Abstract
Background
Meta-analyses of observational studies report a 1.1–1.7% pooled risk of stroke among patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection requiring hospitalization, but consultations for stroke and reperfusion procedures have decreased during the outbreak that occurred during the first half of the year 2020. It is still unclear whether a true increase in the risk of stroke exists among patients with coronavirus disease 2019 (COVID-19). In-hospital ischemic stroke (IHIS) complicated the 0.04–0.06% of all admissions in the pre-COVID-19 era, but its incidence has not been assessed among inpatients with COVID-19. We aimed to compare IHIS incidence among patients with SARS-CoV-2 infection with that of inpatients with non-COVID-19 illnesses from the same outbreak period and from previous periods.
Methods
This historical cohort study belongs to the COVID-19@Vallecas cohort. The incidence of IHIS was estimated for patients with SARS-CoV-2 hospitalized during March–April 2020 [COVID-19 cohort (CC)], for patients with non-COVID-19 medical illness hospitalized during the same outbreak period [2020 non-COVID-19 cohort (20NCC)], and for inpatients with non-COVID-19 illness admitted during March–April of the years 2016–2019 [historical non-COVID-19 cohort (HNCC)]. Unadjusted risk of IHIS was compared between the three cohorts, and adjusted incidence rate ratio (IRR) of IHIS between cohorts was obtained by means of Poisson regression.
Results
Overall, 8126 inpatients were included in this study. Patients in the CC were younger and more commonly men than those from the HNCC and 20NCC. Absolute risk of IHIS was 0.05% for HNCC, 0.23% for 20NCC, and 0.36% for CC, (p = 0.004 for HNCC vs. CC). Cumulative incidence for IHIS by day nine after admission, with death as a competing risk, was 0.09% for HNCC, 0.23% for 20NCC, and 0.50% for CC. In an adjusted Poisson regression model with sex, age, needing of intensive care unit admission, and cohort (HNCC as reference) as covariates, COVID-19 was an independent predictor for IHIS (IRR 6.76, 95% confidence interval 1.66–27.54, p = 0.01). A nonsignificant increase in the risk of IHIS was observed for the 20NCC (IRR 5.62, 95% confidence interval 0.93–33.9, p = 0.06).
Conclusions
SARS-CoV-2 outbreak was associated with an increase in the incidence of IHIS when compared with inpatients from a historical cohort. Viral infection itself may be related to the increased risk of IHIS among patients with COVID-19, but in view of our results from the 20NCC, it is likely that other factors, such as hospital saturation and overwhelming of health systems, may have played a role in the increased frequency of IHIS.
Similar content being viewed by others
Introduction
Case series and cohort studies report a relatively high frequency of stroke among patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [1,2,3,4]. Meta-analyses have estimated a 1.1–1.7% pooled risk of ischemic stroke among patients with this disease requiring hospitalization [5,6,7,8], and one population-based study yielded a ≈10 times higher incidence of ischemic stroke during the first 14 days after Coronavirus disease 2019 (COVID-19) diagnosis [9]. COVID-19 has been also associated with an increased risk of large-vessel occlusion strokes and with worse functional outcome and higher mortality than strokes among patients with non-COVID-19 illness [10,11,12,13]. Several physiopathological hypotheses have been suggested for these observations. Angiotensin-converting enzyme-2 receptor expression in arterial smooth muscle cells, specifically in the brain vessels, may have relevance in the presentation of acute ischemic strokes [14]. In addition, an acquired syndrome known as COVID-19-associated coagulopathy has emerged to be frequent, multifactorial, and involve venous, arterial, and microcirculatory systems [15]. Also, it is possible that more severe COVID-19 is related to a higher risk of thrombosis mediated by cytokine storm and immuno-inflammation [16].
