Epidemiology of patients with dizziness over a 3-year period, requiring utilization of the emergency medical serviced system: A pre- and post-COVID pandemic comparative study using the population-based ORION registry
Abstract
OBJECTIVE:
We aimed to identify the proportion of each medical condition or disease contributing to dizziness and their disposition in the Emergency Department (ED).
METHODS:
This retrospective, descriptive study examined data from the Osaka Emergency Information Research Intelligent Operation Network system in Japan for the period from January 1, 2018 to December 31, 2020. The inclusion criteria were patients with presumptive ICD-10 codes including “dizziness” or “vertigo”. Patient demographics were compared using the χ2 test and Kruskal-Wallis test. Logistic regression analysis was performed to calculate disposition from ED (emergency admission or discharge) over the 3-year study period. The adjusted odds ratio (OR) and 95% confidence interval (CI) were calculated using multivariate analyses.
RESULTS:
During the 3-year study period, a total of 1,346,457 patients (462,773 in 2018, 468,697 in 2019, and 414,987 in 2020; P < 0.001), including 53,190 patients with dizziness (18,396 in 2018, 18,649 in 2019, and 16,145 in 2020; P = 0.058), were identified as having been transported to hospitals by ambulance in Osaka Prefecture. Dizziness and giddiness (R42) was the most common form of dizziness, in 27,075 cases (9,570 in 2018, 9,613 in 2019, and 7,892 in 2020; P < 0.001; Gender composition showed 10,483 males and 16,592 females.) Vestibular Neuronitis (H81.2) showed significant increase in 2020 compared to the two preceding years (91 in 2018, 119 in 2019, and 130 in 2020, P = 0.003; including 174 males and 167 females, respectively). Of the 53,190 patients with dizziness, 11,862 (22.3%; 4,323 males, 7,539 females) were admitted to hospital. The odds ratio (OR) for emergency admission for dizziness in 2020 during the COVID-19 pandemic was 0.98 (95% confidence interval (CI), 0.93– 1.03) with reference to 2018.
CONCLUSION:
Patients with dizziness accounted approximately 4% of ED transportations, with about 20% requiring hospital admission, irrespective of the COVID-19 pandemic. Vestibular neuronitis was significantly increased in 2020.
1Introduction
Dizziness is a common complaint, accounting for 2– 4% of emergency department (ED) visits and leading to hospital admission in approximately 20% of cases [6, 7, 12, 16]. A report from the United States estimated that approximately 4 million patients presented to the ED with dizziness in one year [20]. However, the epidemiology of emergency dizziness in Japan has remained unclear, although one report investigated a small number of patients with dizziness in a restricted local area about 3 decades ago [13]. Osaka is the second largest metropolitan area in Japan and the prefectural core of the Kansai region, with one of Japan’s highest population densities. The Osaka prefectural government developed the Osaka Emergency Information Research Intelligent Operation Network (ORION) system, an information system for emergency patients transported by emergency medical services (EMS) personnel. The ORION system compiles prehospital ambulance records and hospital information (i.e., diagnosis and hospital course for 21 days) [17]. To the best of our knowledge, no previous studies have clarified the epidemiology of patients with dizziness associated with the EMS system in Japan.
The first positive result for coronavirus disease 2019 (COVID-19) in a Japanese patient was recorded on January 28, 2020. The World Health Organization declared a COVID-19 pandemic on March 11, 2020. Our previous study revealed an approximately 10% reduction in EMS service use among the all-ages population in 2020, possibly due to the COVID-19 pandemic, but studies of EMS related to the COVID-19 pandemic in patients with dizziness remain scarce [18, 19]. We hypothesized the decreased number of patients with dizziness using EMS in 2020 maybe directly related to the overall impact of COVID 19, however we suspect some subcategories of dizziness may represent an increase of patients utilizing EMS.
To the best of our knowledge, no clinical studies examining the influence of the COVID-19 outbreak in patients with dizziness on the EMS system have yet been published anywhere in the world. This study aimed to clarify the epidemiology of emergency dizziness transported by ambulance and its hospital course in Japan. In addition, we also assessed the influence of the COVID-19 pandemic on the patients with dizziness.
2Methods
2.1Study design and setting
This was a retrospective, descriptive study examining the period from January 1, 2018 to December 31, 2020 using the ORION system [17]. Osaka Prefecture is the largest metropolitan community in western Japan, with a population of about 8.8 million and a total area of 1905 km2. To assess the effects of the COVID-19 pandemic on the EMS system, this study focused on patients with dizziness transported by ambulance in Osaka Prefecture (Fig. 1). The presumptive diagnosis, and the final diagnosis if the patient was admitted, according to the International Classification of Diseases, 10th revision (ICD-10), were used [23]. Data were collected using the following ICD-10 codes: dizziness and giddiness, R42; epidemic vertigo, A88.1; Ménière’s disease, H81.0; benign paroxysmal vertigo, H81.1; vestibular neuronitis, H81.2; other peripheral vertigo, H81.3; vertigo of central origin; H81.4; other disorders of vestibular function, H81.8; disorders of vestibular function, unspecified, H81.9; and vertiginous syndromes in diseases classified elsewhere, H82.
