Decrease in Admissions and Change in the Diagnostic Landscape in a Newborn Care Unit in Northern Ghana During the COVID-19 Pandemic
- 1Department of Pediatrics and Child Health, School of Medicine and Health Sciences, University for Development Studies, Tamale, Ghana
- 2Department of Pediatrics and Child Health, Tamale Teaching Hospital, Tamale, Ghana
- 3Department of Public Health, Robbins College of Health and Human Services, Baylor University, Waco, TX, United States
- 4Duke Global Health Institute, Duke University, Durham, NC, United States
Background: The coronavirus disease (COVID-19) has spread worldwide with an increasing number of patients, including pregnant women and neonates. This study aims to evaluate morbidity and mortality in the COVID-19 era compared to the preceding year in the Neonatal Intensive Care Unit (NICU) at Tamale Teaching Hospital, Ghana.
Methods: This is a cross-sectional study carried out on neonates admitted to NICU between March 1st to August 31st, 2019 (pre-COVID-19 era) and March 1st to August 31st, 2020 (COVID-19 era). Multivariate logistic regression was performed to identify predictors of mortality for both periods.
Results: From 2,901 neonates, 1,616 (56%) were admitted before, and 1,285 (44%) were admitted during the pandemic. Admissions decreased during the COVID-19 era, reaching their lowest point between June and August 2020. Compared to the previous year, during the COVID-19 era, admissions of patients born at TTH, delivered at home, and with infections decreased from 50 to 39%, 7 to 4%, and 22 to 13%, respectively. Referred status (OR = 3.3) and vaginal delivery (OR = 1.6) were associated with an increased likelihood of mortality. For low- birth weight neonates, admissions of patients born at TTH, with vaginal and home delivery decreased from 62 to 48%, 8 to 2%, and 59 to 52%, respectively. Neonatal infections and congenital anomalies decreased from 8 to 4%, 5 to 3%, respectively. The likelihood of mortality among referred patients increased by 50%.
Conclusion: We observed a marked decrease in admissions and change in the diagnosis landscape and related mortality during the pandemic. Underlying challenges, including fear, financing, and health system capacity, might intensify delays and lack of access to newborn care in northern Ghana, leading to higher rates of lifelong disabilities and mortality. Immediate damage control measures, including an improved home-based continuum of care and equipping families to participate in the newborn care with complemented m-health approaches, are needed with urgency.
Introduction
Severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) is the strain of the virus with the typical symptoms at the onset of illness, including fever, difficulty in breathing, dry cough, and fatigue (1). The disease caused by this virus was named Coronavirus disease 19 (COVID-19) by the WHO on February 11th, 2020 (2). On January 30th, 2020, the World Health Organization (WHO) declared COVID-19 a Public Health Emergency of International Concern and, subsequently, a pandemic on March 11th, 2020 (3, 4). Transmission of the disease is through human-to-human respiratory droplets from a cough or sneeze and fomites (5). Being exposed to the epidemic center and close contact with infected family members were identified as risk factors for transmission (6). COVID-19 has and is still spreading rapidly across the globe with an increasing number of patients, including pregnant women and neonates (7).
With no vaccines or antiviral treatments widely available for COVID-19, the pandemic's negative impacts are most present in overburdened healthcare systems (8). Studies have shown that disruptions in routine care plans may lead to a backlog of surgical cases that may take years to clear (9–11). Some studies have also suggested more indirect deaths could result from these disruptions caused by COVID-19 (10). There was a documented increase in indirect causes of maternal and neonatal mortality during the Ebola outbreak in Sierra Leone (12). Therefore, the fear is that the gains made in child mortality may be negatively affected by COVID-19, especially in countries with fewer resources. On March 12th, 2020, Ghana confirmed its first two cases of COVID-19. Since then, Ghana has had a rapid increase in the number of confirmed cases of the disease. Also, there have been reports of the temporary closure of some maternity units and Neonatal Intensive Care Units (NICUs) as a result of positive COVID-19 cases, with the country losing a pediatrician to the virus (13–15).
In recent times, children and pregnant women have become highly at risk due to their unique and specially modulated immune status (16, 17). It was found that the virus has potentially unfavorable outcomes for both mother and fetus during the perinatal period (18). Although reports have suggested a lower prevalence in pediatric populations (19–21), Castagnoli et al. (5), in their systematic review of 18 studies, identified 1,065 pediatric cases of SARS-CoV-2 infection. Clinical manifestations of the disease in children might be less severe as compared with adult patients (6, 7, 21–25), however, younger children and infants are more susceptible to infections (24). For example, a three-month-old has been among the COVID-19 deaths reported in Ghana (26).
Although the in-patient care and daily outpatient clinics for newborns continued during the peak of the restrictions (i.e., closure of out-patients services and cancellation of non-emergency surgeries) at Tamale Teaching Hospital (TTH) NICU in Northern Ghana, we are not sure if care-seeking in the catchment area might have been affected by external factors. Therefore, this study aims to describe the impact of the COVID-19 pandemic on newborn care by comparing morbidity and mortality between the COVID-19 era and the preceding year in the Neonatal Intensive Care Unit (NICU) at Tamale Teaching Hospital, Ghana.
Methods
Setting and Participants
The TTH is a tertiary facility that serves a 4-million catchment population and is the main center for medical students' clinical training from the University for Development Studies School of Medicine and Health Sciences. This facility receives patients from Northern, North East, Savannah, Upper East, and Upper West regions, sometimes from Burkina Faso, Cote d'Ivoire, and Togo. The hospital is equipped with a 50 incubator/crib capacity NICU with a 7-bed Kangaroo Mother Care Unit attached to it. Besides medical care, the unit also provides pre-operative and post-operative care for sick neonates referred from the catchment areas (27). The study included all neonates admitted to the NICU from March 1st to August 31st, 2019 (pre-COVID-19 era), and March 1st to August 31st, 2020 (COVID-19 era). Neonates were recruited for the study if they were admitted from TTH maternity unit or theater, from other facilities in the catchment area, or from home, and they aged up to 28 days at presentation. Neonates with significantly missing data, whose records were not entered into the electronic database or who were referred to other facilities were not included in the study.
