To the Editor—During the coronavirus disease 2019 (COVID-19) pandemic, screening of asymptomatic patients for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at the time of healthcare facility admission has often been used in an effort to reduce the risk of nosocomial transmission.Reference Alsuhaibani, Kobayashi and Trannel1–Reference Uchida, Uwamino and Uno3 However, the Society for Healthcare Epidemiology of America recently recommended against routine use of asymptomatic screening in healthcare facilities, including admission screening.Reference Talbot, Hayden and Yokoe4 Such testing is of unclear benefit when other control measures are in place and may result in unintended adverse consequences, including delays in medical care and unnecessary isolation and treatment of noninfectious patients.Reference Talbot, Hayden and Yokoe4
In Veterans’ Affairs (VA) hospitals, it is recommended that all new admissions be screened for SARS-CoV-2 using a polymerase chain reaction (PCR) test. At this stage of the pandemic, PCR screening can be problematic because tests often remain positive for months after COVID-19, and undiagnosed infections are not uncommon.Reference Alsuhaibani, Kobayashi and Trannel1,Reference Talbot, Hayden and Yokoe4,Reference Aslam, Singh and Robilotti5 The cycle threshold (Ct) of the PCR test can be useful in assessing whether asymptomatic patients are infectious because high Ct values, which correlate with low viral burden, suggest a remote infection.Reference Alsuhaibani, Kobayashi and Trannel1 In previous studies, many asymptomatic patients with positive PCR tests have been deemed noninfectious based on clinical presentation, serology, and high Ct value.Reference Alsuhaibani, Kobayashi and Trannel1,Reference Aslam, Singh and Robilotti5 Here, we conducted a retrospective study to evaluate the potential benefits and adverse consequences associated with screening asymptomatic patients being admitted to a VA hospital.
The Cleveland VA Medical Center’s Research and Development Committee determined that the study was a nonresearch, quality-improvement project not requiring approval from the institutional review board. Between September 1, 2022, and January 31, 2023, we obtained the Ct values of all patients testing positive for SARS-CoV-2 on admission except those with prior COVID-19 within 90 days. The Xpert Xpress CoV-2 plus assay (Cepheid) was used for testing. Ct values were not provided in the medical record but were available to infectious diseases providers upon request. Medical records and infection control databases were reviewed to obtain information on symptoms, prior COVID-19 diagnosis, test results for COVID-19, treatment and isolation for COVID-19, and suspected transmission based on contact tracing investigations.
Patients were deemed noninfectious if the admission sample and any additional samples collected within 3 days had a Ct value >35, antigen testing (if completed) was negative, and no symptoms consistent with COVID-19 developed during the hospital admission. The Ct cutoff of 35 was chosen based on evidence that positive SARS-CoV-2 cultures, a surrogate for infectiousness, are infrequent for samples with Ct values >35.Reference Tassetto, Garcia-Knight and Anglin6–Reference Azeem, Walters, Cavalieri and Quimby8 The Ct result for the nucleocapsid (N2) target was used; if the N2 target was not detected, the highest Ct value reported for the envelope (E) or RNA-dependent RNA polymerase (RdRP) targets was used.
Of 2,794 admissions during the study, 129 (4.6%) tested positive by PCR; 54 (41.9%) were asymptomatic, 9 (7.0%) were presymptomatic, and 66 (51.2%) were symptomatic. Overall, 2.3% of hospital admissions (63 of 2,794) had positive PCR tests and were asymptomatic or presymptomatic. The mean Ct values for the asymptomatic, presymptomatic, and symptomatic patients were 35.9 (range, 15.0–44.5), 23.9 (range, 18.1–37.0), and 22.0 (range, 11.7–40.5), respectively. Of the 54 asymptomatic PCR-positive patients, 39 (72.2%) had Ct values >35 and were deemed noninfectious, 11 (20.4%) had Ct values <30, and 4 (7.4%) had Ct values between 30 and 35. Infectious diseases consultation, including review of Ct values, was obtained for 10 asymptomatic PCR-positive patients (18.5%) within 2 days of admission.
