributed to caregivers who met the inclusion criteria and agreed to participate in the study. The investigators handed out questionnaires on site, and used unified instructions to explain the significance of the survey, the time required and the notes for filling in the survey to the caregivers. For caregivers who were illiterate or had visual impairment, the investigator stated the questions and options of the questionnaire, and the researcher checked them after answering the questions. General information and disease-related information can be obtained from medical records. If there is no record in medical records, consult the medical staff in charge of the bed or the caregivers themselves. Collect and check the questionnaire on the spot, and check with caregivers in time to ensure the completeness and accuracy of the questionnaire.
Statistical analysis
SPSS 22.0 software was used for data entry and statistical analysis. Measurement data were described by mean and standard deviation, and enumeration data were described by frequency and percentage. Independent sample t-test, ANOVA test, Pearson correlation analysis and multiple linear regression analysis were used to analyze the influencing factors of caregiver burden. In two-sided test, p < 0.05 was considered statistically significant.
Results
Figure 1 shows our workflow.
General information about caregivers
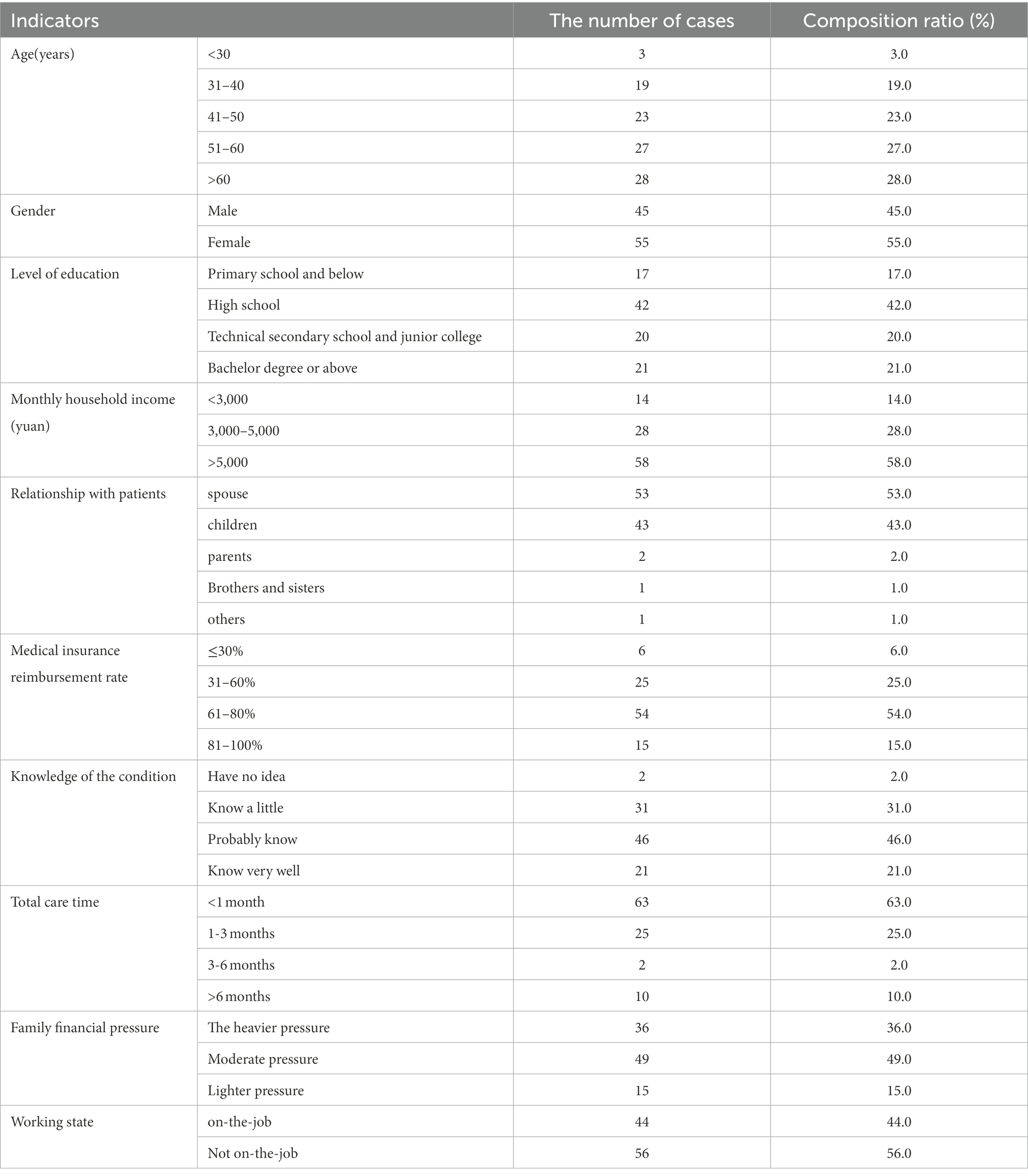
A total of 100 questionnaires were distributed and 100 were recovered, with a recovery rate of 100%. Among the 100 pancreatic cancer caregivers, 55% were older than 50 years and 45% were male. The rest of the general information is shown in Table 1.
Comparison of care burden scores of caregivers with different characteristics