Fig. 1
Patient flow. All patients with dizziness were selected and then divided into two groups (admission from the ED and non-admission from the ED).
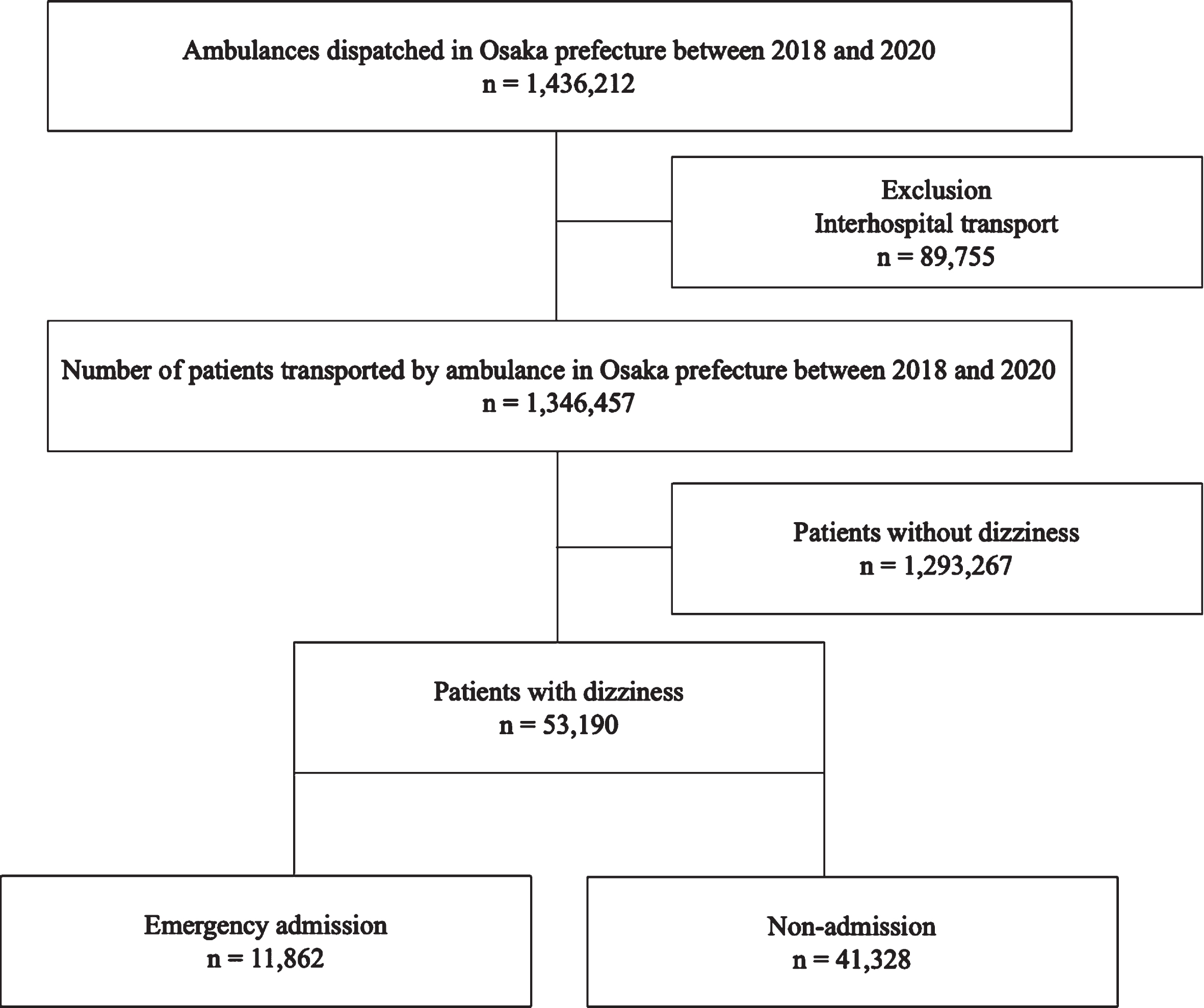
This study excluded patients who were not transported to a hospital and patients who were transported or transferred to another hospital from the ED (Interhospital transport).
The ambulance records in Osaka Prefecture are considered administrative records, and the need to obtain informed consent from individual participants was waived because the data had been anonymized. This study was approved by the Ethics Committee of Osaka Medical and Pharmaceutical University (Takatsuki City, Japan). Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines were used to design and report the results of this study [8].
2.2The Osaka prefectural government developed the Osaka Emergency Information Research Intelligent Operation Network (ORION) system
The Osaka prefectural government has developed and introduced the ORION system as an information system for emergency patients that uses a smartphone application for hospital selection by on-scene EMS personnel. The ORION system has been collecting all ambulance records. Medical institutions have obtained information on the diagnoses and outcomes of patients transported to medical institutions, and the ORION system has merged these data with ambulance records, including smartphone application data, since January 2015.