Study Design and Data Collection
This is a cross-sectional hospital-based study conducted at TTH NICU in northern Ghana to compare morbidity and mortality of neonatal admissions during the COVID-19 era to the period immediately preceding the pandemic. A local team of healthcare professionals at TTH (KAB and MJK) collected data from the TTH NICU between July and September 2020. AAM oversaw the data collection. The team used a predesigned data collection sheet to retrieve information on neonatal admissions, demographics, diagnosis, and outcomes from electronic records stored in the TTH NICU. For patients admitted two or more times, readmissions were not counted as new data entries. Instead, the first admission was included in this study. All information was deidentified and organized in an excel spreadsheet. COVID-19 incidence data (March-August 2020) were obtained from Our World in Data, a global database supported by the University of Oxford and Global Change Data Lab (28).
Data Analysis
The pre-COVID-19 era was defined as neonatal admissions from March 1st to August 31st, 2019. The COVID-19 era was defined as neonatal admissions from March 1st to August 31st, 2020. Birth weight was defined as normal birth weight (NBW ≥ 2,500 grams) and low birth weight (LBW < 2,500 grams) to facilitate subset analysis and interpretation of policy implications (29). Descriptive and inferential statistics were generated using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA). Demographic characteristics were compared among neonates admitted during the pre-COVID-19 era and the COVID-19 era using independent samples t-test and χ2 test when appropriate. Predictive variables included sex, region, referral, place of delivery, mode of delivery, birth weight, diagnosis, age of admission, length of stay, and insurance. The outcome was determined as a dichotomous variable (death/discharge). Bivariate and multivariate logistic regression analyses were performed to determine predictors of neonatal death. Only variables with p < 0.2 were included in the multivariate logistic regression model. Bivariate and multivariate logistic regressions were performed for neonates admitted during the pre-COVID-19 era and the COVID-19 era and in a subset population of neonates with birth weight <2500 g admitted during the pre-COVID-19 era and COVID-19 era. Statistical significance was defined at p < 0.05.
Ethics Statement
Permission and ethical clearance to conduct this retrospective chart review was granted by the Research and Development Department and the Ethical Review Committee of the TTH, respectively.
Results
A total of 2,901 neonates were admitted to TTH NICU between March 1st to August 31st in 2019 and 2020. Of these admissions, 1,616 (55.7%) were admitted before, and 1,285 (44.3%) were admitted after the declaration of the pandemic. General and low birthweight admissions decreased during the COVID-19 era and reached their lowest point between June and August 2020, while national COVID-19 incidence increased exponentially since March 2020 (Figure 1). During the COVID-19 era, admissions of inborn neonates decreased from 50% (n = 797/1,616) to 39% (n = 501/1,285) and neonates born at home decreased from 7% (n = 105/1,616 to 4% (n = 47/1,285). However, there was an increase in the proportion of referrals to the NICU from other facilities from 50% (n = 798/1,616) to 61% (n = 775/1,285) (Table 1). Furthermore, admissions due to neonatal infections decreased from 22% (n = 352/1,616) to 13% (n = 170/1,285). In contrast, admissions due to prematurity and complications, and neonatal jaundice increased from 25% (n = 398/1,616) to 28% (n = 355/1,285) and from 14% (n = 227/1,616) to 18% (n = 233/1,285), respectively. Age at discharge (11 vs. 9.7 days) decreased by one day, on average. The predictors associated with neonatal mortality pre-COVID-19 era were LBW (OR = 2.8), congenital anomalies (OR = 2.5), and birth asphyxia (OR = 1.9). In contrast, the predictors associated with neonatal mortality during the COVID-19 era were being referred from other facilities (OR = 3.3), LBW (OR = 2.8), birth asphyxia (OR = 2.0), and SVD (OR = 1.6) (Figure 2).
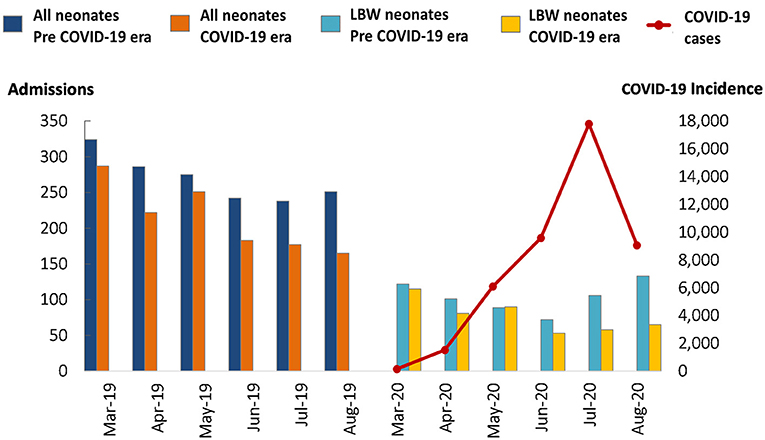
Figure 1. Frequency of neonates admitted in TTH NICU during pre-COVID-19 and COVID-19 era. Pre-COVID-19 was defined as neonatal admissions from March 1st to August 31st, 2019. COVID-19 era was defined as neonatal admissions from March 1st to August 31st, 2020.