As an apparent paradox, consultations for stroke and reperfusion procedures have decreased during the SARS-CoV-2 outbreak that occurred during the first half of the year 2020 [17,18,19,20]. This has been attributed to the fear of being exposed to SARS-CoV-2 and has caused a delay in seeking medical attention or even avoiding consultation, a reduced detection of stroke due to isolation, or overwhelmed emergency medical systems [21]. However, it is still unclear whether a true increase in the risk of stroke exists among patients with COVID-19 [22]. Epidemiological evidence assessing the actual risk of stroke associated with SARS-CoV-2 infection is scarce, probably because of the difficulty of obtaining reliable data at a population level during the pandemic. To overcome this limitation, we aimed to compare the incidence of in-hospital ischemic stroke (IHIS) among patients with SARS-CoV-2 infection during the COVID-19 outbreak with the incidence of IHIS among patients with non-COVID-19 illness. IHIS represents the 2–17% of all strokes [23] and has been reported to complicate the 0.04–0.06% of all admissions in the pre-COVID-19 era [24, 25]. Analysis of the incidence of IHIS would allow for the evaluation of the risk of ischemic stroke associated with COVID-19, assuming that any event occurring during hospitalization would cause medical consultation, and would therefore be more easily identified.
Methods
This historical cohort study belongs to the COVID-19@Vallecas cohort and received approval from the Infanta Leonor Hospital research ethics committee, who waived written informed consent because of its retrospective design. Our institution is composed of a 260-bed acute care facility (the Hospital Universitario Infanta Leonor) and a 100-bed rehabilitation and long-term care facility (the Hospital Virgen de la Torre), both in the neighborhood of Vallecas, Madrid, Spain. Our institution received the first confirmed case of SARS-CoV-2 infection on March 1, 2020, and then rapidly became a de facto COVID-19 hospital, reaching a maximum of 569 inpatients with confirmed or suspected SARS-CoV-2 infection at the peak of the pandemic. Patients with confirmed or suspected COVID-19 were admitted if they presented with any of the following: basal oxygen saturation < 95%, tachypnea with breathing rate ≥ 24 per minute, dyspnea, bilateral interstitial lung infiltrates on chest X-ray, or, at criteria of the attending physician, if they had other clinical or analytical risk factors for developing an unfavorable evolution of the disease (e.g., patients who are immunocompromised, previous lung disorders, active malignancies).
Characteristics and outcomes of the patients included in the COVID-19@Vallecas cohort have been described elsewhere [26]. Briefly, the cohort was composed of more than 2200 patients (57% men) with a median age of 69 years. The prevalence of hypertension was 55%, of diabetes 24%, and of obesity 16%. Of all the patients, 14% had acute respiratory distress syndrome, and 6% of inpatients were admitted to the intensive care unit (ICU). Cumulative incidence of ischemic stroke in the cohort was 1.4% by day ten [27]. During the first weeks of the outbreak, admitted patients received thromboprophylaxis with 20 or 40 mg of subcutaneous enoxaparin (depending on body weight and kidney function) unless contraindicated. By April 9, 2020, because of the recommendations from the Spanish Society of Thrombosis and Hemostasis, a dosage-escalating protocol was implemented. This enhanced thromboprophylaxis protocol recommended treatment with subcutaneous enoxaparin 40 mg per 24 h for those inpatients with body weight < 60 kg or age > 75 years; 60 mg per 24 h for those patients with body weight of 60–100 kg; and 80 mg per 24 h if weight was > 100 kg. Those patients considered to be at a high thrombotic risk received treatment with enoxaparin 1 mg/kg/24 h (0.75 mg/kg/24 h if age > 75 years), and the dosage was up to 0.75–1 mg/kg/12 h for patients who were critically ill. These dosages were reduced if filtration rate estimated by the MDRD-4 was < 30 ml/minute/1.73 m2 [27]. The degree of compliance with the two different protocols in the COVID-19@Vallecas cohort was 92.5% from March 3 to April 8 and 97.9% from April 9 onward.
