Abstract
Background
During the COVID-19 pandemic, prioritization of care and utilization of scarce resources are daily considerations in healthcare systems that have never experienced these issues before. Elective surgical cases have been largely postponed, and surgery departments are struggling to correctly and equitably determine which cases need to proceed. A resource to objectively prioritize and track time sensitive cases would be useful as an adjunct to clinical decision-making.
Methods
A multidisciplinary working group at Emory Healthcare developed and implemented an adjudication tool for the prioritization of time sensitive surgeries. The variables identified by the team to form the construct focused on the patient’s survivability according to actuarial data, potential impact on function with delay in care, and high-level biology of disease. Implementation of the prioritization was accomplished with a database design to streamline needed communication between surgeons and surgical adjudicators. All patients who underwent time sensitive surgery between 4/10/20 and 6/15/20 across 5 campuses were included.
Results
The primary outcomes of interest were calculated patient prioritization score and number of days until operation. 1767 cases were adjudicated during the specified time period. The distribution of prioritization scores was normal, such that real-time adjustment of the empiric algorithm was not required. On retrospective review, as the patient prioritization score increased, the number of days to the operating room decreased. This confirmed the functionality of the tool and provided a framework for organization across multiple campuses.
Conclusions
We developed an in-house adjudication tool to aid in the prioritization of a large cohort of canceled and time sensitive surgeries. The tool is relatively simple in its design, reproducible, and data driven which allows for an objective adjunct to clinical decision-making. The database design was instrumental in communication optimization during this chaotic period for patients and surgeons.
Similar content being viewed by others
The COVID-19 pandemic brought novel challenges and forced difficult decision-making. As the number of cases continued to increase, prioritization of care and utilization of scarce resources became daily considerations in healthcare systems. While the primary impact of the viral spread occurred in the emergency rooms and intensive care units (ICU), procedural specialties stopped providing medical care to preserve resources and protect patient safety. Several societies published guidelines aimed towards maximizing health benefits to patients, decision-making at an institutional level, and maintenance of ethical principles [1,2,3]. For proceduralists, the conversation largely centered around mitigating risk of exposing patients or healthcare workers to the virus, tracking and trending available resources, and ongoing procedural case prioritization for the patients thus far untreated [4, 5].
As a result of this pandemic, elective surgical procedures were postponed, and the number of time sensitive cases performed daily was curtailed sharply. Consequently, there was a large burden of untreated surgical disease. Surgery departments struggled to correctly and equitably determine which cases were highest priority to proceed. Additionally, there was great need for communication across many different groups within the healthcare system. This led to large volume meeting, email, and phone communication burden. The usefulness of prior systems such as scheduling offices and scheduling software programs was reduced due because they lacked the ability to discriminate surgical priority. Without these processes, there was even more communication burden on select individuals involved in creating a surgical schedule, leading to the potential for missed information or failed communication.
In short notice, development of in-house prioritization strategies for surgical backlogs and large volume communication burden became paramount.
Materials and methods
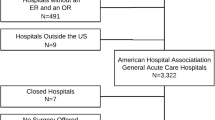
Emory Healthcare comprises 8 hospitals and one ambulatory surgery center. The hospitals are broadly variant in setting from large quaternary referral centers represented by all subspecialties to smaller community hospitals with core specialties.
On March 16th, 2020, Emory Healthcare suspended all elective surgical procedures for a rolling two week period with weekly reassessment. In this early phase of the pandemic, we established definitions for surgical priority which became the basis of our current vocabulary.
-
Emergent – immediate operation
-
Urgent—operation needed within the week
-
Time Sensitive – operation needs to be done in next 1–12 weeks
-
Elective- operation can be delayed > 12 weeks without detriment
On March 22, 2020- Emory Healthcare expanded suspension of surgical care to include Time Sensitive procedures, as internal pandemic dashboards indicated the possibility of a surge in COVID-19 cases in the coming days. This was accompanied by heightened concerns about availability of PPE, as well as the first signs of members of our own healthcare team becoming unable to work.