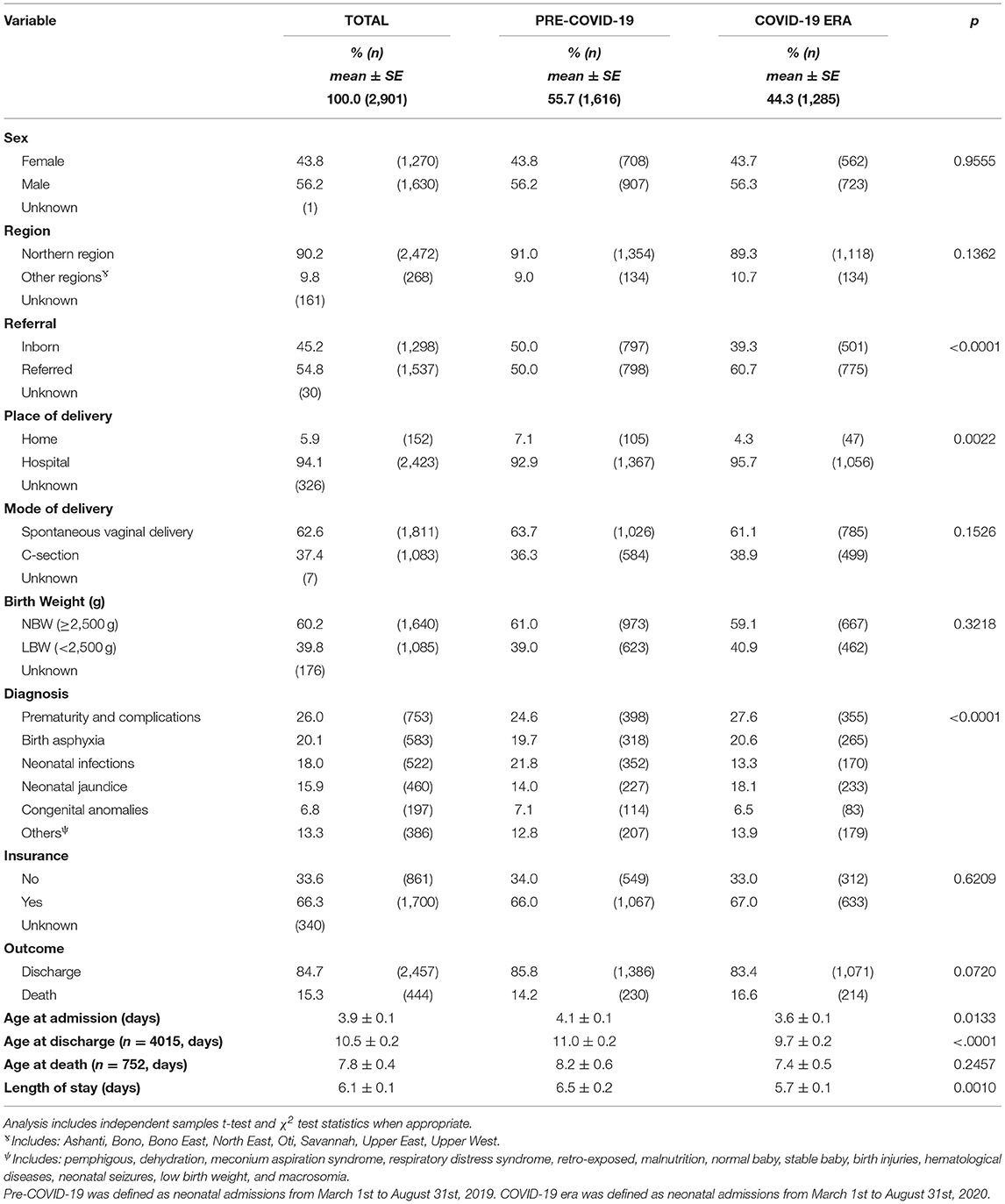
Table 1. General characteristics of neonates admitted in TTH NICU during pre-COVID-19 and COVID-19 era.
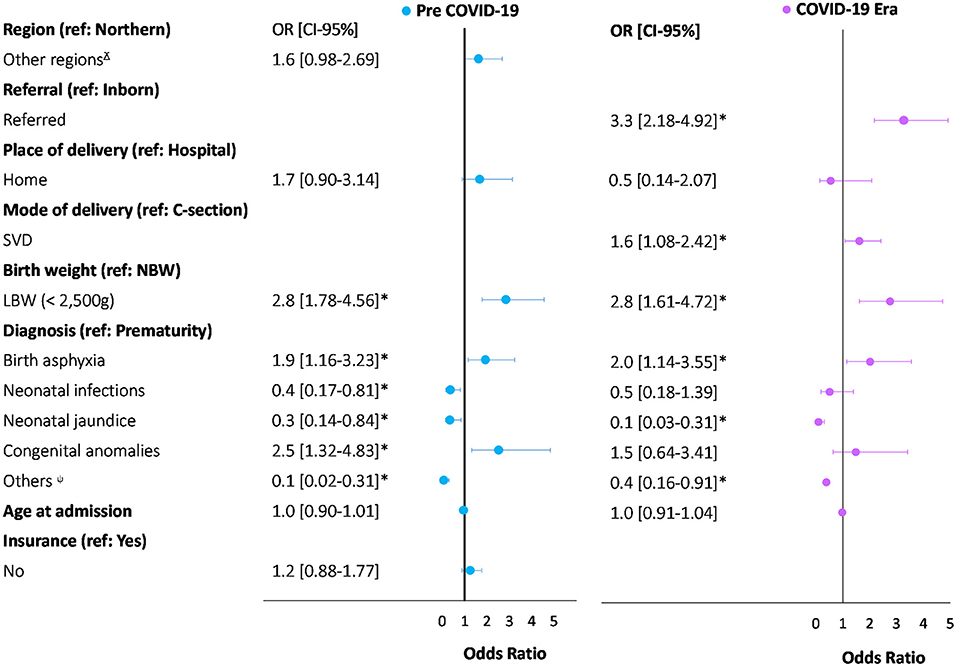
Figure 2. Comparison of multivariate logistic regression for predictors of neonatal death between pre-COVID-19 and COVID-19 era in TTH NICU. *Statistiscally significate (p < 0.05). ɤIncludes: Ashanti, Bono, Bono East, North East, Oti, Savannah, Upper East, Upper West. ψIncludes: pemphigous, dehydration, meconium aspiration syndrome, respiratory distress syndrome, retro-exposed, malnutrition, normal baby, stable baby, birth injuries, hematological diseases, neonatal seizures, low birth weight, and macrosomia. Pre-COVID-19 was defined as neonatal admissions from March 1st to August 31st, 2019. COVID-19 era was defined as neonatal admissions from March 1st to August 31st, 2020.