The caring burden score of the main caregivers of pancreatic cancer patients was 44.04 ± 20.9, including 30 without burden, 43 with mild burden, 26 with moderate burden, and 1 with severe burden. There were statistically significant differences in the care burden of main caregivers with different ages, education levels, family monthly income, degree of understanding of illness, and family economic pressure (all p < 0.05; Table 2).

Table 2. Comparison of care burden scores of caregivers of pancreatic cancer patients with different characteristics (scores).
Benefit discovery, anxiety and general self-efficacy of caregivers of pancreatic cancer patients
The total score of anxiety and depression of caregivers of pancreatic cancer patients was 15.94 ± 9.64, the benefit finding was 80.8 ± 17.05, and the general self-efficacy was 25.14 ± 8.20. Pearson correlation analysis showed that benefit finding was inversely proportional to care burden (r = −0.558, p < 0.05), anxiety and depression were inversely proportional to care burden (r = 0.676, p < 0.05), and self-efficacy was inversely proportional to care burden (r = −0.280, p < 0.05), as shown in Table 3.

Table 3. Correlation analysis of care burden of caregivers of pancreatic cancer patients and its influencing factors (R value).
Multiple linear regression analysis of influencing factors of care burden of caregivers of patients with pancreatic cancer
In patients with pancreatic cancer burden of caregivers to take care of the total score as the dependent variable, the single factor analysis was statistically significant in the project as independent variables, multivariate linear regression analysis, finally found that anxiety depression (p < 0.001), and family economic pressure (p = 0.001) and self-efficacy (p = 0.014) are the influence factors of pancreatic cancer caregiver burden of care, The specific results are shown in Table 4.