It became clear that there was an expanding backlog of pending surgical cases across multiple specialty surgical services which would need adjudication to proceed to limited operating rooms. At each site, entrusted surgical leaders were appointed to Adjudicator teams, consisting of members from proceduralist, anesthesia, and nursing leadership. These teams were led by the “Adjudicator”, acting as a local liaison at each site and charged with putting forward the highest priority cases for surgery, taking into account the stability of critical resources. An immediate challenge was determining relative case priority across surgical subspecialties. During this time period, management of myriad case requests occurred through variable means including electronic mail, text messaging, and phone call communications. In addition to being a highly manual process involving individually managed spreadsheets, the volume of these requests led to difficulty in prioritization, organization, and creation of a daily surgical schedule.
On April 4th, Departmental leadership recognized the burgeoning need for the site Adjudicators to have an objective construct to prioritize cases which ensured access to all specialties. A small team (“Team 9”) was tasked with creating what we now call the “Adjudicator Tool”.
Goals/Guiding principles
-
Provide a tool to prioritize and track pending time sensitive surgeries locally
-
Simple
-
Objective (to the extent possible)
-
Consistent prioritization across sites
-
Access for both cancer and benign cases
-
-
Adjudicators apply clinical expertise and judgment overseeing prioritization
-
o
Local (Site specific) resources may cause some cases on the priority list to be temporarily skipped or directed to an alternative site:
-
ICU
-
PPE
-
Blood products
-
Dialysis
-
Bed availability
-
-
o
Recognizing the myriad of variables pertinent to various surgical diseases, Team 9 discussed a high-level approach to prioritization. The variables identified by the team to form the construct focused on the patient’s survivability, potential impact of delayed care on function, and high-level disease biology.
-
Patient Age
-
Cancer (type)
-
Will survival be affected?
-
Will function be irreversibly affected by delaying surgery
-
Will delay make surgery more complex (e.g., complications occur) or increase the needed resources (ICU, blood products, etc.)
Each of these data were variably weighted to develop a prioritization system.
Prioritization score element definitions
Four weighted items are used to calculate the total score, and were calculated as follows.
Survival
The primary variable affected by delay of cancer care. This variable was input by the requesting physician, choosing from 6 possible choices: null, 1 week, 2 weeks, 4 weeks, 8 weeks, or 12 weeks. The answer correlates to the number of weeks that could pass before a change in the patient's survival from ongoing delay of surgical care would be expected. This formed an Adjusted Survival Score based on an empirically derived weighting system (Fig. 1A):
Example: A patient with pancreatic cancer might be expected to have a change in life expectancy without surgical treatment in two weeks, whereas a patient with papillary thyroid cancer might expect that 12 weeks could pass before a change in life expectancy might be incurred.
Function
Irreversible loss of function was deemed the primary variable affected by delay of surgery for patients with benign conditions. Factors that could result in loss of function may include items such as escalating neurologic deficits, irreversible loss of key body functions including ambulation, organ function, need for transfusions, or potential future deficits if further delay is incurred. This variable was input by the requesting physician, who chooses from 6 possible delay choices: null, 1 week, 2 weeks, 4 weeks, 8 weeks, or 12 weeks. This answer formed an Adjusted Function score based on the same empirical weighting system as used for the Adjusted Survival Score (Fig. 1B).
Example: A patient with gallstones having daily symptoms of biliary colic might have a functional impact in 1 week without surgical treatment, where as a patient with a mildly symptomatic paraesophageal hernia and anemia, requiring iron infusions, might have an expected change in function in 8 or 12 weeks without surgical treatment.
Increased complexity if delayed
Case complexity was deemed to be potentially affected by delay of surgical care. This answer is provided by a requesting surgeon with only two possible answers: yes or no. A case’s complexity would increase if there was a high chance that, if delayed, the operation needed could change (a hernia becomes incarcerated), or different treatments would be required (ICU admission, need for blood transfusions). This variable addresses the potential for a Time Sensitive case to become urgent and potentially consume more. For this variable, the adjusted score was either 100 or 0 points.