For the present study, we established three clinical cohorts: (1) the COVID-19 cohort (CC) included those inpatients testing positive to SARS-CoV-2 by means of polymerase chain reaction (PCR) (nasopharyngeal swab) between March 1 and April 3, 2020; (2) the 2020 non-COVID-19 cohort (20NCC) included those inpatients with a negative result of PCR to SARS-CoV-2 who were hospitalized in medical specialty wards (i.e., cardiology, endocrinology, gastroenterology, geriatrics, hematology, internal medicine, nephrology, neurology, oncology, palliative care medicine, pulmonary medicine, and rheumatology) and/or the ICU during the period from March 1 to April 30, 2020; and (3) those inpatients admitted during the months of March and April of the years 2016 to 2019, which were considered previous equivalent periods, formed the historical non-COVID-19 cohort (HNCC). Inpatients admitted to surgical wards were excluded to increase the comparability of cohorts. Time at risk was obtained for all patients who generated at least 1 day of hospital stay in medical specialty wards. Only the stays generated during the 61-day study periods of the included years were considered to calculate the incidence of IHIS. Follow-up time was the time elapsed between admission and IHIS, discharge, or death (whatever happened earlier), and was censored by April 30, 2020, for patients who remained admitted at the end of the study period.
Patients who presented with IHIS were identified from hospital databases [codes I63 to I66 of the 10th version of the International Classification of Diseases (ICD-10)] [28] and cross-ascertained with in-hospital neurological consultation registers. Two authors (FSH and EAR) independently reviewed the available clinical information on the episodes that had received an ICD-10 secondary diagnosis of ischemic stroke at discharge. Only those inpatients with registered clinical evidence of an acute, new onset focal neurological impairment during hospitalization compatible with a neurovascular syndrome and meeting World Health Organization criteria for the clinical diagnosis of stroke [29] and a confirmed brain infarction on brain imaging testing (computed tomography and/or magnetic resonance imaging), topographically congruent with clinical presentation, were recorded as having an IHIS. Etiology of IHIS was diagnosed according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) stroke subtype classification system [30]. A principal diagnosis of pneumonia was given to those patients coded with J12 to J18 of the ICD-10. Severe pneumonia was defined by the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) criteria [31].
Data were collected using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Ideas for Health Association. REDCap is a secure, Web-based software platform designed to support data capture for research studies [32]. Data on pneumonia severity were missing for 139 patients. No other missing data existed. Analysis was performed using Stata 12 (StataCorp LLC, College Station, TX). Frequencies of categorical variables are expressed as numbers and percentages, and results of discrete or continuous variables are reported as medians and interquartile ranges (IQRs). For their comparisons, χ2 or Kruskall–Wallis tests were applied when appropriate. When differences were observed, between-group comparisons applying the Bonferroni correction were done.
Several analyses were performed on the three cohorts to assess the risk of IHIS. Firstly, absolute frequencies of IHIS were compared applying χ2 tests, with the Bonferroni correction for multiple comparisons. Secondly, cumulative incidences of IHIS were estimated by the multiple decrement model, with death as a competing risk [33]. Thirdly, unadjusted incidence rates for IHIS were calculated by dividing the number of events observed by the number of person-days recorded within each group. Unadjusted incidence rate ratios (IRR) were obtained. Finally, Poisson regression allowed us to obtain IRR of IHIS between cohorts after covariate adjustment. A value of p < 0.05 was considered significant.