2.3Data collection and quality control
Data were uniformly collected using specific data collection forms and included the reason for the ambulance call, location of the accident, the time of day and the day of the week, and tools used, in addition to age, sex, and ICD-10 code. The detailed situation and patient information were recorded in text form. These data were completed by EMS personnel then transferred to the information center in the Osaka Municipal Fire Department. To ensure the quality of the data, data sheets showing incomplete information were supposed to be returned to the relevant EMS personnel for correction.
2.4Outcomes
The primary outcome was to identify the proportion of each disease entity associated with dizziness and the respective disposition in the ED for the 3-year period under study, including the COVID-19 pandemic. The secondary outcome was to elucidate the broader influence of COVID-19 pandemic on acute dizziness including its prevalence and hospital course.
2.5Data analysis
The number of patients transported by ambulance due to any cause other than interhospital transport was calculated for the year from January 1 to December 31, 2020. Patient demographics were compared among the three years using the χ2 test for categorical variables and the Kruskal-Wallis test for continuous variables. Patients presented via EMS were reported by age in 10-year increments as well as by gender. Vital signs of patients presented via EMS were collected. For the purposes of comparison, the numbers of patients transported by ambulance for the same reasons per year from January 1 to December 31, 2018, and from January 1 to December 31, 2019 were also collected. Logistic regression analysis was used to calculate the disposition at the ED, such as emergency admission, discharged to home, and death in the ED to which the patient was transported for the 3-year study period, and the adjusted odds ratio (OR) and 95% confidence interval (CI) were calculated using multivariate analyses for each year for admission (using 2018 as the reference), each disease of dizziness (using dizziness and giddiness [R42] as the reference), sex, time of transportation (using night time 17 : 00– 09 : 00 as the reference), day of the week (using the weekend as the reference), and age categories. The adjusted OR and 95% CI of disposition in the ED were also calculated in patients with dizziness using multivariate analyses including year, each disease of dizziness, sex, time of transportation (nighttime 17 : 00– 09 : 00), day of the week (weekend), and age categories. Patient vital signs were compared between emergency admission and non-admission groups using the Wilcoxon rank-sum test. All data were analyzed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA) or STATA (version 16.1; Stata Corp., College Station, TX, USA). All tests were two-tailed, and p-value < 0.05 were considered significant.
3Results
3.1Results relating to transport to hospital
For the 3-year period between January 1, 2018, and December 31, 2020, a total of 1,436,212 patients were transported to hospital by ambulance in Osaka Prefecture. Of these, 1,346,457 patients were enrolled in this study. The remaining 89,755 patients had been transferred to a different hospital (interhospital transport) and were thus excluded. By year, 462,773 patients in 2018, 468,697 patients in 2019, and 414,987 patients in 2020 were transported to hospital by ambulance, with a total of 53,190 patients showing dizziness (18,396 in 2018, 18,649 in 2019, and 16,145 in 2020; P = 0.058). Figure 1 displays the flow diagram for this study. Baseline characteristics of patients transported to hospitals by ambulance in Osaka Prefecture are shown in Table 1. Dizziness and giddiness (R42) was the most common ICD-10 code for dizziness, seen in 27,075 patients (9,570 in 2018, 9,613 in 2019, and 7,892 in 2020; P < 0.001). Vestibular neuronitis (H81.2) was significantly increased in both absolute number and prevalence in 2020 compared with the other years (91 in 2018, 119 in 2019, and 130 in 2020; P = 0.003) (Fig. 3). Age category and sex differences for patients with dizziness are shown in the Fig. 2 and Supplemental Table 8. Female patients were more common than male patients, with a female-to-male ratio of approximately 1.7. The age strata of patients in their seventies showed the greatest frequency and number of dizziness patients.
Fig. 2
Age category and sex differences for total number of patients with dizziness. Blue: male. Red: female. X axis was ten-year age categories. Y axis was number of patients. Female patients were more common than male patients in all ten-year age categories. The age strata of patients in their seventies showed the greatest frequency and number of dizziness patients.