Life expectancy
This variable was obtained using readily available published data from the Social Security Life Expectancy Tables, and then calculating the expected remaining years of life [6]. For benign conditions, the remaining years of life expected may not change with delay in surgical care, but for cancer patients, delay in care or biology of the tumor could potentially have great impact. The anticipated survival from the most common cancer types was obtained from the website for the National Cancer Institute [7]. This 10-year survival data do not account for specific patient tumor characteristics but does allow for some finer definition of survival of the most common cancer types. More specified calculations were deemed beyond the scope and desired user simplicity of this time sensitive project.
Final prioritization score calculation
The final prioritization score was used by adding the adjusted scores from the 4 primary inputs into a total score. Based on social security tables, we estimated the Years of Life Remaining (YLR) based on current age. Based on 10-year survival rates for cancer, we then multiplied the YLR by that survival percentage (or by 100% if no cancer) and divided that number by 0.8 to get the Years Remaining Score (YRS). The Survival Impact Score (SIS) was calculated based on the number of weeks a cancer case can be delayed without affecting survival (1 wk = 100, 2 wks = 80, 4 wks = 60, 8 wks = 40, 12 wks = 20). In a non-cancer case, the Quality of Life Impact Score (QOLIS) is calculated based on the number of weeks a non-cancer case can be delayed before permanent negative effects on bodily function or ability to return to pre-morbid activity level will be impacted (1 wk = 100, 2 wks = 80, 4 wks = 60, 8 wks = 40, 12 wks = 20). The Added Complexity Score (ACS) is a binary option: If delay of the case will result in the need for added resources (e.g., ICU, blood) or the need for a much bigger operation that could be avoided if the case were not delayed then the ACS = 100 (yes) or ACS = 0 (no). To get the final prioritization score, each of the four components are multiplied by the relative weighting factor and added [Prioritization Score = (YRS X 0.25) + (SIS × 0.40 OR QOLIS × 0.25) + (ACS × 0.10)].
Note again that a patient was assigned in the Tool with either an Adjusted Survival Score, or an Adjusted Function score, but not both. This was intended to give access to procedural resources for both cancer and non-cancer cases. For any patient, proceduralists were only asked to input EITHER Survival or function data, and no patient received scores for both. The greater of the two would be judged by the provider. The relative weighting of the key components of the Final Score are shown in Fig. 1B. These weightings were empirical, and there was intent to modify these formulas if required to improve prioritization and discrimination of the values. Team 9 beta-tested the Tool with many hypothetical scenarios to ascertain if the prioritization performance would be as expected.
Additional variables were deemed necessary to determine the availability of potentially scarce resources but did not affect the prioritization score included:
-
Surgical specialty
-
Patient Identifiers
-
Procedure requested
-
Reason Case is Time Sensitive
-
Anesthesia Requirements
-
Estimated Case Length
-
Blood requirements
-
Expected length of stay (LOS)
-
ICU stay (yes/no)
-
Preferred Surgical day of week
All of these variables were included either to assist with scheduling, decreasing communication needs, or for screening purposes in the event of an acute resource scarcity (e.g., an ICU bed is not available, so screen out cases that might require this resource). These items are important but were not viewed as playing a role in the prioritization of the case, and thus were not part of the prioritization score, but rather used a filters in the database that could be toggled by the Adjudicator (see Figure 3B, boxes in yellow, for filter options in the document).
Review process for time sensitive cases
It was agreed that assurance of the validity of the input data would be necessary to protect the integrity of an objective system. The team concluded that all requests for Time Sensitive cases should be vetted and approved by their appropriate Division Chief or Department Chair. This would allow the data to be validated by content experts, rather than placing this task on the local Adjudicator, who is unlikely to be a content expert in multiple specialties. This would also allow for cases from a single specialty to likely come with built-in prioritization from that section, if the inputs for those cases were vetted accurately. An email template was created for the submission of Time Sensitive surgery requests in the same order as the data needed to be input into the tool, and this was widely disseminated through various forums to the proceduralists to ensure compliance with use. This template would be filled out by the requesting surgeon and submitted to the Chief who could vet and approve the request and validate the accuracy of the content.