Results
Overall, 8126 inpatients were included in this study. During the period of March and April 2020, 2546 patients were hospitalized (median age 72 years, IQR 57–83 years) and generated 19,938 stays (i.e., person-days) (Fig. 1). Of them, 1673 tested positive for SARS-CoV-2 (the CC) and 873 tested negative (the 20NCC). During the period of March and April of the years 2016 to 2019 (the HNCC), 5,580 admissions in medical wards and/or ICU were recorded. Patients in the CC were younger and more commonly men than their counterparts from the HNCC and the 20NCC (for sex, χ2 = 29.4, p < 0.001; and for age, H0 = 188.7, p < 0.001) (Table 1). The CC had shorter median hospital stay than the HNCC (t = 2.6, p = 0.03) but not than the 20NCC (t = 1.0, p = 0.70). Among the CC, 239 of 1534 (15.6%) patients presented with severe pneumonia at the time of admission to the emergency department according to IDSA/ATS criteria, and 89 patients (5.3%) were admitted to ICU during hospitalization. Overall, 404 inpatients from the CC (24.2%) required admission to ICU, invasive or noninvasive mechanical ventilation, and/or died during the hospitalization episode. The highest percentage of inpatients who died was that of the CC (17.2%). The 20NCC had a higher frequency of death in the hospital (12.4%) than that of the HNCC (9.3%) (χ2 = 8.2, p = 0.008).
Eleven out of 8126 patients (0.014%) included in this study had a confirmed IHIS in the total study period (March–April of the years 2016–2020). Three of them occurred during the years 2016–2019 (two cardioembolic; one of other determined etiology), accounting for the 0.05% of the HNCC. Two out of 873 inpatients with non-COVID-19 illness from the 20NCC (0.23%; one cardioembolic; one of undetermined etiology) and six patients from the CC (0.36%; one cardioembolic; and five of undetermined origin, three of which had incomplete evaluation), who’s clinical and imaging features have been previously reported elsewhere [34], had IHIS (Table 2, Fig. 2). The difference in IHIS frequency was significant for the comparison between the HNCC and the CC (χ2 = 9.7, p = 0.004) but was not between the 20NCC and the CC (χ2 = 0.31, p = 1.0). One IHIS occurred among 193 inpatients with non-COVID-19 illness, with a principal diagnosis of pneumonia from the 20NCC (0.5%), and none among the 384 inpatients with a principal diagnosis of pneumonia from the HNCC. The frequency of stroke among patients with COVID-19 pneumonia was 6 of 1430 (0.4%; Fisher’s exact test, p = 0.51).
Number of patients who were hospitalized during the SARS-CoV-2 outbreak period (March and April 2020). Diamonds denote the dates of IHIS, blue denotes patients who tested positive to SARS-CoV-2, and yellow denote patients who tested negative to SARS-CoV-2. IHIS In-hospital ischemic stroke, SARS-CoV-2 Severe acute respiratory syndrome coronavirus 2
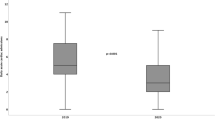
All IHIS occurred within the first nine days of hospital stay in all cases. Cumulative incidence for IHIS by day nine after admission, with death as a competing risk, was 0.09% [95% confidence interval (CI) 0.03–0.26%] for the HNCC; 0.23% (95% CI 0.05–0.79%) for the 20NCC; and 0.50% (95% CI 0.20–1.10%) for the CC (Fig. 3). Unadjusted incidence rates for IHIS were 0.65 per 10,000 person-days in the HNCC, 3.31 per 10,000 person-days in the 20NCC, and 4.32 events per 10,000 person-days in the CC (between HNCC and CC, IRR = 6.6, 95% CI 1.4–40.8, p = 0.004; between HNCC and 20NCC, IRR = 5.1, 95% CI 0.4–44.2, p = 0.12; and between 20NCC and CC, IRR = 1.3, 95% CI 0.2–13.2, p = 0.79).
In an adjusted multivariate model (Poisson regression) with IHIS as the dependent variable and sex (female sex as reference), age, need of ICU admission during hospitalization, and cohort (HNCC as reference) as covariates, COVID-19 diagnosis was an independent predictor for IHIS, with an IRR of 6.76 (95% CI 1.66–27.54, p = 0.01; Table 3). An increased, not statistically significant adjusted risk of IHIS was also observed for the 20NCC with respect to the HNCC (IRR = 5.62, 95% CI 0.93–33.9, p = 0.06).