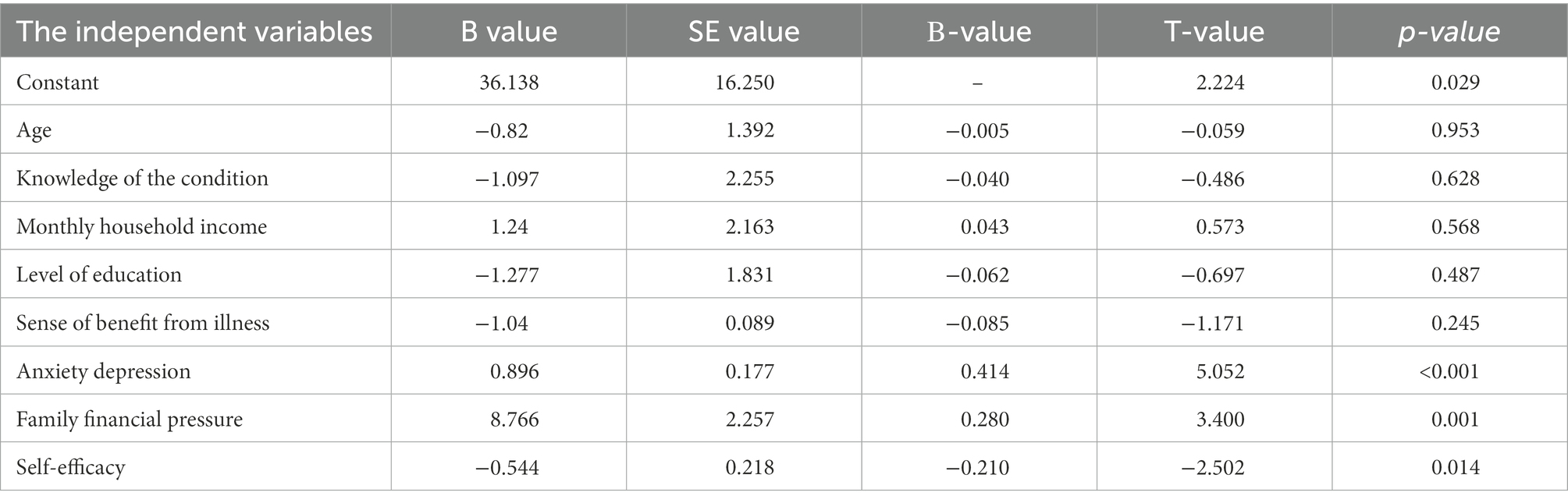
Table 4. Multiple linear regression analysis of influencing factors of care burden of caregivers of pancreatic cancer patients.
Discussion
The results of this study showed that the total score of care burden of caregivers of pancreatic cancer patients was (44.04 ± 20.9), which was generally at a mild level, among which 30% reported no burden, 43% reported mild burden, 26% reported moderate burden, and 1% reported severe burden. This finding is consistent with that of caregivers of breast and lung cancer patients in China, which cannot be compared with the burden of care in a non-pandemic setting due to the lack of research on caregivers of pancreatic cancer patients (Borges et al., 2017; Sun et al., 2019). Previous studies conducted qualitative interviews on caregivers of patients with inoperable pancreatic cancer, and the results showed that caregivers’ burden experience mainly included psychological burden, physical burden, lack of knowledge and emotional support, challenges in personal life, burden of disease notification and end-of-life decision-making (Xia et al., 2022). Pancreatic cancer has no characteristic symptoms in the early stage, and most patients are already in the late stage when they are diagnosed. The sudden disease will lead to the responsibility of caring for the family members in the case of insufficient preparation. At the same time, during the epidemic prevention and control period, the hospital’s closed management measures prohibit the random change of caregivers, resulting in all the care pressure concentrated in one person. This caregiver not only faces the stress of caring for the disease, but also faces the risk of the epidemic, which can easily lead to negative emotions and even physical health problems. It is necessary to pay attention to the physical and mental health of caregivers of pancreatic cancer (Sun et al., 2019).
Most of the pancreatic cancer patients in this study rated their family financial stress as moderate (49%) or heavy (36%), and the greater the family financial stress, the heavier the care burden of pancreatic cancer caregivers. Due to the continuous development and improvement of tumor treatment technology, while prolonging the survival time of patients, it also brings some economic burden to families, including high medical expenses, care costs and income reduction caused by the reduction of labor force. Some studies have shown that the family income of cancer patients after the disease is 32% lower than that before the disease, and the annual medical expenditure of cancer patients is 1.18 times of the average annual expenditure of the family (Xia et al., 2022). Pancreatic cancer mainly occurs in middle-aged and elderly people. The middle-aged people are the main labor force of the family, and their normal work is affected by the disease, which affects their family income (Khalaf et al., 2021). The elderly, due to physical reasons, have underlying diseases or are prone to complications, and so on, resulting in more follow-up treatment and care expenses (Huang et al., 2021). In addition, during the closed management of the epidemic, it greatly affected the normal work of caregivers and affected their economic income (Klein, 2021). Heavy economic burden will not only affect the treatment choice of patients, but also lead to patients’ quality of life decline, psychological distress and behavior change and many other adverse outcomes. Because the psychological burden perception of caregivers is closely related to the patient’s own condition, it will eventually lead to the increased perceived burden of caregivers. Therefore, in future studies, we should focus on patients and caregivers with heavy family burden, and actively carry out education, counseling and intervention programs for high-risk groups, so that caregivers can make full use of family and social resources and reduce the care burden caused by economic pressure.