Creation of the adjudicator tool
The initial version of the tool was a spreadsheet calculator with the aforementioned four inputs. The resulting prioritization could be seen by the Adjudicator and not by the requestor, but the process remained very manual with reentry of data from requests into the calculator, and then transcription of the score back into the individual spreadsheets of surgical requests being maintained at each of the system’s sites.
A database solution was built to address several ongoing concerns, principally repetitive data entry at each process step, and Adjudicator communication burden (Fig. 2). Due to time constraints and the necessity for ease of access, the interface solution was built in Excel and linked to an Access database via Visual Basic for Applications (VBA) and Structured Query Language (SQL). The database was built within the healthcare system’s networks, in which all users have space on a shared drive. Permissions to the database could then be granted to users by existing credentials, and the activity on the database and in the interface documents would occur within the secure virtual network of the healthcare system, fulfilling the need for security. Distribution of multiple interface documents allowed for multiple users to access the database at the same time and prevent interruption of service while maintaining security through the use of the built-in worksheet protections. Updating these documents to add new data fields or functionality was not as streamlined—it was necessary to maintain a consistent and open line of communication, which allowed for quicker adoption of newer versions while allowing individuals with data issues to quickly receive user support and improve staff buy-in. Thus far, there have been 3 distributed versions of the documents. Each new version added features to improve functionality for all users, including those entering in data and those making adjudication decisions (features like sorting, filters, visual appeal).
Use of the chief of service documents
The section Chief or Chair has access to two different interface documents (Fig. 2). The first is the “Input” document which allows the requisite data points from the proceduralists’ request template to be entered. Use of this interface ensures completeness of data entry, and once complete, the data are stored in the database and are removed from the Input document. Included in this submission is which hospital location being requested by the proceduralist. The second document is an “Output” document which shows all of the active requests for that Division/Department, not ranked by priority. The requestors of cases are blinded to the prioritization score, which is only kept in the database. Using these two documents, the Division Chief or Department Chair can easily enter requests, see their own section’s pending requests, and remove/replace requests if they are canceled or the information changes.
Use of the adjudicator document
The Adjudicator works from a single document which has capabilities to both input cases if needed, as well as data review of the prioritized case list (Fig. 3). Requested cases are visible to the adjudicator in prioritization order, but the Adjudicator is also blinded to the raw score. Adjudicators are also able to modify all entered data cell by cell to keep it updated if required. Given that these weighting formulas were empirically derived, and this was rapidly developed, the Adjudicator is charged with exercising clinical judgment as well as verification of resource availability in selecting the final list of cases to be performed on a given day. Varying conditions with PPE, blood products, or ICU teams might affect the choice of cases to be scheduled and cause the need to skip some cases that had higher priority, and these can be filtered, or sorted, depending on the variable. There is also an opportunity to recommend resubmission of the case to other system sites if those sites might be more appropriate (e.g., moving an outpatient case to the ambulatory surgery center). Other factors such as patient comorbidities, patient location, or equitable service allocation of operating room access might be used to drive creation of the schedule.
Screenshot of the Adjudicator Tool with sample cases from across specialties, which are provided initially in prioritized order based on the algorithm. The input document A shows 6 sample cases. The output document B shows the same cases retrieved from the database by the Adjudicator and presented in the prioritized order based on the empiric algorithm
The Tool provides scalability because the Adjudicators are given the requests from various services in an order of priority, which can be used as a guide to place them on the OR schedule. Daily numbers of cases to perform, or rooms to open, are determined by the local Adjudicator Teams (nursing, anesthesia, proceduralist) after assessment of local resources. With a large repository of cases, they can schedule as many or as few cases as resource limitations allow. The database maintains all needed clinical information, which only needs to be entered on one occasion. This decreases manual tasks (email, phone call, or text messages) needed to arrive at a completed surgical schedule. The Tool also contains customizable columns for planning proposed surgical dates based on the preferred surgery dates entered by requesting proceduralists. This customizable column is sortable so that the schedule can be planned out, satisfying the many different scheduling requests and availability issues that arise.