When stratified by low birth weight (<2,500 grams), admissions of inborn neonates decreased from 62% (n = 386/623) to 48% (n = 220/462), neonates born at home decreased from 8% (n = 48/623) to 2% (n = 10/462), and neonates born by SVD decreased from 59% (n = 368/623) to 52% (n = 241/462). However, there was an increase in the proportion of referrals to the NICU from other facilities from 38% (n = 235/623) to 52% (n = 240/462), and neonates born by caesarian section increased from 41% (n = 254/623) to 48% (n = 221/462) (Table 2). Furthermore, admissions due to neonatal infections and congenital anomalies decreased from 8% (n = 53/623) to 4% (n = 17/462) and from 5% (n = 31/623) to 3% (n = 15/462), respectively. In contrast, admissions due to prematurity and complications, and neonatal jaundice increased from 60% (n = 377/623) to 66% (n = 307/462) and from 6% (n = 39/623) to 9% (n = 40/462), respectively. Age at discharge (12.7 vs. 10 days) and length of stay (9.4 vs. 7 days) decreased by two days, on average. The predictors associated with neonatal mortality pre-COVID-19 era were congenital anomalies (OR = 2.9) and being referred from other facilities (OR = 1.8). In contrast, the predictors associated with neonatal mortality during the COVID-19 era were birth asphyxia (OR = 2.7) and being referred from other facilities (OR = 2.3). The likelihood of mortality during the COVID-19 era compared to the pre-COVID-19 era increased by 50% among referred neonates (2.3 OR vs. 1.8 OR) (Figure 3).
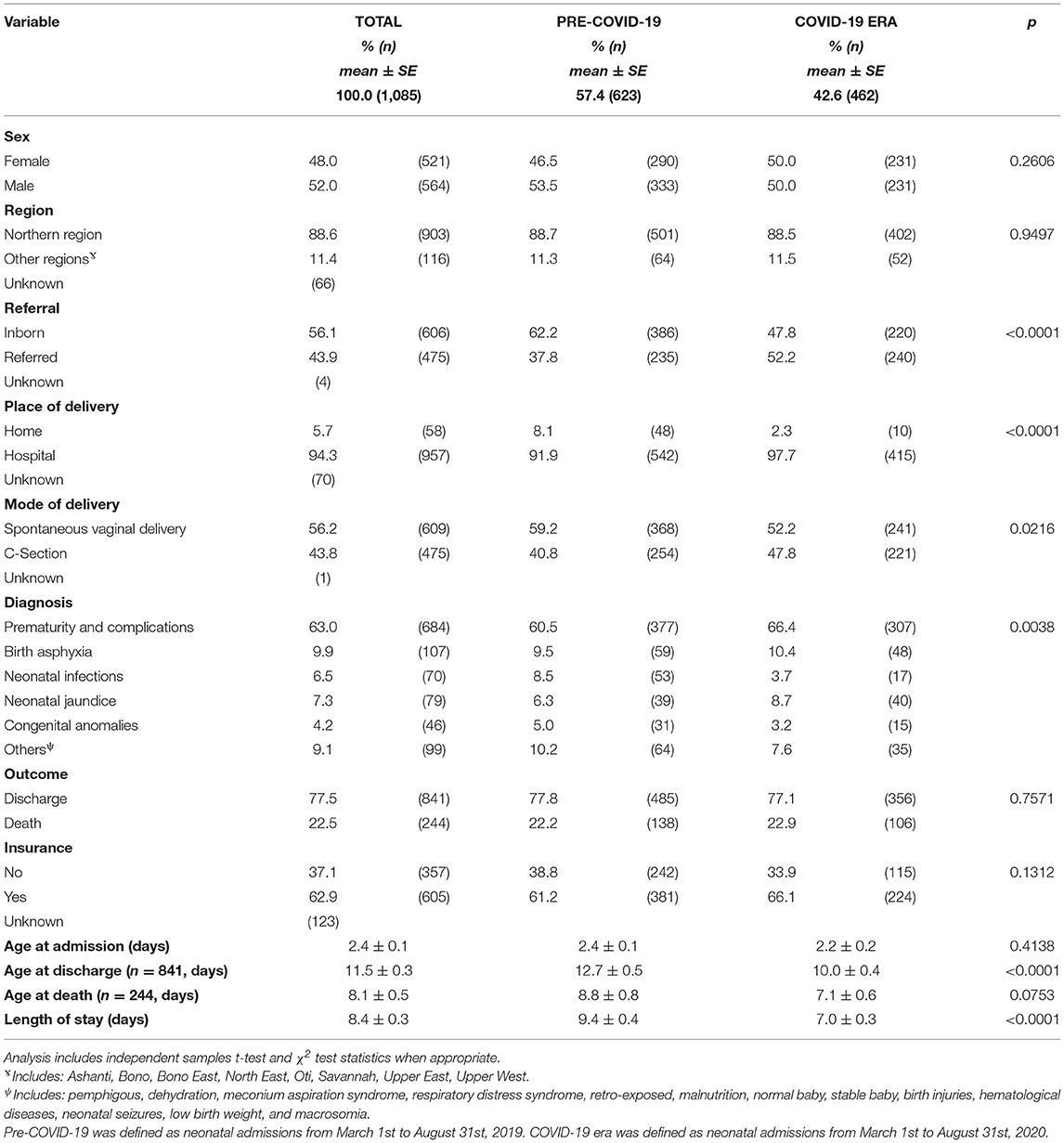
Table 2. General characteristics of LBW neonates (< 2500 g) admitted at TTH NICU during pre-COVID-19 and COVID-19 era.