Discussion
This study shows that, compared with a historical cohort of patients with non-COVID-19 medical illness, those patients hospitalized with COVID-19 during the SARS-CoV-2 outbreak had a sixfold increase in the adjusted incidence of IHIS. Despite being younger, the risk of stroke during admission was higher for patients from the CC than for patients from the non-COVID cohorts. The frequency of IHIS in our CC was lower than that of other series that reflect a > 1% absolute risk of stroke among patients who were hospitalized with COVID-19 [5,6,7,8]. As opposed to these series, our cohort only included patients having a stroke during admission because of COVID-19 and excluded those patients presenting with stroke and SARS-CoV-2 infection at the time of admission. This point is a strength of the present study because it allows comparison of IHIS incidence with historical controls, and it is also a limitation because it does not allow for generalization of the results to a population level or comparisons with others works on stroke incidence among patients with COVID-19.
Controversial data exist on the association of stroke and COVID-19 due to contradictory results of the studies assessing the first months of the year 2020 [35]. At the hospital level, meta-analyses of cases series and cohort studies suggest an increased risk of ischemic stroke among patients with this disease [5,6,7,8], but stroke codes and reperfusion procedures have decreased respecting the prepandemic era [17,18,19,20]. When compared with other viral diseases, the proportion of hospitalizations complicated by any thrombosis was higher in patients with COVID-19 than in patients with viral respiratory illness during 2002–2014 [36]. In contrast, some studies have not replicated the previously reported findings of increased presentation of young patients with large-vessel occlusion stroke nor have identified increased stroke severity or delays in stroke presentation [37]. Another previous hospital study showed that the odds of stroke was 0.25 times less likely in patients with COVID-19 in comparison with noninfected individuals during SARS-CoV-2 outbreak in New York State [38]. At a population level, a nationwide Danish study obtained an increased risk of stroke of more than ten times related to a recent diagnosis of COVID-19 [9], but a Chinese population-based prospective cohort study showed a decrease in the community incidence of ischemic stroke [39].
Interestingly, incidence of IHIS in our study was also increased among non-COVID-19 inpatients admitted during the SARS-CoV-2 outbreak, although adjusted estimation of the IRR for the 20NCC compared to the HNCC was not significant. A similar result was obtained in a previous work, finding acute ischemic stroke being infrequent in patients with COVID-19 (1.3%) and a similar prevalence (1%) of ischemic stroke being observed among patients without COVID-19 [40]. These results may have several concurrent causes. Firstly, a true increase of IHIS incidence may have been caused by hospital saturation, which potentially led to a suboptimal quality of hospital care to all inpatients admitted during the outbreak. Secondly, sample size of our study is relatively low taking into account that IHIS is an uncommon outcome, so small random changes in absolute frequency of stroke in any cohort may have led to underestimation or overestimation of the true risk. And finally, some patients may have been misclassified as patients with non-COVID-19 illness. It is noteworthy that both age and length of stay were lower in the 20NCC than in the HNCC, similarly to which occurred in the CC, and they received a principal diagnosis of pneumonia more commonly than historic controls (22.1% vs. 6.9%). So, some of these patients may have had a SARS-CoV-2 infection that could not be demonstrated for several reasons (e.g., low suspicion index at the beginning of the outbreak, or patients with a first negative PCR to SARS-CoV-2 dying early after admission and therefore not being able to confirm the diagnosis in successive tests).
Our study has other limitations. We acknowledge that these findings may be eventually influenced by noncontrolled variables such as vascular risk factors, which were not obtained from non-COVID-19 cohorts for this study. Furthermore, the association of COVID-19 and stroke among admitted patients may overestimate its true relationship, taking into account that most patients with SARS-CoV-2 infection present with mild forms of the disease and do not require hospital admission. Also, our results may not be generalizable to other settings or health systems. Finally, we cannot fully establish causality based on observational evidence provided by our study or previous ones.