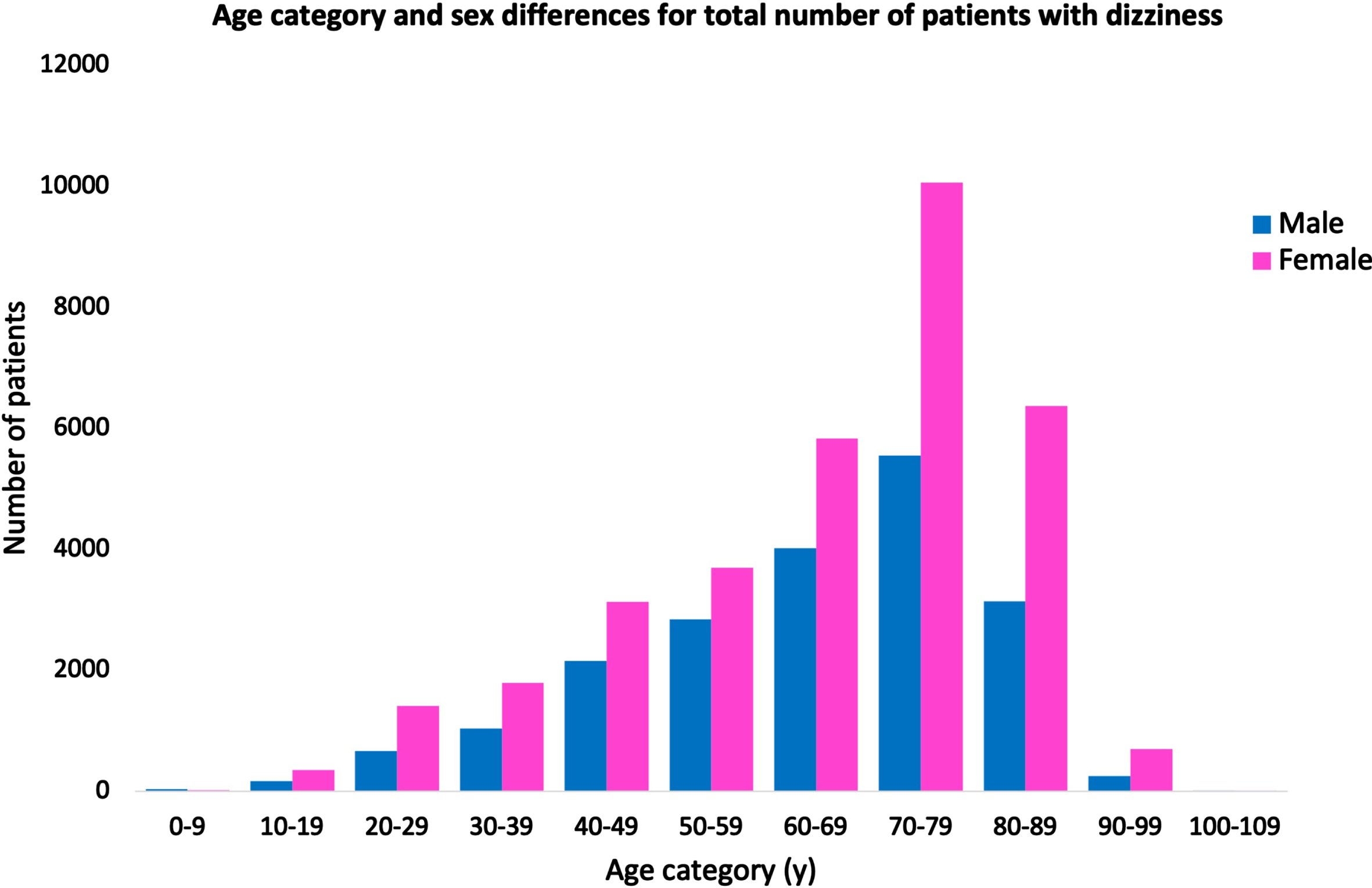
Fig. 3
Age categories for patients with benign paroxysmal vertigo and vestibular neuronitis for each year. Green: benign paroxysmal vertigo. Orange: vestibular neuronitis. X axis was ten-year age categories. Y axis was number of patients. Patients younger than 50 years old with both benign paroxysmal vertigo and vestibular neuronitis were increased in 2020 compared with other years.

Table 1
Demographic characteristics of transported patients
| Year | 2018 | 2019 | 2020 | Total | P value |
| Number of patients | 462,773 | 468,697 | 414,987 | 1,346,457 | <0.001 |
| Age, median (IQR) | 69.0(38) | 70.0(38) | 71.0(35) | <0.001 | |
| Sex (male), % | 234,542 (50.7) | 236,661 (50.5) | 210,334 (50.7) | 681,537 (50.6) | 0.111 |
| Age, median (IQR) | 67.0 (38) | 67.0 (38) | 69.0 (34) | <0.001 | |
| Children, % | 35,314 (7.6) | 37,547 (8.0) | 24,697 (6.0) | 97,558 (7.3) | <0.001 |
| Age, median (IQR) | 3.0 (7) | 3.0 (7) | 4.0 (7) | <0.001 | |
| Adults, % | 166,402 (36.0) | 164,722 (35.1) | 143,740 (34.6) | 474,864 (35.3) | <0.001 |
| Age, median (IQR) | 43.0 (26) | 44.0 (26) | 45.0 (26) | <0.001 | |
| Elderly patients, % | 261,057 (56.4) | 266,428 (56.8) | 246,550 (59.4) | 774,035 (57.5) | <0.001 |
| Age, median (IQR) | 80.0 (12) | 80.0 (12) | 80.0 (12) | <0.001 | |
| Total number with dizziness, % | 18,396 (3.98) | 18,649 (3.98) | 16,145 (3.89) | 53,190 (3.95) | 0.058 |
| Dizziness and giddiness, % | 9,570 (2.07) | 9,613 (2.05) | 7,892 (1.9) | 27,075 (2.01) | <0.001 |
| Epidemic vertigo, % | 270 (0.06) | 121 (0.03) | 47 (0.01) | 438 (0.03) | <0.001 |
| Ménière’s disease, % | 749 (0.16) | 704 (0.15) | 596 (0.14) | 2,049 (0.15) | 0.083 |
| Benign paroxysmal vertigo, % | 1,354 (0.29) | 1,455 (0.31) | 1,442 (0.35) | 4,251 (0.32) | <0.001 |
| Vestibular neuronitis, % | 92 (0.02) | 119 (0.03) | 130 (0.03) | 341 (0.03) | 0.003 |
| Other peripheral vertigo, % | 2,949 (0.64) | 3,177 (0.68) | 2,890 (0.7) | 9,016 (0.67) | 0.002 |
| Vertigo of central origin, % | 510 (0.11) | 475 (0.1) | 450 (0.11) | 1,435 (0.11) | 0.384 |
| Other disorders of vestibular function, % | 32 (0.01) | 52 (0.01) | 54 (0.01) | 138 (0.01) | 0.015 |
| Disorders of vestibular function, unspecified, % | 2,787 (0.6) | 2,881 (0.61) | 2,483 (0.6) | 8,151 (0.61) | 0.579 |
| Vertiginous syndromes in diseases | 83 (0.02) | 52 (0.01) | 161 (0.04) | 296 (0.02) | <0.001 |
| classified elsewhere, % |
Children, 0– 14 years; Adults, 15– 64 years; Elderly patients, 3 65 years. Infant, 0 years; Toddler, 1– 4 years; Childhood, 5– 9 years; Adolescent, 10– 14 years. Determined by the χ2 test for categorical variables and Kruskal-Wallis test for continuous variables. Abbreviation: IQR, interquartile range.