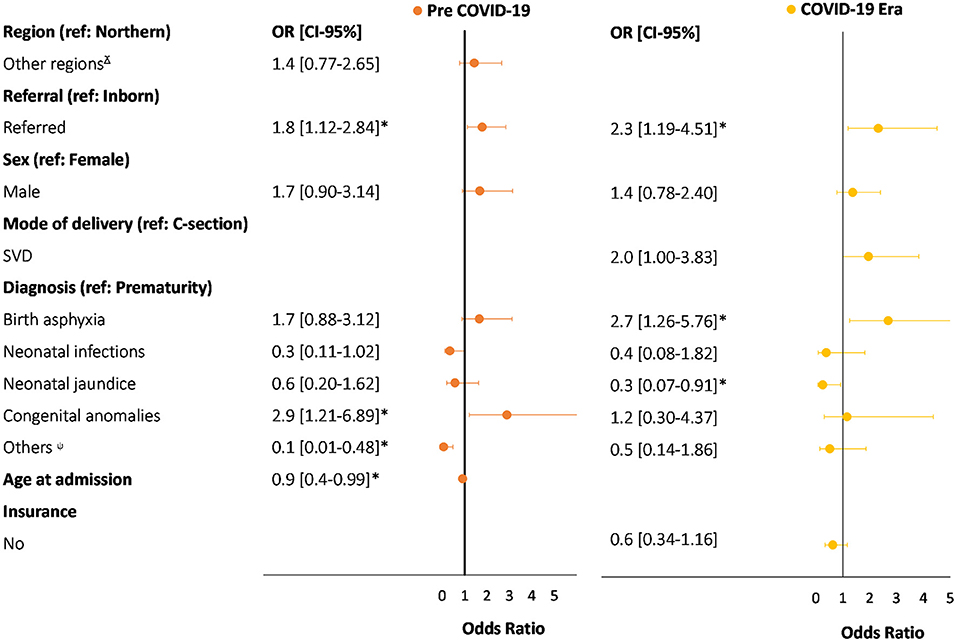
Figure 3. Comparison of multivariate logistic regression for predictors of neonatal death between pre-COVID-19 and COVID-19 era in LBW neonates (<2,500 g) in TTH NICU. *Statistiscally significate (p < 0.05). ɤIncludes: Ashanti, Bono, Bono East, North East, Oti, Savannah, Upper East, Upper West. ψIncludes: pemphigous, dehydration, meconium aspiration syndrome, respiratory distress syndrome, retro-exposed, malnutrition, normal baby, stable baby, birth injuries, hematological diseases, neonatal seizures, low birth weight, and macrosomia. Pre-COVID-19 was defined as neonatal admissions from March 1st to August 31st, 2019. COVID-19 era was defined as neonatal admissions from March 1st to August 31st, 2020.
Discussion
In this cross-sectional hospital-based study, we sought to document the early impact of COVID-19 on neonatal admissions and deaths by comparing data in our unit between the COVID-19 era and the pre-COVID-19 era. Overall, we found a significant decrease in neonatal admissions and changes in the landscape of diagnosis and their associations with mortality during the pandemic. These changes and additional challenges, including limited healthcare capacity, financial constraints, and widespread fear, might severely undermine newborn care in northern Ghana.
The Northern region is one of the poorest regions in Ghana (30). With the advent of the COVID-19 pandemic, the disparities in access to newborn care in this region have intensified. Our data suggest a decrease in admission from neonates born at home during the COVID-19 era. As part of the pandemic response and “the stay at home unless necessary” slogan, patients and their families were advised to refrain from visiting health facilities unless essential (31). In northern Ghana, where healthcare-seeking behaviors are already sub-optimal, the implementation of strict protocols of decongestion at TTH might have contributed to the step back from the most vulnerable communities' progress. Previous studies have found about 40% of women in northern Ghana deliver at home (32). For women who prefer to give birth at home due to traditional beliefs, lack of trust in the healthcare system, and financial challenges (33–35), additional challenges such as lockdown measures and fear of infection may have a significant influence when deciding to seek care at a health facility (36, 37). Previous literature has reported an 8% decrease in deliveries at health facilities during other health crises (38). If that is true for COVID-19 in northern Ghana, then the proportion of newborns without access to health care increases, thereby escalating the number of preventable neonatal deaths.
Decreased healthcare utilization is potentially explained by the fear of the virus and the lack of financial resources. Previous studies on knowledge, attitudes, and practices toward the pandemic in low-resource settings have shown disparities in understanding and performing the best preventative measures (39). This, in turn, can affect caregivers' decision-making when seeking medical and surgical care for their children amid a global pandemic. A previous study reported a decline in visits to pediatric emergency departments due to fear of contracting the coronavirus infection in Italy (40). Healthcare utilization is often negatively impacted by limited financial and medical resources. On average, for neonatal treatment of perinatal asphyxia and low birthweight in Ghana, out-of-pocket costs for care account for 66% of costs, and families often spend 9% of their annual income on acute care (41). Moreover, we have already seen increased closures of maternity units and NICUs within Ghana (13, 14). These shifts in resources and personnel often negatively impact emergency and essential surgical care, such as Cesarean sections (42). Such reductions in maternal and child health provisions have been estimated to result in 28,000 additional maternal deaths and 168,000 additional newborn deaths in LMICs (43).
We documented an increase in referrals and related likelihood of neonatal mortality during the COVID-19 era, compared to the pre-pandemic era. The increase in referrals could be explained by the fact that most lower health facilities were not operating at full capacity, and some facilities suspended operations temporarily due to exposure of staff to the coronavirus infection. In addition, antenatal clinics were not functioning at full capacity, with a resultant decrease in pregnancy monitoring. This might explain the increased likelihood of mortality among referred babies, as our facility received most of the complicated pregnancies and critically ill neonates from the catchment area. In the Ebola epidemic in Sierra Leone, a decline in utilization of vital reproductive, maternal and neonatal health services was reported, with about 22% decrease in antenatal care coverage and a consequent increase in neonatal deaths (38). Furthermore, SVD delivery was associated with an increase in neonatal mortality. This could be explained by the late presentation of pregnant women to the hospital due to initial hesitancy, leading to complicated deliveries (37).