In this study, the anxiety and depression score of caregivers was (15.94 ± 9.64), which was relatively severe. The anxiety and depression was directly proportional to the care burden. This is in line with the findings of a study on the quality of life of caregivers of pancreatic cancer patients, which showed that 14 to 32 percent of caregivers met the clinical cutoff for depression. Compared with patients with pancreatic cancer, caregivers had a significantly higher proportion of negative emotions such as anxiety and depression, which may be due to more stress on caregivers, such as bathing, feeding, wound/drainage care and monitoring complications. At the same time, the severe epidemic situation and the stress and pressure caused by the closed management of hospitals are more likely to lead to mental health problems of caregivers. Adverse emotional responses of caregivers can lead to a series of negative effects, such as the decline of their own health, poor quality of care, and emotional problems of patients (Bevans and Sternberg, 2012; Litzelman et al., 2016). In the actual process of clinical nursing, medical staff often ignore the psychological status of caregivers. In future research, it is necessary to evaluate the psychological status of patients and caregivers at the same time, and treat both sides as a whole. A cohort study showed that caregiver burden was primarily related to the baseline psychosocial health status of caregivers and patients (Jansen et al., 2021). Therefore, in future research, it is necessary to identify caregivers with poor psychological status early, so as to focus and target interventions.
Self-efficacy is an individual’s subjective judgment of his ability to perform a certain behavior, that is, his confidence in his ability to perform a certain behavior and achieve the expected results. For caregivers, it is a prerequisite to implement better care behaviors. Higher self-efficacy can help caregivers cope with care tasks with more confidence and less negative emotions, so as to cope with illness stress. This study found that the lower the self-efficacy of pancreatic cancer caregivers, the higher the care burden, which is consistent with previous studies. At present, a number of studies have been conducted to intervene the self-efficacy of cancer caregivers, and all of them have achieved good results. Hendrix conducted a randomized controlled trial of self-efficacy and care stress in caregivers of cancer patients, and the results showed that the intervention group had greater improvements in self-efficacy in cancer symptom management, stress management, and care preparation than the control group (Hendrix et al., 2016). A study on the influencing factors of the self-efficacy of caregivers of cervical cancer patients showed that caregivers with the number of shared help caregivers had higher self-efficacy than caregivers without the number of shared help caregivers. Due to the inability to change caregivers during the pandemic, one person must assume the care task, which may affect the self-efficacy of caregivers and ultimately increase their care burden. Therefore, in clinical nursing, it is necessary to pay attention to caregivers who have long periods of solitary care, screen and assess their perception of care burden as early as possible, and take corresponding intervention measures (Zou et al., 2021a,b).
So far, some studies have revealed the psychological impact of COVID-19 on care givers. Sun et al. found that in the early stage, negative emotions dominated, and self-treatment styles and psychological growth played an important role in maintaining the mental health of nurses (Sun, N. et al., 2020b). Panda et al. (2021) found that similarly, 52.3 and 27.4% of caregivers had anxiety and depression, respectively, during their isolation from their children (). Our study found that the caregiver burden of pancreatic cancer patients was at a mild level, and the main influencing factors included family economic pressure, caregiver anxiety and depression, and self-efficacy. These results can provide reference for psychological counseling of pancreatic cancer caregivers.