This was a quality improvement initiative on an administrative process, and thus did not require patient consent or approval by the Institutional Review Board.
Currently, our team is working on a web-based link which can be sent to all surgeons with cases that have been placed on the schedule. This link will contain questions to the above defined elements regarding prioritization, and resource requirements (ICU, blood, etc.). The web-based link will populate the database, and the adjudicators will be able to generate a report all resources needed to perform all of the cases on the daily schedule. With COVID numbers rising again, this information will be accessible by the Adjudicators for rescheduling of lower priority cases in the event the hospital will not have the resources needed to finish the operative day.
Results
Between April and June, 1,767 cases were entered into the Adjudicator Tool across five hospital locations. During this time, there was a gradual ramp up of access to the operating room at each site, determined locally. This ranged from a few cases a day early on, to gradually increasing allocations of operating rooms over the two months the Adjudication Tool was in use for case prioritization. Early analysis of the discriminatory capability of the prioritization algorithm was encouraging, and the distribution of prioritization scores was normal enough that adjustment of the algorithm was not required (Fig. 4). Additionally, on retrospective review it was apparent that patients with a higher prioritization score were able to reach the operating room faster (Fig. 5).
Discussion
In his book, “The Goal”, Eliyahu Goldratt introduced the Theory of Constraints [8]. In this current crisis, surgical throughput is affected by two major constraints. The first is the availability of the hospital to provide safe facilities, adequate staff for surgical cases, or critical resources through a potential surge of COVID-19 infections. The second is the ability of the Adjudicator to digest the volume of case information being delivered by manual means. Situational awareness is heightened in the current crisis, with decisions varying day to day.
We developed an in-house Adjudication Tool to assist prioritization of a large cohort of Time Sensitive surgeries across all surgical specialties. The Tool solves a number of acute administrative issues occurring with during COVID-19 pandemic. Currently, many of the prior steps (schedulers, software, preoperative testing sites) to complete the surgical schedule cannot be completed without prioritization. Schedulers may not possess the needed clinical insight to prioritize surgical requests to those who need the resources the most. Scheduling software efficiently handles case volumes but loses efficacy when there are no block schedules to manage and there is no prioritization mechanism.
We considered several potential modes to adjudicate the large volume of pending Time Sensitive requests. Of great concern was the pressure that would be placed on site Adjudicators from individual proceduralists vying to protect the interests of their patients. In many cases, the Adjudicators may not possess enough discerning knowledge of the content to be able to make strategic decisions on behalf of patients from several different surgical specialties. Proceduralists would often lack insight into the current resource constraints of the system and may have more trouble adapting to the larger view needed in a resource constrained environment. The Tool also provided some consistency between adjudicators that were at different hospitals within the same healthcare system.
This Tool has allowed for basic stratification which has been defensible with a large number of cases input in a short time. This is scalable for the Adjudicator, and the hospital as the case backlog increases during COVID-19 plateau or decline. It allows for elimination of many prior required communications which frees up all parties to focus on getting our systems back to patient care.
Our current work to develop a web-based link that can be emailed to all surgeons with cases on the schedule will soon be in use which will greatly facilitate gathering the needed information for upcoming surgical cases. Currently, our most pressing resource limitation is the need for postoperative intensive care unit beds. The surgeons will receive links to fill out the data needed to generate prioritization scores for all cases, as well as documenting the potential needs for resources that may be limited. This will allow Adjudicators to be able to generate a daily report of the accurate resource requirements for the case in the following days, in case some curtailing of the schedule may be needed. In that event, the prioritization scores will serve as a guide for which cases may come off the schedule first.