3.2Admission results
Supplemental Table 1 also shows the disposition in the ED, comparing sex differences. A total of 11,862 patients (4,323 males, 7,539 females) were admitted to the hospital to which they were transported, representing 22.3% (11,862/53,190) of patients with dizziness. A total of 41,109 patients (15,426 males, 25,683 females) were discharged home. The prevalence of admission from the ED did not differ significantly between the 3 years studied (Supplemental Table 6). Three patients with dizziness and giddiness or epidemic vertigo died in the ED. Of these, one male patient with dizziness and giddiness died in the ED. Supplemental Table 2 shows the hospital course for 21 days after transportation. Most patients could go back home within 21 days (4,009 males, 7,059 females). Thirteen patients (9 males, 4 females) died within 21 days of admission and the mortality rate was 0.003%. The final diagnoses of the 13 deceased patients per ICD-10 code were as followed: 3 same diagnoses, 2 heart failure, 2 cerebral infarction, 1 malignant neoplasm of breast, 1 acute myocardial infarction, 1 bacterial meningitis, 1acute respiratory failure, 1 adult T-cell lymphoma, and 1 cirrhosis of liver.
3.3Final diagnoses analysis
The OR of admission for emergency dizziness was 0.98 in 2020 with reference to 2018 (95% CI 0.93– 1.03) and was not significant (Table 2). With reference to males, the OR for female emergency admission was not significant (adjusted OR 1.00, 95% CI 0.96– 1.05) (Table 2). With reference to dizziness and giddiness, all dizziness diseases except epidemic vertigo (A88.1) were significantly higher for admission to the ED in patients with dizziness (Table 2). The highest OR was seen for emergency admission of vestibular neuronitis (adjusted OR 21.43, 95% CI 16.54– 27.76), followed by vertigo of central origin (adjusted OR 4.70, 95% CI 4.21– 5.25) in dizziness. Nighttime was significantly higher for admission to the ED in patients with dizziness (adjusted OR 1.05, 95% CI 1.00– 1.09, P = 0.038), but weekend was significantly negative for admission of patients with dizziness to the ED (adjusted OR 0.91, 95% CI 0.91– 1.00, P = 0.045). Vital signs of patients who needed admission from the ED differed significantly from those of patients who were not admitted to the hospital from the ED (Supplemental Table 4 and Supplemental Figure 1).