Conclusion
In conclusion, the care burden of caregivers of pancreatic cancer patients is at a mild level, and the main influencing factors include family economic pressure, anxiety and depression of caregivers and self-efficacy. In order to reduce the care burden of caregivers, but also to further improve the quality of care, medical staff should timely psychological counseling for caregivers with negative emotions, early attention should be paid to caregivers with poor family economic status and low self-efficacy, and carry out disease education for them. In future studies, we should expand the sample size and collect multi-center data to more comprehensively explore the influencing factors, so as to construct targeted intervention programs.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The First Affiliated Hospital of Nanjing Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
QS and XF designed the study and were responsible for the submission of the final version of the paper. QS, JJ, and JL were involved in database search and statistical analyses. QS and JC were involved in the writing of manuscript and its critical revision. All authors contributed to the article and approved the submitted version. All authors agree to be accountable for all aspects of the work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ansari, D., Tingstedt, B., Andersson, B., Holmquist, F., Sturesson, C., Williamsson, C., et al. (2016). Pancreatic cancer: yesterday, today and tomorrow. Future Oncol. 12, 1929–1946. doi: 10.2217/fon-2016-0010
Bauer, M. R., Bright, E. E., MacDonald, J. J., Cleary, E. H., Hines, O. J., and Stanton, A. L. (2018). Quality of life in patients with pancreatic cancer and their caregivers: a systematic review [J]. Pancreas 47, 368–375. doi: 10.1097/MPA.0000000000001025
Bevans, M., and Sternberg, E. M. (2012). Caregiving burden, stress, and health effects among family caregivers of adult cancer patients [J]. JAMA 307, 398–403. doi: 10.1001/jama.2012.29
Bjelland, I., Dahl, A. A., Haug, T. T., and Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale. An updated literature review [J]. J. Psychosom. Res. 52, 69–77. doi: 10.1016/S0022-3999(01)00296-3
Borges, E. L., Franceschini, J., Costa, L. H. D., Fernandes, A. L. G., Jamnik, S., and Santoro, I. L. (2017). Family caregiver burden: the burden of caring for lung cancer patients according to the cancer stage and patient quality of life [J]. J. Bras. Pneumol. 43, 18–23. doi: 10.1590/s1806-37562016000000177
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., and Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries [J]. CA Cancer J. Clin. 68, 394–424. doi: 10.3322/caac.21492
Chu, L. C., Goggins, M. G., and Fishman, E. K. (2017). Diagnosis and detection of pancreatic cancer. Cancer J. 23, 333–342. doi: 10.1097/PPO.0000000000000290.29189329
Cohen, G., Russo, M. J., Campos, J. A., and Allegri, R. F. (2020). Living with dementia: increased leve of caregiver stress in times of COVID-19 [J]. Int. Psychogeriatr. 32, 1377–1381. doi: 10.1017/S1041610220001593
Hendrix, C. C., Bailey, D. E. Jr., Steinhauser, K. E., Olsen, M. K., Stechuchak, K. M., Lowman, S. G., et al. (2016). Effects of enhanced caregiver training program on cancer caregiver's self-efficacy, preparedness, and psychological well-being [J]. Support Care Cancer 24, 327–336. doi: 10.1007/s00520-015-2797-3
Huang, J., Lok, V., Ngai, C. H., Zhang, L., Yuan, J., Lao, X. Q., et al. (2021). Worldwide burden of risk factors for, and trends in pancreatic cancer. Gastroenterology 160, 744–754. doi: 10.1053/j.gastro.2020.10.007
Jansen, L., Dauphin, S., de Burghgraeve, T., Schoenmakers, B., Buntinx, F., and van den Akker, M. (2021). Caregiver burden: an increasing problem related to an aging cancer population [J]. J. Health Psychol. 26, 1833–1849. doi: 10.1177/1359105319893019