Prachand, et al. published an elegant alternate scoring system designed for a similar purpose [9]. Their system uses 21 separate variables to construct a score, many of which, in our system, would be used for filtering rather than prioritization. This is a fundamental difference. Our solution also involves a database approach which addresses a number of logistical concerns for all users, namely decreasing voluminous manual communication that many proceduralists are currently experiencing. Our solution also provides the ability to calculate the priority score in an automated fashion and the ability to track pending cases and build daily operating room schedules in advance while being able to factor in both medical prioritization by the scoring system and resource constraints. Both methods have merit, and many can make use of these expedited publications to craft their own systems for adjudication.
There are drawbacks and limitations to this automated approach. We are fortunate to have a database engineer with the skill set to create this Tool. The initial calculator was created by physicians and is easily reproducible in a basic spreadsheet. Expansion beyond a simple calculator to a multi-user automated database requires help from someone with the proper skill set. It would be of great interest for our tool to be sharable to all who need it. The system also relies on the service chiefs properly vetting the cases and the time urgency represented by the requesting surgeons for accuracy.
We have provided the code for both the database and the interface documents for those wishing to implement the solution locally and who have IT support to integrate the system within their network.
Conclusion
The Adjudicator Tool was rapidly developed over several days and became invaluable in our processes for prioritization of Time Sensitive surgeries during our recovery. Importantly, this is a data-driven tool which allows for objectivity and consistency of prioritization across multiple adjudicators and specialties. This construct is reproducible, and it is of great interest that this learning curve can be of use to others.
References
Emanuel E, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, Phillips J (2020) Fair Allocation of Scarce Medical Resources in the Time of COVID-19. N Engl J Med 382:2049–2055
Ethics ACoSCo. COVID-19 and Surgery: Ethical Considerations. https:;//www.facs.org/covid-19/ethics. Published 2020. Accessed.
Marron J, Joffe S, Jagsi R, Spence R, Hlubocky F (2020) Ethics and Resource Scarcity: ASCO Recommendations for the Oncology Community During the COVID19 Pandemic. J Clin Onc 38:2201–2205
Ross S, Lauer C, Miles W, Green J, Christmas A, May A, Matthews B (2020) Maximizing the Calm Before the Storm: Tiered Surgical Response Plan for Novel Coronavirus (COVID-19). J Am Coll Surg 230:1080–1091
Surgeons ACo. COVID-19: Elective Case Triage Guidelines for Surgical Care. 2020.
Administration SS. Period Life Table, 2016. https://www.ssa.gov/oact/STATS/table4c6.html. Published 2017. Accessed.
Institute NC. Reports on Cancer. https://seer.cancer.gov.archive/csr/1975_2014/browse_csr.php?sectionSEL=1&pageSEL=sect_01_table.05.html. Published 2020. Accessed.
The Goal [sound recording]. St. Paul, Minn.: Penguin Highbridge Audio: 1993.
Prachand V, Milner R, Angelos P, Posner M, Fung J, Agrawal N, Jeevanandam V, Matthews J (2020) Medically Necessary, Time-Sensitive Procedures: A Scoring System to Ethically and Efficiently Manage Resource Scarcity and Provider Risk During the COVID-19 Pandemic. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2020.04.011,April9
Acknowledgements
The participants of Team 9, who worked to develop this framework. Dr. Keith Delman, Dr. Angel Leon, Dr. Carrie Cwiak, Dr. Kenneth Ogan, and Dr. Grant Carlson.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No authors have financial disclosures, and no funding has been received specific to this work. Drs. Davis, Williford, Klopman, Sweeney, and Boden and Mr. Isenburg have no conflicts of interest or financial ties to disclose relative to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Davis, S.S., Williford, M.L., Isenburg, S. et al. A scalable tool for adjudication of time sensitive cases during COVID-19 pandemic. Surg Endosc 35, 5626–5634 (2021). https://doi.org/10.1007/s00464-020-08073-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08073-7