Another collateral effect of the COVID-19 pandemic in TTH NICU is the drastic change of the diagnostic landscape and associated likelihood of mortality. We observed an increase in prematurity and complications, and neonatal jaundice admissions but a decrease in admissions from neonatal infections and congenital anomalies. The increase in jaundice cases could be explained by the early discharge of mother-infant pairs from the hospital, and the fewer opportunities for follow-up at postnatal clinics as most of these clinics suspended services during the peak of the pandemic. This potentially increased the risk for severe neonatal jaundice, a significant contributor of neonatal mortality and long-term disability related to neurocognitive issues, cerebral palsy, deafness, and learning difficulties (44–46).
Neonatal infections, birth asphyxia, and congenital anomalies remain among the leading causes of morbidity and mortality among neonates in LMICs (47–50). However, our results show the profile of neonatal admissions in the COVID-19 era look different from the pre-COVID-19 era, with fewer admissions related to neonatal infections and congenital anomalies, increased likelihood of mortality due to birth asphyxia (especially for LBW neonates), and decreased likelihood of mortality due to congenital anomalies. In normal times, admissions to our NICU due to birth asphyxia and other peripartum adverse events occur on the day of birth and from the delivery rooms, while admissions due to infections and other conditions occur later in the first week and from home. The decrease in admissions of neonatal infections during the pandemic could be explained by the increase in non-presentation—as these patients usually present from home—and/or the increased measures in hand hygiene and use of personal protective equipment during the peak of the pandemic in Ghana. On the other hand, the likelihood of mortality due to birth asphyxia could have been intensified by the decrease in admissions related to other diagnoses.
Congenital anomalies disproportionately affect children in LMICs and, if left untreated, can result in lifelong disabilities and death (51, 52). Before the pandemic, patients with congenital anomalies usually presented to TTH from home. Our data suggest that admissions and likelihood of mortality for these patients decreased during the COVID-19 pandemic. As previously discussed, the decrease in admissions is most likely explained by the widespread fear among caregivers and the preexisting, if not intensified, financial barriers in low resource settings. In consequence, congenital anomalies were not seen as a leading predictor of death during the COVID-19 pandemic, as it was pre-pandemic. The surgical backlog generated by underreported congenital anomalies contributes to the hidden neonatal mortality and the underestimation of the burden of disease in northern Ghana.
Recommendations
Communities should be empowered with accurate information regarding the prevention and treatment of SARS-CoV-2 to increase healthcare utilization for the most vulnerable populations, such as pregnant women and sick newborns (42). Immediate damage control measures, including an improved home-based continuum of care and equipping families to participate in the newborn care with complemented m-health approaches are needed to mitigate the impact of the COVID-19 pandemic in newborn care in northern Ghana (31). As we battle with the second wave of the pandemic, effective care for neonatal jaundice should include risk factor screening, the early establishment of breastfeeding, monitoring and managing hyperbilirubinemia, and parental education before neonate discharge (53). To continue to prepare hospitals for the direct and indirect impacts of the pandemic, resources for surgical care should be improved, health care personnel should be educated on available treatments for SARS-CoV-2, and hospitals should ensure the provision of personal protective equipment (42, 54).
Limitations
Our study constitutes a foundational step in identifying neonatal care challenges in northern Ghana amidst the COVID-19 crisis. However, some limitations warrant discussion. First, our study shares the limitations of cross-sectional designs, such as the inability to make causal inferences and establish temporal relationships between exposures and outcome. However, we offer a baseline knowledge that might be useful for future studies with more robust designs. Second, this a hospital-based study, and its results are limited to be generalized to the whole population. Therefore, a collection of robust population-based data is needed to evaluate newborn care access in northern Ghana. Third, data on COVID-19 incidence was not found for the Northern region, specifically. Instead, we used incidence data at a national level. Third, this study does not include specific data that can accurately explain the changes found in the neonatal care at TTH during the COVID era. Further studies may focus on hospital capacity, healthcare personnel, and parental perspectives to obtain a comprehensive view of the barriers hindering neonatal care amid the pandemic. Future studies may also focus on implementing and evaluating interventions to decrease the adverse effects of COVID-19 in newborn care and guide the creation of a robust evidence-based emergency preparedness protocol for neonatal care in Ghana.
Conclusion
We have documented a decline in neonatal admissions and change in the diagnosis landscape and related mortality during the height of the COVID-19 restrictions in Ghana. As we battle with the second wave of the COVID-19 pandemic, common underlying factors such as widespread fear, financial challenges, and limitations in health system capacity might intensify direct and indirect impacts and contribute to more acute delays and lack of access to newborn care in northern Ghana. Consequently, higher rates of lifelong disabilities and preventable neonatal deaths due to leading causes of neonatal mortality and surgical backlog might be experienced in this country. Immediate damage control measures, including an improved home-based continuum of care and equipping families to participate in newborn care with complemented m-health approaches, are needed to mitigate the effects of the COVID-19 pandemic in newborn care in northern Ghana.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Committee of the Tamale Teaching Hospital. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
AA-M conceived the study, sought relevant permissions for the study, supervised the data collection, provided guidance for the data analysis, and contributed to the initial drafts and revision of the manuscript. ES oversaw the project, provided guidance for the data analysis, and contributed to the study design and revision of the manuscript. KB and MK collected and cleaned the initial data and contributed to the initial draft and revision of the manuscript. CC-C analyzed the data, contributed to the study design, drafting, and revision of the manuscript. AG contributed to the initial drafting and revision of the manuscript. RY, PK, and YF supervised the data clean-up, contributed to the drafting and revision of the manuscript. All authors read and approved the final draft of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to acknowledge all staff of the Neonatal Intensive Care Unit (NICU), Mr. Akram Baba Yakubu, and the Head of Research and Development Department, Mr. Alhassan Mohammed Shamudeen, of the Tamale Teaching Hospital.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.642508/full#supplementary-material
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
2. WHO Director-General's Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed September 20, 2020).
3. Eurosurveillance editorial team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Eurosurveillance. (2020) 25:131. doi: 10.2807/1560-7917.ES.2020.25.5.200131e
4. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed September 20, 2020).
5. Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. (2020) 174:882–9. doi: 10.1001/jamapediatrics.2020.1467
6. Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. (2020) 20:689–96. doi: 10.1016/S1473-3099(20)30198-5
7. Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. (2020) 174:722–5. doi: 10.1001/jamapediatrics.2020.0878
8. Q&A on coronaviruses (COVID-19). Available online at: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed July 1, 2020).
9. Collaborative C. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. (2020) 107:1440–9. doi: 10.1002/bjs.11746
10. Salenger R, Etchill EW, Ad N, Matthew T, Alejo D, Whitman G, et al. The surge after the surge: cardiac surgery post–COVID-19. Ann Thor Surg. 110:2020–5. (2020). doi: 10.1016/j.athoracsur.2020.04.018
11. Surgery Backlog Crisis Looming. CMAJ. Available online at: https://www.cmaj.ca/content/192/21/E593 (accessed September 20, 2020).
12. Counting Indirect Crisis-Related Deaths in the Context of a Low-Resilience Health System: the Case of Maternal and Neonatal Health During the Ebola Epidemic in Sierra Leone. Health Policy and Planning. Oxford Academic. Available online at: https://academic.oup.com/heapol/article/32/suppl_3/iii32/4621472 (accessed September 20, 2020).
13. Korle-Bu: Child Health Dept. Closed Down After Child Died of Coronavirus. (2020) Available online at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Korle-Bu-Child-Health-Dept-closed-down-after-child-died-of-coronavirus-938782 (accessed September 20, 2020).
14. Maternity Unit at Bolgatanga Hospital to Shut Down Following Coronavirus Case - MyJoyOnline.com. Available online at: https://www.myjoyonline.com/news/regional/the-newborn-care-unit-at-the-bolgatanga-hospital-will-be-closed-from-monday-until-further-notice-authorities-say/ (accessed September 20, 2020).
15. Kwadaso SDA Hospital Medical Director Dies of Coronavirus. (2020) Available online at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Kwadaso-SDA-Hospital-Medical-Director-dies-of-coronavirus-980140 (accessed September 20, 2020).
16. Adar T, Grisaru-Granovsky S, Ben Ya'acov A, Goldin E, Bar-Gil Shitrit A. Pregnancy and the immune system: general overview and the gastroenterological perspective. Dig Dis Sci. (2015) 60:2581–9. doi: 10.1007/s10620-015-3683-z
17. Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. (2010) 63:425–33. doi: 10.1111/j.1600-0897.2010.00836.x
18. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. (2020) 9:51–60. doi: 10.21037/tp.2020.02.06
19. Han D, Li R, Han Y, Zhang R, Li J. COVID-19: Insight into the asymptomatic SARS-COV-2 infection and transmission. Int J Biol Sci. (2020) 16:2803–11. doi: 10.7150/ijbs.48991
20. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
21. Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. SARS-CoV-2 Infection in children. N Engl J Med. (2020) 382:1663–5. doi: 10.1056/NEJMc2005073
22. Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. (2020) 26:502–5. doi: 10.1038/s41591-020-0817-4
23. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
24. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. (2020) 145:e20200702. doi: 10.1542/peds.2020-0702
25. Cruz AT, Zeichner SL. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics. (2020) 145:e20200834. doi: 10.1542/peds.2020-0834
26. Three-Month-Old Baby Among COVID-19 Deaths in Northern Region. Available online at: https://citinewsroom.com/2020/06/three-month-old-baby-among-covid-19-deaths-in-northern-region/ (accessed September 20, 2020).
27. Abdul-Mumin A, Owusu S, Wright N, Decker J, Niemeier K, Benavidez G, et al. Burden of neonatal surgical conditions in Northern Ghana. World J Surg. (2019) 2019:1–9. doi: 10.1007/s00268-019-05210-9
28. Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Coronavirus pandemic (COVID-19). Our World in Data. (2020) Available online at: https://ourworldindata.org/coronavirus/country/ghana (accessed September 20, 2020).
29. ICD-10: International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organization (2011).
30. Kobina Annim S, Mariwah S, Sebu J. Spatial inequality and household poverty in Ghana. Econ Syst. (2012) 36:487–505. doi: 10.1016/j.ecosys.2012.05.002
31. Abdul-Mumin A, Agbozo F, Abubakari A, Jahn A. Maintaining quality newborn care in Ghana amid the COVID-19 pandemic. Pan Afr Med J. (2020) 35:6. doi: 10.11604/pamj.2020.35.4.22797
32. Ghana Statistical Service, Ghana Health Service ICF. Ghana Maternal Health Survey 2017: Key Findings. Available online at: https://www.dhsprogram.com/pubs/pdf/SR251/SR251.pdf (accessed October 7, 2020).
33. Boah M, Adampah T, Jin B, Wan S, Mahama AB, Hyzam D, et al. “I couldn't buy the items so I didn't go to deliver at the health facility” Home delivery among rural women in northern Ghana: a mixed-method analysis. PLoS ONE. (2020) 15:e0230341. doi: 10.1371/journal.pone.0230341
34. Adatara P, Strumpher J, Ricks E, Mwini-Nyaledzigbor PP. Cultural beliefs and practices of women influencing home births in rural Northern Ghana. Int J Womens Health. (2019) 11:353–61. doi: 10.2147/IJWH.S190402
35. Moyer CA, Adongo PB, Aborigo RA, Hodgson A, Engmann CM. “They treat you like you are not a human being”: maltreatment during labour and delivery in rural northern Ghana. Midwifery. (2014) 30:262–8. doi: 10.1016/j.midw.2013.05.006
36. UNICEF. Maternal and Newborn Health and COVID-19. Available online at: https://data.unicef.org/topic/maternal-health/covid-19/ (accessed October 7, 2020).
