Association of Vitamin D levels on the Clinical Outcomes of Patients Hospitalized for COVID-19 in a Tertiary Hospital
DOI:
https://doi.org/10.15605/jafes.038.01.07Keywords:
Vitamin D, Vitamin D deficiency, COVID-19Abstract
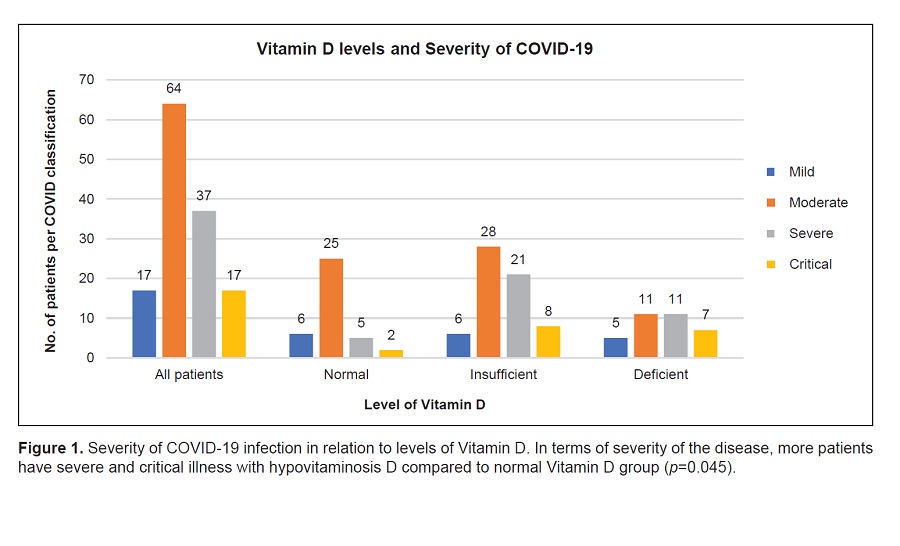
Objectives. This study aimed to compare the severity of COVID-19, inflammatory parameters and clinical outcomes among patients with normal and subnormal levels of Vitamin D.
Methodology. This is a retrospective cohort study of 135 patients admitted in a tertiary hospital for COVID-19. Patients were grouped according to their Vitamin D level. Primary outcome measure was the composite of all-cause mortality and morbidity. Other outcome measures determined were the comparison among the groups on the severity of COVID-19 infection, changes in inflammatory parameters, length of hospital stay and duration of respiratory support.
Results. There was a significant trend of higher ICU admission (p=0.024), mortality (p=0.006) and poor clinical outcome (p=0.009) among the Vitamin D deficient group. No significant difference was found for most of the inflammatory parameters, duration of hospital stay and respiratory support. Overall, patients with deficient, but not insufficient Vitamin D level had 6 times higher odds of composite poor outcome than those with normal Vitamin D (crude OR=5.18, p=0.003; adjusted OR=6.3, p=0.043).
Conclusion. The inverse relationship between Vitamin D level and poor composite outcome observed in our study suggests that low Vitamin D may be a risk factor for poor prognosis among patients admitted for COVID-19.
Downloads
References
Holick MF. The Vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18(2):153-65. https://pubmed.ncbi.nlm.nih.gov/28516265. https://doi.org/10.1007/s11154-017-9424-1.
Angeles-Agdeppa I, Perlas LA, Capanzana M. Vitamin D status of Filipino adults: Evidence from the 8th National Nutrition Survey 2013. Malays J Nutr. 2018; 24(3):395-406.
Sung CC, Liao MT, Lu KC, Wu CC. Role of Vitamin D in insulin resistance. J Biomed Biotechnol. 2012;2012:634195. https://pubmed.ncbi.nlm.nih.gov/22988423. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3440067. https://doi.org/10.1155/2012/634195.
Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881-6. https://pubmed.ncbi.nlm.nih.gov/21527855. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166406. https://doi.org/10.2310/JIM.0b013e31821b8755.
Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of Vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep. 2020;10(1):20191. https://pubmed.ncbi.nlm.nih.gov/33214648. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7677378. https://doi.org/10.1038/s41598-020-77093-z.
Ali N. Role of Vitamin D in preventing of COVID-19 infection, progression and severity. J Infect Public Health. 2020;13(10):1373-80. https://pubmed.ncbi.nlm.nih.gov/32605780. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7305922. https://doi.org/10.1016/j.jiph.2020.06.021.
Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988. https://pubmed.ncbi.nlm.nih.gov/32252338. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7231123. https://doi.org/10.3390/nu12040988.
Peng MY, Liu WC, Zheng JQ, et al. Immunological aspects of SARS-CoV-2 infection and the putative beneficial role of Vitamin-D. Int J Mol Sci. 2021;22(10):5251. https://pubmed.ncbi.nlm.nih.gov/34065735. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8155889. https://doi.org/10.3390/ijms22105251.
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of Vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30. Erratum in: J Clin Endocrinol Metab. 2011;96(12):3908. https://pubmed.ncbi.nlm.nih.gov/21646368.
https://doi.org/10.1210/jc.2011-0385.
World Health Organization. Clinical management of COVID-19 Interim Guidance; 2020. https://apps.who.int/iris/handle/10665/332196.
Demir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID- 19 positivity and severity of the disease. J Med Virol. 2021;93(5):2992-9. https://pubmed.ncbi.nlm.nih.gov/33512007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8013436. https://doi.org/10.1002/jmv.26832.
Greenland S, Pearce N. Statistical foundations for model-based adjustments. Annu Rev Public Health. 2015;36:89-108. https://pubmed.ncbi.nlm.nih.gov/25785886. https://doi.org/10.1146/annurev-publhealth-031914-122559.
Palomer X, González-Clemente JM, Blanco-Vaca F, Mauricio D. Role of Vitamin D in the pathogenesis of type 2 diabetes mellitus. Diabetes Obes Metab. 2008;10(3):185-97. https://pubmed.ncbi.nlm.nih.gov/18269634. https://doi.org/10.1111/j.1463-1326.2007.00710.x.
Vranić L, Mikolašević I, Milić S. Vitamin D deficiency: Consequence or cause of obesity? Medicina (Kaunas). 2019;55(9):541. https://pubmed.ncbi.nlm.nih.gov/31466220. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6780345. https://doi.org/10.3390/medicina55090541.
Agarwal M, Phan A, Willix R Jr, Barber M, Schwarz ER. Is Vitamin D deficiency associated with heart failure? A review of current evidence. J Cardiovasc Pharmacol Ther. 2011;16(3-4):354-63. https://pubmed.ncbi.nlm.nih.gov/21304056. https://doi.org/10.1177/1074248410390214.
Campi I, Gennari L, Merlotti D, et al. Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy. BMC Infect Dis. 2021;21(1):566. https://pubmed.ncbi.nlm.nih.gov/34126960. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8200788. https://doi.org/10.1186/s12879-021-06281-7.
Pereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida Oliveira T, da Mota Santana J. Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2022;62(5):1308-16. https://pubmed.ncbi.nlm.nih.gov/33146028. https://doi.org/10.1080/10408398.2020.1841090.
Fatemi A, Ardehali SH, Eslamian G, Noormohammadi M, Malek S. Association of Vitamin D deficiency with COVID-19 severity and mortality in Iranian people: A prospective observational study. Acute Crit Care. 2021;36(4):300-7. https://pubmed.ncbi.nlm.nih.gov/35263825. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8907463. https://doi.org/10.4266/acc.2021.00605.
Samprathi M, Jayashree M. Biomarkers in COVID-19: An Up-To-Date review. Front Pediatr. 2021;8:607647. https://pubmed.ncbi.nlm.nih.gov/33859967. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8042162. https://doi.org/10.3389/fped.2020.607647.
Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. Evidence for possible association of Vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients. Aging Clin Exp Res.2020;32(10):2141-58. https://pubmed.ncbi.nlm.nih.gov/32876941. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7465887. https://doi.org/10.1007/s40520-020-01677-y
Yao Y, Cao J, Wang Q, et al. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: A case control study. J Intensive Care. 2020;8:49. https://pubmed.ncbi.nlm.nih.gov/32665858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7348129. https://doi.org/10.1186/s40560-020-00466-z.
Teama MAEM, Abdelhakam DA, Elmohamadi MA, Badr FM. Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection. Sci Prog. 2021;104(3):368504211036854. https://pubmed.ncbi.nlm.nih.gov/34347528. https://doi.org/10.1177/00368504211036854.
Sengupta T, Majumder R, Majumder S. Role of Vitamin D in treating COVID-19-associated coagulopathy: Problems and perspectives. Mol Cell Biochem. 2021;476(6):2421-7. https://pubmed.ncbi.nlm.nih.gov/33604809. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7891480. https://doi.org/10.1007/s11010-021-04093-6.
Li Y, Hu Y, Yu J, Ma T. Retrospective analysis of laboratory testing in 54 patients with severe- or critical-type 2019 novel coronavirus pneumonia. Lab Invest. 2020;100(6):794-800. https://pubmed.ncbi.nlm.nih.gov/32341519. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184820. https://doi.org/10.1038/s41374-020-0431-6.
Driggin E, Madhavan MV, Gupta A. The role of Vitamin D in cardiovascular disease and COVID-19. Rev Endocr Metab Disord. 2022;23(2):293-7. https://pubmed.ncbi.nlm.nih.gov/35233703. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8888268. https://doi.org/10.1007/s11154-021-09674-w.
Ilie PC, Stefanescu S, Smith L. The role of Vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020;32(7):1195-8. https://pubmed.ncbi.nlm.nih.gov/32377965. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202265. https://doi.org/10.1007/s40520-020-01570-8.
Reis BZ, Fernandes AL, Sales LP, et al. Influence of Vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: A multicenter prospective cohort study. Am J Clin Nutr. 2021;114(2):598-604. https://pubmed.ncbi.nlm.nih.gov/34020451. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8194634. https://doi.org/10.1093/ajcn/nqab151.
Orchard L, Baldry M, Nasim-Mohi M, et al. Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients. Clin Chem Lab Med. 2021;19;59(6):1155-63. https://pubmed.ncbi.nlm.nih.gov/33554566. https://doi.org/10.1515/cclm-2020-1567.
Pecina JL, Merry SP, Park JG, Thacher TD. Vitamin D status and severe COVID-19 disease outcomes in hospitalized patients. J Prim Care Community Health. 2021;12:21501327211041206. https://pubmed.ncbi.nlm.nih.gov/34452582. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8404616. https://doi.org/10.1177/21501327211041206.
Infante M, Buoso A, Pieri M, et al. Low Vitamin D status at admission as a risk factor for poor survival in hospitalized patients with COVID-19: An Italian
retrospective study. J Am Nutr Assoc. 2022;41(3):250-65. https://pubmed.ncbi.nlm.nih.gov/33600292.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7899172. https://doi.org/10.1080/07315724.2021.1877580.
Jolliffe DA, Holt H, Greenig M, et al. Effect of a test-and-treat approach to Vitamin D supplementation on risk of all cause acute respiratory tract infection and COVID-19: Phase 3 randomised controlled trial (CORONAVIT). BMJ. 2022;378:e071230. https://pubmed.ncbi.nlm.nih.gov/36215226. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9449358. https://doi.org/10.1136/bmj-2022-071230.
Syquio MVA, Genuino RNF, Tolosa MTS. Should Vitamin D supplements be used as adjunct treatment for COVID-19? Philippine COVID-19 Living Clinical Practice Guidelines. February 20, 2021. https://www.psmid.org/wp-content/uploads/2021/05/ADJUNCT_Vitamin-D_FINAL.pdf.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Margarita Katrina Amor Tan, Rebecca Alba, Kingbherly Li

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