Table 2
Multivariate logistic regression analysis of the disposition at the ED in patients with dizziness
| Emergency admission | Odds ratio | 95% confidence interval | P value | ||
| Year | |||||
| 2018 | Reference | ||||
| 2019 | 0.98 | 0.93 | – | 1.03 | 0.333 |
| 2020 | 0.98 | 0.93 | – | 1.03 | 0.406 |
| Female (compared with male) | 1.00 | 0.96 | – | 1.05 | 0.866 |
| Dizziness and giddiness | Reference | ||||
| Epidemic vertigo | 1.13 | 0.88 | – | 1.46 | 0.34 |
| Ménière’s disease | 2.99 | 2.71 | – | 3.30 | <0.001 |
| Benign paroxysmal vertigo | 3.81 | 3.55 | – | 4.09 | <0.001 |
| Vestibular neuronitis | 21.43 | 16.54 | – | 27.76 | <0.001 |
| Other peripheral vertigo | 2.63 | 2.49 | – | 2.78 | <0.001 |
| Vertigo of central origin | 4.70 | 4.21 | – | 5.25 | <0.001 |
| Other disorders of vestibular function | 4.69 | 3.33 | – | 6.60 | <0.001 |
| Disorders of vestibular function, unspecified | 1.29 | 1.21 | – | 1.38 | <0.001 |
| Vertiginous syndromes in diseases classified elsewhere | 3.18 | 2.49 | – | 4.06 | <0.001 |
| Nighttime (17 : 00– 09 : 00) (compared with daytime) | 1.05 | 1.00 | – | 1.09 | 0.038 |
| Weekends (compared with weekdays) | 0.95 | 0.91 | – | 1.00 | 0.045 |
| Age (per 10 years) | 1.21 | 1.20 | – | 1.23 | <0.001 |
| Discharged to home | Odds ratio | 95% confidence interval | P value | ||
| Year | |||||
| 2018 | Reference | ||||
| 2019 | 1.01 | 0.96 | – | 1.07 | 0.576 |
| 2020 | 1.00 | 0.95 | – | 1.05 | 0.944 |
| Female (compared with male) | 1.00 | 0.96 | – | 1.05 | 0.983 |
| Dizziness and giddiness | Reference | ||||
| Epidemic vertigo | 0.84 | 0.65 | – | 1.07 | 0.161 |
| Ménière’s disease | 0.34 | 0.31 | – | 0.37 | <0.001 |
| Benign paroxysmal vertigo | 0.27 | 0.25 | – | 0.29 | <0.001 |
| Vestibular neuronitis | 0.05 | 0.04 | – | 0.06 | <0.001 |
| Other peripheral vertigo | 0.39 | 0.37 | – | 0.41 | <0.001 |
| Vertigo of central origin | 0.22 | 0.19 | – | 0.24 | <0.001 |
| Other disorders of vestibular function | 0.22 | 0.16 | – | 0.31 | <0.001 |
| Disorders of vestibular function, unspecified | 0.77 | 0.72 | – | 0.83 | <0.001 |
| Vertiginous syndromes in diseases classified elsewhere | 0.32 | 0.25 | – | 0.41 | <0.001 |
| Night-time (17 : 00– 09 : 00) (compared with daytime) | 0.97 | 0.93 | – | 1.01 | 0.174 |
| Weekends (compared with weekdays) | 1.06 | 1.01 | – | 1.11 | 0.014 |
| Age (per 10 years) | 0.82 | 0.81 | – | 0.83 | <0.001 |
4Discussion
This study appears to be the first study to clarify the epidemiology of emergency dizziness using EMS data in Japan. The total number of patients with dizziness who were transported to hospitals by ambulance in Osaka Prefecture was 53,190 (18,396 in 2018, 18,649 in 2019, and 16,145 in 2020; P = 0.058). This accounted for approximately 4% of ED transportations and 22.3% of these patients required hospital admission, similar to previous studies, with or without the COVID-19 pandemic [6, 7, 12, 16]. The COVID-19 pandemic in 2020 was associated with an increased OR for emergency admission in all transported patients, but did not exert a significant influence on emergency admissions among patients with dizziness.
Vestibular neuronitis shows no sex preference and usually affects individuals at 30– 50 years old, and is caused by inflammation of the vestibular portion of the eighth cranial nerve [1, 14]. Vestibular neuronitis showed the highest OR for emergency admission with reference to dizziness and giddiness in our study, usually accompanied by nausea and gait imbalance lasting more than 24 h [1, 14]. The prevalence of vertigo of central origin was approximately 6% among patients with dizziness to the ED [6, 15]. However, in our study, this prevalence was only 2.7% among patients with dizziness to the ED (Table 1), compared to 5.4% among patients needing admission (Supplemental Table 1). Dizziness due to the central origin includes central etiologies such as vestibular migraine and impending cerebrovascular event of vertebrobasilar ischemia [14]. Why vestibular neuronitis had a higher OR for emergency admission than vertigo of central origin in our study remains unclear. One reason may be that dizziness caused by stroke events was excluded from this study, because stroke used another ICD-10 code (not H81.4) and 28– 59% of central etiologies were misdiagnosed in the ED [7].
Three patients (1 male, 2 females) with dizziness died in the ED (Supplemental Table 1) and 13 patients (9 males, 4 females) died within 21 days of admission (Supplemental Table 2), and the causes of death were not recorded in the ORION system, however we were able to obtain the final diagnosis by ICD-10 codes as to the cause of death of the patients who died during their admission (3 same diagnoses, 2 heart failure, 2 cerebral infarction, 1 malignant neoplasm of breast, 1 acute myocardial infarction, 1 bacterial meningitis, 1acute respiratory failure, 1 adult T-cell lymphoma, and 1 cirrhosis of liver). Two patients were died of cerebral infarction, but their diagnoses at the ED were dizziness and giddiness, not vertigo of central origin. They might have stroke irrespective of dizziness; however, we could not know the details of the hospital course. One patient with epidemic vertigo died in the ED. Epidemic vertigo is a monophasic episode of paroxysmal attack of vertigo, not accompanied by cochlear symptoms, often following a non-specific upper respiratory infection, and difficult to differentiate from vestibular neuronitis. Some of these cases might have further attacks of vertigo beyond the specific period of follow up. It is unclear as to the reason why the physician coded this patient “epidemic vertigo”.