Khalaf, N., El-Serag, H. B., Abrams, H. R., and Thrift, A. P. (2021). Burden of pancreatic cancer: from epidemiology to practice. Clin. Gastroenterol. Hepatol. 19, 876–884. doi: 10.1016/j.cgh.2020.02.054
Klein, AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat. Rev. Gastroenterol. Hepatol. (2021). 18:493–502. doi: 10.1038/s41575-021-00457-x
Li, Q., Lin, Y., Xu, Y., Zhou, H., Yang, L., and Xu, Y. (2017). Construct validity of the 17-item benefit finding scale in Chinese cancer patients and their family caregivers: a cross-sectional study [J]. Support Care Cancer 25, 2387–2397. doi: 10.1007/s00520-017-3644-5
Litzelman, K., Kent, E. E., Mollica, M., and Rowland, J. H. (2016). How does caregiver well-being relate to perceived quality of Care in Patients with Cancer? Exploring associations and pathways [J]. J. Clin. Oncol. 34, 3554–3561. doi: 10.1200/JCO.2016.67.3434
McGuigan, A., Kelly, P., Turkington, R. C., Jones, C., Coleman, H. G., and McCain, R. S. (2018). Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes [J]. World J. Gastroenterol. 24, 4846–4861. doi: 10.3748/wjg.v24.i43.4846
Panda, P. K., Gupta, J., Chowdhury, S. R., Kumar, R., Meena, A. K., Madaan, P., et al. (2021). Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J. Trop. Pediatr. 67. doi: 10.1093/tropej/fmaa122
Schröder, K. E., Schwarzer, R., and Endler, N. S. (1997). Predicting cardiac patients' quality of life from the characteristics of their spouses. J. Health Psychol. 2, 231–244. doi: 10.1177/135910539700200219
Sun, D., Cao, M., Li, H., He, S., and Chen, W. (2020a). National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100021, China Cancer burden and trends in China: a review and comparison with Japan and South Korea [J]. Chin. J. Cancer Res. 32, 129–139. doi: 10.21147/j.issn.1000-9604.2020.02.01
Sun, V., Raz, D. J., and Kim, J. Y. (2019). Caring for the informal cancer caregiver [J]. Curr. Opin. Support. Palliat. Care 13, 238–242. doi: 10.1097/SPC.0000000000000438
Sun, N., Wei, L., Shi, S., Jiao, D., Song, R., Ma, L., et al. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 48, 592–598. doi: 10.1016/j.ajic.2020.03.018
Xia, B. T., Otto, A. K., Allenson, K., Kocab, M., Fan, W., Mo, Q., et al. (2022). Patient-caregiver dyads in pancreatic cancer: identification of patient and caregiver factors associated with caregiver well-being. J. Behav. Med. 45, 935–946. doi: 10.1007/s10865-022-00354-x
Zou, Y., Hu, X., and Deng, X. (2021a). Distant lymph node metastases from breast cancer-is it time to review TNM cancer staging? JAMA Netw. Open 4:e212026. doi: 10.1001/jamanetworkopen.2021.2026
Zou, Y., Hu, X., Zheng, S., Yang, A., Li, X., Tang, H., et al. Discordance of immunotherapy response predictive biomarkers between primary lesions and paired metastases in tumours: a systematic review and meta-analysis. EBioMedicine. (2021b). 63:103137. doi: 10.1016/j.ebiom.2020.103137.; PMCID: PMC7736926
Keywords: pancreatic cancer, new crown epidemic, family caregivers, care burden, influencing factors
Citation: Sun Q, Li J, Fang X, Jin J and Cui L (2023) Current status and influencing factors of care burden of pancreatic cancer caregivers under COVID-19. Front. Psychol. 13:1066278. doi: 10.3389/fpsyg.2022.1066278
Edited by:
Zhaohui Su, Southeast University, Nanjing, ChinaReviewed by:
Chenyu Sun, AMITA Health Saint Joseph Hospital Chicago, United StatesJianing Lin, Karolinska Institutet (KI), Sweden
Peng Liu, Sun Yat-sen University, China
Copyright © 2023 Sun, Li, Fang, Jin and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoping Fang, fxp84284@163.com
 Qingmei Sun
Qingmei Sun Jiarong Li
Jiarong Li Xiaoping Fang*
Xiaoping Fang*