37. Moyer CA, Sakyi KS, Sacks E, Compton SD, Lori JR, Williams JEO. COVID-19 is increasing Ghanaian pregnant women's anxiety and reducing healthcare seeking. Int J Gyn Obs. (2020) 152:444–5. doi: 10.1002/ijgo.13487
38. Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plann. (2017) 32:2–9. doi: 10.1093/heapol/czx108
39. Lau LL, Hung N, Go DJ, Ferma J, Choi M, Dodd W, et al. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: A cross-sectional study. J Glob Health. 10:7. doi: 10.7189/jogh.10.011007
40. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. (2020) 4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5
41. Enweronu-Laryea CC, Andoh HD, Frimpong-Barfi A, Asenso-Boadi FM. Parental costs for in-patient neonatal services for perinatal asphyxia and low birth weight in Ghana. PLoS ONE. (2018) 13:e0204410. doi: 10.1371/journal.pone.0204410
42. Ma X, Vervoort D, Reddy CL, Park KB, Makasa E. Emergency and essential surgical healthcare services during COVID-19 in low- and middle-income countries: A perspective. Int J Surg. (2020) 79:43–46. doi: 10.1016/j.ijsu.2020.05.037
43. Riley, Sully, Ahmed, Biddlecom. Estimates of the potential Impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries. Int Persp Sex Reprod Health. (2020) 46:73. doi: 10.1363/46e9020
44. Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediat Res. (2013) 74:86–100. doi: 10.1038/pr.2013.208
45. Shapiro SM. Bilirubin toxicity in the developing nervous system. Pediat Neurol. (2003) 29:410–21. doi: 10.1016/j.pediatrneurol.2003.09.011
46. Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. (2012) 379:445–52. doi: 10.1016/S0140-6736(11)61577-8
47. Thaver D, Zaidi AKM. Burden of neonatal infections in developing countries: a review of evidence from community-based studies. Pediat Infect Dis J. (2009) 28:S3-9. doi: 10.1097/INF.0b013e3181958755
48. Lawn JE, Cousens S, Zupan J. Neonatal survival 1: 4 million neonatal deaths: when? Where? Why? The Lancet (British edition). (2005) 365:891–900. doi: 10.1016/S0140-6736(05)71048-5
49. Ersdal HL, Mduma E, Svensen E, Perlman J. Birth asphyxia: a major cause of early neonatal mortality in a Tanzanian rural hospital. Pediatrics. (2012) 129:e1238. doi: 10.1542/peds.2011-3134
50. Alliance for Maternal and Newborn Health Improvement (AMANHI) mortality study group. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health. (2018) 6:e1297–e1308. doi: 10.1016/S2214-109X(18)30385-1
51. Sitkin NA, Ozgediz D, Donkor P, Farmer DL. Congenital anomalies in low- and middle-income countries: the unborn child of global surgery. World J Surg. (2015) 39:36–40. doi: 10.1007/s00268-014-2714-9
52. Toobaie A, Yousef Y, Balvardi S, St-Louis E, Baird R, Guadagno E, et al. Incidence and prevalence of congenital anomalies in low- and middle-income countries: a systematic review. J Pedia Surg. (2019) 54:1089–93. doi: 10.1016/j.jpedsurg.2019.01.034
53. Ma X-L, Chen Z, Zhu J-J, Shen X-X, Wu M-Y, Shi L-P, et al. Management strategies of neonatal jaundice during the coronavirus disease 2019 outbreak. World J Pediatr. (2020) 347:1–4. doi: 10.1007/s12519-020-00347-3
54. Van Nguyen H, Van Hoang M, Dao ATM, Nguyen HL, Van Nguyen T, Nguyen PT, et al. An adaptive model of health system organization and responses helped Vietnam to successfully halt the Covid-19 pandemic: What lessons can be learned from a resource-constrained country. Int J Health Plan Manag. (2020) 35:988–92. doi: 10.1002/hpm.3004
Keywords: COVID-19, neonatal mortality, pandemic impact, northern Ghana, newborn care
Citation: Abdul-Mumin A, Cotache-Condor C, Bimpong KA, Grimm A, Kpiniong MJ, Yakubu RC, Kwarteng PG, Fuseini YH and Smith ER (2021) Decrease in Admissions and Change in the Diagnostic Landscape in a Newborn Care Unit in Northern Ghana During the COVID-19 Pandemic. Front. Pediatr. 9:642508. doi: 10.3389/fped.2021.642508
Received: 16 December 2020; Accepted: 26 February 2021;
Published: 25 March 2021.
Edited by:
Michelle Starr, Indiana University, United StatesReviewed by:
Cheryl Moyer, University of Michigan, United StatesJesper Padkær Petersen, Aarhus University Hospital, Denmark
Copyright © 2021 Abdul-Mumin, Cotache-Condor, Bimpong, Grimm, Kpiniong, Yakubu, Kwarteng, Fuseini and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emily R. Smith, emily_r_smith@baylor.edu
 Alhassan Abdul-Mumin
Alhassan Abdul-Mumin Cesia Cotache-Condor3
Cesia Cotache-Condor3  Kingsley Appiah Bimpong
Kingsley Appiah Bimpong Mary Joan Kpiniong
Mary Joan Kpiniong Rafiuk Cosmos Yakubu
Rafiuk Cosmos Yakubu Peter Gyamfi Kwarteng
Peter Gyamfi Kwarteng Emily R. Smith
Emily R. Smith