A previous retrospective cohort study of 1,931 patients with dizziness reported an overall 5-year mortality rate of 4.3%, comparable with that in the general population [3]. The mortality rate in the present study was only 0.03% for 21 days, which might approximate to 2.6% for 5 years if calculated simply. One reason for this low mortality rate might be the use of mismatched ICD-10 codes such as stroke and other serious diseases with dizziness.
COVID-19 is caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was identified in China in December 2019, and the COVID-19 outbreak spread rapidly around the world [24]. The COVID-19 pandemic in 2020 decreased the number of both general patients and patients with dizziness (Table 1), with similar prevalence to other years (3.98% in 2018, 3.98% in 2019, and 3.89% in 2020; P = 0.058). This may mean that individuals may have refrained from unnecessary EMS transports during the COVID-19 pandemic in 2020. A previous study from a university hospital in Japan showed numerous cancellations for medical examinations in patients with dizziness among ear, nose, and throat (ENT) outpatients during the COVID-19 outbreak [22]. Both the absolute number and prevalence of dizziness/giddiness (R42) and epidemic vertigo (A88.1) were decreased in 2020 in our study, but young patients < 50 years old with benign paroxysmal vertigo and vestibular neuronitis increased in 2020, and this finding was also reported in China [11]. The authors reported special stress as a triggering factor for benign paroxysmal vertigo, likely caused by the COVID-19 pandemic [11]. Sleep disturbance attributed to night duties has been associated with increased risk of benign paroxysmal vertigo in healthy physicians and nurses under the age of 60 [2]. Oxidative stress can play a role in the pathogenesis of benign paroxysmal vertigo [5, 9]. Psychological stress increases oxidative stress, hence, special psychological stress due to COVID-19 outbreak could produce endolymphatic free-floating debris [5, 21]. Several studies had reported the association between psychological stress and vestibular neuronitis [4, 10].
This study shows several limitations. First, this was a retrospective, observational study, and some unknown confounding factors may have been included due to this study type. However, our results were in line with findings from previous studies. Second, adjustment for various factors such as medical history, medications, and health status could not be performed in the logistic regression analysis, because this information was unavailable. Third, the COVID-19 outbreak started in April 2020 in Japan, so we might have underestimated the influence of COVID-19, although a previous study showed the influences of COVID-19 on the EMS system in Japan for the same study period [18, 19]. Finally, details of the hospital course as well as test results in the ED were unavailable, so we did not have access to the results of neurological examinations and imaging findings, or to exact causes of death.
5Conclusions
The results of this study showed that patients with dizziness accounted for approximately 4% of ED transportations and about 20% of them required hospital admission, irrespective of the COVID-19 outbreak. However, the absolute number of patients with dizziness decreased significantly. The OR for an emergency admission for vestibular neuronitis was the highest, followed by vertigo of central origin. Further research is needed to investigate the tendency of younger patients with increased incidence of benign paroxysmal vertigo and vestibular neuronitis during the COVID-19 pandemic.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
K.O. designed the study and wrote the initial draft of the manuscript. Ka.O., D.N., T.K., Y.K., M.N., T.M., and A.T. contributed to analysis and interpretation of the data and assisted in the preparation of the manuscript. All authors contributed to data collection and interpretation and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work, including ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ICMJE statement
All authors meet the ICMJE authorship criteria.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
We have no conflicts of interest to disclose.
Ethics approval
This study was approved by the Ethics Committee of Osaka Medical and Pharmaceutical University (Takatsuki City, Japan).
Consent to participate
Informed consent from the participants was waived because the data were anonymous.
Acknowledgments
The authors thank the EMS providers, nurses, emergency physicians and administrators for their cooperation in the ORION. We thank all the members of The Working Group to Analyze the Emergency Medical Care System in Osaka Prefecture for their kind support.
Supplementary material
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/VES-220024.