Of the 39 asymptomatic patients deemed noninfectious, 10 (25.6%) had follow-up PCR tests within 3 days of admission, and all had Ct values >35. Also, 13 (33.3%) of these patients had antigen tests within 3 days and all were negative. Furthermore, 7 (17.9%) of these patients had had COVID-19 >90 days prior to admission (range, 4–12 months). Moreover, 23 (59.0%) had had 1 or more adverse consequences: delays in medical care (N = 13) including cancelation of admissions (N = 8), unnecessary isolation (N = 9) ranging from 2 to 10 days, admission to a double-occupancy room with a roommate with acute COVID-19 (N = 1), and unnecessary COVID-19 treatment (N = 7). Table 1 provides several examples of adverse consequences associated with asymptomatic screening.
Table 1. Examples of Adverse Consequences for Asymptomatic Patients Testing Positive for SARS-CoV-2 on Admission Screening by PCR
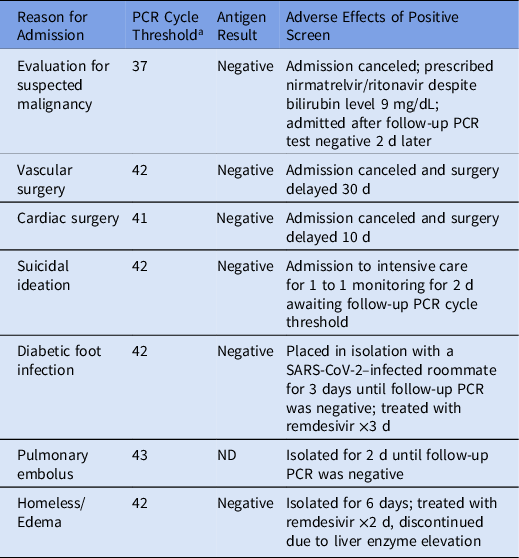
Note. PCR, polymerase chain reaction; ND, not done; N2, nucleocapsid.
a Cycle threshold for N2 target.
Our findings are consistent with those of previous studies suggesting that asymptomatic admission screening could be beneficial in reducing nosocomial transmission of SARS-CoV-2.Reference Alsuhaibani, Kobayashi and Trannel1–Reference Uchida, Uwamino and Uno3 Admission screening detected 9 presymptomatic patients and 15 asymptomatic patients with Ct values <35, including 11 with Ct value <30. Such patients may contribute substantially to transmission, including to roommates in healthcare facilities.Reference Johansson, Quandelacy and Kada9,Reference Cadnum, Jencson, Alhmidi, Zabarsky and Donskey10 However, it is not clear that universal admission screening adds benefit in settings where multiple control measures are in place, including masking of personnel during patient care.Reference Alsuhaibani, Kobayashi and Trannel1 An alternative approach might involve targeted screening of patients being admitted to double-occupancy rooms or to high-risk areas such as oncology wards.
Our findings also highlight the potential for adverse consequences of asymptomatic admission screening using PCR-based assays. 72% of the asymptomatic patients testing positive by PCR were deemed noninfectious based on clinical presentation and Ct values >35. Furthermore, 18% of these patients had prior SARS-CoV-2 infection 4–12 months before admission, probably with persistent positive PCR results. Others likely had undocumented prior infections. Asymptomatic but noninfectious patients experienced a variety of adverse effects, including delays in care and unnecessary isolation and treatment. Although Ct values must be interpreted with caution,Reference Tassetto, Garcia-Knight and Anglin6–Reference Azeem, Walters, Cavalieri and Quimby8,Reference Cadnum, Jencson, Alhmidi, Zabarsky and Donskey10 our results are consistent with previous reports suggesting that Ct values can be a useful adjunct in evaluation of asymptomatic patients testing positive on admission.Reference Alsuhaibani, Kobayashi and Trannel1
Acknowledgments
Financial support
This research was supported by the Department of Veterans’ Affairs.
Conflicts of interest
C.J.D. has received research grants from Clorox, Pfizer, and PDI. All other authors report no conflicts of interest relevant to this article.