Conclusions
Our results suggest that SARS-CoV-2 outbreak was associated with an increase in the incidence of IHIS. Viral disease itself may be related to the increased risk of IHIS among patients with COVID-19 but, in view of our results from the 20NCC, it is likely that hospital saturation and overwhelming of health systems may have played an important role in the increased frequency of IHIS. We have estimated an unadjusted incidence of approximately four ischemic strokes per 10,000 hospital stays of patients with COVID-19 and three ischemic strokes per 10,000 hospital stays of patients with COVID-19 during the COVID-19 outbreak. Stroke care protocols must be optimized to face a potential increase of events in the hospital associated with SARS-CoV-2 outbreaks. This may be challenging in the context of the logistical constraints laid down by the pandemic (e.g., patient isolation, personal protection equipment, limitation of in-hospital transfers). Additional epidemiological research is needed to confirm these results in larger hospital cohorts and, ideally, at the community level.
References
Avula A, Nalleballe K, Narula N, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020;87:115–9.
Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60.
Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91:889–91.
Yaghi S, Ishida K, Torres J, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51:2002–11.
Tsivgoulis G, Katsanos AH, Ornello R, Sacco S. Ischemic stroke epidemiology during the COVID-19 pandemic: navigating uncharted waters with changing tides. Stroke. 2020;51:1924–6.
Katsanos AH, Palaiodimou L, Zand R, et al. The impact of SARS-CoV-2 on stroke epidemiology and care: a meta-analysis. Ann Neurol. 2021;89:380–8.
Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A, Young B. Stroke as a neurological complication of COVID-19: a systematic review and meta-analysis of incidence, outcomes and predictors. J Stroke Cerebrovasc Dis. 2021;30:105549.
Parsay S, Vosoughi A, Khabbaz A, Sadigh-Eteghad S. The incidence and mortality ratio of ischemic cerebrovascular accidents in COVID-19 cases: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2021;30:105552.
Modin D, Claggett B, Sindet-Pedersen C, et al. Acute COVID-19 and the incidence of ischemic stroke and acute myocardial infarction. Circulation. 2020;142:2080–2.
Kihira S, Schefflein J, Mahmoudi K, et al. Association of coronavirus disease (COVID-19) with large vessel occlusion strokes: a case-control study. AJR Am J Roentgenol. 2021;216:150–6.
Majidi S, Fifi JT, Ladner TR, et al. Emergent large vessel occlusion stroke during New York City’s COVID-19 outbreak: clinical characteristics and paraclinical findings. Stroke. 2020;51:2656–63.
Ntaios G, Michel P, Georgiopoulos G, et al. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke. 2020;51:e254–8.
Fuentes B, Alonso de Leciñana M, García-Madrona S, et al. Stroke acute management and outcomes during the COVID-19 outbreak: a cohort study from the Madrid stroke network. Stroke. 2021;52:552–62.
Hamming I, Timens W, Bulthuis M, Lely A, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7.
Becker R. COVID-19 update: Covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020;50:54–67.
Guo L, Rondina MT. The era of thromboinflammation: platelets are dynamic sensors and effector cells during infectious diseases. Front Immunol. 2019;10:2204.
Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–1.
Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001.
Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 2020;51:2315–21.
Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29:104953.
Rudilosso S, Laredo C, Vera V, et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51:1991–5.
Altable M, de la Serna JM. Cerebrovascular disease in COVID-19: Is there a higher risk of stroke? Brain Behav Immun Health. 2020;6:100092.
Cumbler E. In-hospital ischemic stroke. Neurohospitalist. 2015;5:173–81.
Park HJ, Cho HJ, Kim YD, et al. Comparison of the characteristics for in-hospital and out-of-hospital ischaemic strokes. Eur J Neurol. 2009;16:582–8.
Azzimondi G, Nonino F, Fiorani L, et al. Incidence of stroke among inpatients in a large Italian hospital. Stroke. 1994;25:1752–4.