References
[1] | Bae C.H. , Na H.G. and Choi Y.S. , Update on current diagnosis and treatment of vestibular neuritis, Yeungnam Univ J Med (2021), 1–8. |
[2] | Bashir K. , Elsotohy H.H. and Elmoheen A. , Do night shifts increase the risk of benign paroxysmal positional vertigo among doctors and nurses? J Multidiscip Healthc 13: ((2020) ), 963–966. |
[3] | Berge J.E. , Nordahl S.H.G. , Aarstad H.J. and Goplen F.K. , Long-Term Survival in 1,931 Patients With Dizziness: Disease- and Symptom-Specific Mortality, Laryngoscope 131: ((2021) ), E2031–E2037. |
[4] | Best C. , Tschan R. , Eckhardt-Henn A. and Dieterich M. , Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience 164: ((2009) ), 1579–1587. |
[5] | Chen X. , Feng H. , Liu H. , Xu X. , Wang J. and Jin Z. , Carotid imaging changes and serum IL-1β, sICAM-1, and sVAP-1 levels in benign paroxysmal positional vertigo, Sci Rep 10: ((2020) ), 1–6. |
[6] | Cheung C.S.K. , Mak P.S.K. , Manley K. V. , Lam J.M.Y. , Tsang A.Y.L. , Chan H.M.S. , Rainer T.H. and Graham C.A. , Predictors of important neurological causes of dizziness among patients presenting to the emergency department, Emerg Med J 27: ((2010) ), 517–521. |
[7] | Edlow J.A. , Diagnosing Patients With Acute-Onset Persistent Dizziness, Ann Emerg Med 71: ((2018) ), 625–631. |
[8] | von Elm E. , Altman D.G. , Egger M. , Pocock S.J. , Gøtzsche P.C. and Vandenbroucke J.P. , The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies, Int J Surg 12: ((2014) ), 1495–1499. |
[9] | Güçlütürk M.T. , Ünal Z.N. , Ismi O. , Çimen M.B.Y. and Ünal M. , The role of oxidative stress and inflammatory mediators in benign paroxysmal positional vertigo, J Int Adv Otol 12: ((2016) ), 101–105. |
[10] | Hong S.M. , Lee H.J. , Lee B. , Park S.K. , Hong S.K. , Park I.S. , Kim Y.B. and Kim H.J. , Influence of vestibular disease on psychological distress: A multicenter study, Otolaryngol – Head Neck Surg (United States) 148: ((2013) ), 810–814. |
[11] | Li C. , Guo D. , Ma X. , Liu S. , Liu M. and Zhou L. , The Impact of Coronavirus Disease Epidemic on Dizziness/Vertigo Outpatients in a Neurological Clinic in China, Front Neurol 12: ((2021) ), 663173–. |
[12] | Ljunggren M. , Persson J. and Salzer J. , Dizziness and the Acute Vestibular Syndrome at the Emergency Department: A Population-Based Descriptive Study, Eur Neurol 79: ((2018) ), 5–12. |
[13] | Mizukoshi K. , Watanabe Y. , Shojaku H. , Okubo J. and Watanabe I. , Epidemiological studies on benign paroxysmal positional vertigo in Japan., Acta Otolaryngol Suppl 447: ((1988) ), 67–72. |
[14] | Muncie H.L. , Sirmans S.M. and James E. , Dizziness: Approach to evaluation and management, Am Fam Physician 95: ((2017) ), 154–162. |
[15] | Neuhauser H.K. , The epidemiology of dizziness and vertigo, 1st ed., Elsevier B.V., (2016) . |
[16] | Newman-Toker D.E. , Hsieh Y.H. , Camargo C.A. , Pelletier A.J. , Butchy G.T. and Edlow J.A. , Spectrum of dizziness visits to US emergency departments: Cross-sectional analysis from a nationally representative sample, Mayo Clin Proc 83: ((2008) ), 765–775. |
[17] | Okamoto J. , Katayama Y. , Kitamura T. , Sado J. , Nakamura R. , Kimura N. , Misaki H. , Yamao S. , Nakao S. , Nitta M. , Iwami T. , Fujimi S. , Kuwagata Y. , Shimazu T. and Matsuoka T. , Profile of the ORION (Osaka emergency information Research Intelligent Operation Network system) between and in Osaka, Japan: a population-based registry of emergency patients with both ambulance and in-hospital records, Acute Med Surg 6: ((2019) ), 12–24. |
[18] | Ota K. , Nishioka D. , Katayama Y. , Kitamura T. , Masui J. , Ota K. , Nitta M. , Matsuoka T. and Takasu A. , Influence of the -19 outbreak on transportation of pregnant women in an emergency medical service system: Population-based, ORION registry., Int J Gynaecol Obstet (2022). |
[19] | Ota K. , Nishioka D. , Katayama Y. , Kitamura T. , Masui J. , Ota K. , Nitta M. , Matsuoka T. and Takasu A. , Effect of the COVID-19 outbreak on emergency transport of children by an emergency medical service system: a population-based, ORION registry study., BMC Emerg Med 22: ((2022) ), 206. |
[20] | Saber Tehrani A.S. , Coughlan D , Hsieh Y.H. , Mantokoudis G. , Korley F.K. , Kerber K.A. , Frick K.D. and Newman-Toker D.E. , Rising annual costs of dizziness presentations to U.S. emergency departments, Acad Emerg Med 20: ((2013) ), 689–696. |
[21] | Sivonová M. , Žitňanová I. , Hlinčíková L. , Škodáček I. , Trebatická J. and Ďuračcaron;ková Z. , Oxidative stress inuniversity students during examinations, Stress 7: ((2004) ), 183–188. |
[22] | Ueda K. , Ota I. , Yamanaka T. and Kitahara T. , The Impact of the COVID-19 Pandemic on Follow-Ups for Vertigo/Dizziness Outpatients, Ear, Nose Throat J 100: ((2021) ), 163S–168S. |
[23] | WHO, International Statistical Classification of Diseases and Related Health Problems, 10th Revision ICD-10: Tabular List, World Heal Organ 1: ((2016) ), 332–345. |
[24] | Wiersinga W.J. , Rhodes A. , Cheng A.C. , Peacock S.J. and Prescott H.C. , Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease (COVID-19): A Review, JAMA – J Am Med Assoc 324: ((2020) ), 782–793. |