Jiménez E, Fontán-Vela M, Valencia J, et al. Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: a retrospective case series study. BMJ Open. 2020;10:e042398.
Muñoz-Rivas N, Abad-Motos A, Mestre-Gómez B, et al. Systemic thrombosis in a large cohort of COVID-19 patients despite thromboprophylaxis: a retrospective study. Thromb Res. 2021;199:132–42.
Ministerio de Sanidad, Consumo y Bienestar Social. CIE-10-ES Diagnósticos 2020. https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc.html. Accessed 21 Aug 2020.
The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–14.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27-72.
Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Coviello V, Boggess M. Cumulative incidence estimation in the presence of competing risks. Stata J. 2004;4:103–12.
Sierra-Hidalgo F, Muñoz-Rivas N, Torres Rubio P, et al. Large artery ischemic stroke in severe COVID-19. J Neurol. 2020;267:3441–3.
Finsterer J, Scorza FA. Ischemic Stroke in COVID-19 Patients May Be Incidentally but Not Causally Related to the Infection. Cerebrovasc Dis 2021. Published online ahead of print, Feb 18. https://doi.org/10.1159/000513915.
Smilowitz NR, Subashchandran V, Yuriditsky E, et al. Thrombosis in hospitalized patients with viral respiratory infections versus COVID-19. Am Heart J. 2021;231:93–5.
Etherton MR, Zachrison KS, Yan Z, et al. Regional Changes in Patterns of Stroke Presentation During the COVID-19 Pandemic. Stroke 2021. Published online ahead of print, 2021 Feb 16. https://doi.org/10.1161/STROKEAHA.120.031300.
Bekelis K, Missios S, Ahmad J, et al. Ischemic stroke occurs less frequently in patients with COVID-19: a multicenter cross-sectional study. Stroke. 2020;51:3570–6.
Liu J, Yang Q, Zhang X, et al. A SHARp decline in burden of stroke in rural China during COVID-19 pandemic. Front Neurol. 2021;11:596871.
Qureshi AI, Baskett WI, Huang W, et al. Acute ischemic stroke and COVID-19: an analysis of 27 676 patients. Stroke. 2021;52:905–12.
Acknowledgements
Members of the Infanta Leonor Thrombosis Research Group: B. Mestre-Gómez, R. M. Lorente-Ramos, J. Rogado, A. Franco-Moreno, B. Obispo, D. Salazar-Chiriboga, T. Sáez-Vaquero, J. Torres-Macho, A. Abad-Motos, C. Cortina-Camarero, A. Such-Díaz, E. Ruiz-Velasco, E. Moya-Mateo, M. de Carranza-López, M. A. Herrera-Morueco, V. Pardo-Guimera, P. Medrano-Izquierdo, E. Gómez-Mariscal, K. Marín-Mori, C. Figueras-González, S. López-Lallave, J. Churruca-Sarasqueta, C. Mauleón-Fernández, J. Martín-Navarro, P. Torres-Rubio, M. J. Moro-Álvarez, J. A. Hernández-Rivas, A. Bustamante-Fermosel.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Consortia
Contributions
FSH concepted and designed the study, performed data acquisition, analysis and interpretation of the data, drafted and revised the manuscript. EAR, EMA, SMGM, and AEL performed data acquisition and revised the manuscript. PAR designed the study, performed data acquisition and revised the manuscript. NMR concepted the study, performed data acquisition and revised the manuscript. Authorship requirements have been met and, the final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Ethical approval/informed consent
The study was approved by the Hospital Universitario Infanta Leonor ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was waived because of the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sierra-Hidalgo, F., Aragón Revilla, E., Arranz García, P. et al. Increased Incidence of In-Hospital Ischemic Stroke During SARS-CoV-2 Outbreak: A Single-Center Study. Neurocrit Care 36, 208–215 (2022). https://doi.org/10.1007/s12028-021-01286-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01286-1