Key summary points
To identify the impact of COVID-19 on case-mix, care standards and outcomes of hip fracture patients in Ireland for the first 6 months of the COVID-19 pandemic.
AbstractSection FindingsThere was a 15% reduction in admissions per month during the first 6 months of the COVID-19 pandemic. There was a reduction in compliance with many of the Irish Hip Fracture Standards following the COVID-19 pandemic.
AbstractSection MessageEvery attempt should be made to preserve the multidisciplinary team involved in the care pathway for hip fracture patients throughout any subsequent waves of the COVID-19 pandemic.
Abstract
Purpose
To describe the impact of COVID-19 on hip fracture care during the first 6 months of the pandemic.
Methods
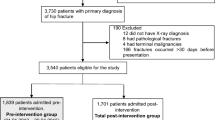
A secondary analysis of 4385 cases in the Irish Hip Fracture Database from 1st June 2019 to 31st August 2020 was conducted.
Results
Hip fracture admissions decreased by 15% during the study period (p < 0.001). Patient characteristics were largely unchanged as the majority of cases occurred in females over 80 years admitted from home. Adherence to many of the Irish Hip Fracture Standards (IHFS) changed following the COVID-19 pandemic. There was an increase in patients admitted to an orthopaedic ward from Emergency Department (ED) within 4 h from 27 to 36% (p < 0.001). However, the proportion of patients reviewed by a geriatrician reduced from 85% pre-COVID to 80% (p < 0.001). Fewer patients received a bone health assessment [90% from 95% (p < 0.001)] and specialist falls assessment [(82% from 88% (p < 0.001)]. No change was seen in time to surgery or incidence of pressure injuries. There was a significant decrease in length of stay from 18 to 14 days (p < 0.001). There was an increase in patients discharged home during the COVID-19 period and a decrease in patients discharged to rehabilitation, convalescence or nursing home care. There was no statistically significant change in mortality.
Conclusion
Healthcare services were widely restructured during the pandemic, which had implications for hip fracture patients. There was a notable change in compliance with the IHFS. Multidisciplinary teams involved in hip fracture care should be preserved throughout any subsequent waves of the pandemic.
Similar content being viewed by others
Introduction
In December 2019, a novel strain of coronavirus disease commonly known as COVID-19 was identified in the city of Wuhan in the Hubei province of China. Since then, the SARS (Severe Acute Respiratory Syndrome)-CoV-2 virus has spread globally and continues to cause huge disruption to healthcare services, societal life and the economy. The first confirmed case in Ireland was identified on the 29th February 2020, and on the 11th March 2020, COVID-19 was declared a pandemic by the World Health Organization [1]. Subsequently, the National Public Health Emergency Team (NPHET) for COVID-19 was established to coordinate the Irish response to the pandemic.
The care pathway for hip fracture patients is complex and requires a multidisciplinary approach. The management of hip fractures is often used as a surrogate marker for the care of older patients in acute hospitals and is an indicator of how well the trauma service is functioning [2]. However, during the pandemic, there was widespread staff redeployment and service reconfiguration, which had implications for the management of hip fracture patients [3]. During this period, healthcare systems were under considerable pressure, grappling with the management of a new infectious disease and rising case numbers. In parallel, patients with trauma and other illnesses continued to present to the acute hospitals, albeit at a reduced level. Data from the Irish Hip Fracture Database (IHFD) showed a reduction in the number of hip fracture presentations during the first 6 months of the pandemic and this will be explored in this paper. A reduction was also observed in Spain where a 25% decrease was noted [4]. Conversely, in the UK, reduction in hip fracture incidence was not observed [5]. As the pandemic rages on, there is a growing need to understand the implications of such significant disruptions to the healthcare system so that steps can be taken to preserve vital services across the acute hospital, rehabilitation and community sectors.
This paper describes the first 6 months of the COVID-19 impact on the incidence, care standards and outcomes of hip fracture patients in Ireland compared to data from the previous 9 months.
Irish Hip Fracture Database
The Irish Hip Fracture Database (IHFD) is a national clinical audit that was established in 2012 to improve the care and outcomes of hip fracture patients in Ireland. It is a clinically led, web-based system where data are collected though the Hospital In-Patient Enquiry (HIPE) portal, in association with the Healthcare Pricing Office (HPO). It is clinically supported by the Irish Institute of Trauma and Orthopaedic Surgery (IITOS) and the Irish Gerontological Society (IGS). Operational management is provided by the National Office for Clinical Audit (NOCA). Each of the 16 operating public hospitals submits data to the IHFD with 99% data coverage [2]. The IHFD focuses on seven clinical standards of care known as the Irish Hip Fracture Standards (IHFS) (Fig. 1). The authors will describe the impact of COVID-19 on adherence to each of the IHFS.
Methods
A secondary analysis of 4,385 cases in the Irish Hip Fracture Database admitted from 1st June 2019 to 31st August 2020 was conducted. For the purpose of this analysis, the authors defined the pre-COVID-19 period as 1st June 2019 to 29th February 2020 and the COVID-19 pandemic from 1st March 2020 to 31st August 2020. The analysis is based on data from the IHFD as captured by HIPE, with the following inclusion and exclusion criteria:
Inclusion criteria
- (i):
-
Patients admitted between 1 June 2019 and 31st August 2020 inclusive;
- (ii):
-
Patients diagnosed on HIPE with either a hip fracture due to injury or with a specified type of fracture, other than periprosthetic;
- (iii):
-
Patients aged 60 years or over.
Exclusion criteria
(i) Patients aged 59 years or younger;
The analysis focussed on identifying differences between the pre-COVID-19 period and the period of the COVID-19 pandemic in terms of monthly number of admissions, case-mix of admitted patients, standards of care and outcomes. Data analysis was conducted using STATA Version 15 and SPSS. Chi-squared statistical tests (for binary and categorical variables) and t-tests (for continuous variables) were used to determine whether there was a statistical difference between the pre-COVID-19 and the period of the COVID-19 pandemic for key outcome and process variables. A p value of less than or equal to 0.05 indicated statistical significance.
Results
Demographics
Overall, there was no statistically significant difference in the sex (p = 0.492) or age (p = 0.408) of hip fracture patients (pre-COVID-19 period and COVID-19 period). The mean age of patients with hip fracture was 85 years. Sixty-eight percent of patients with hip fracture were female and 58% were aged 80 years or more during both time periods. The American Society of Anaesthesiologists (ASA) physical status classification which is used to assess a patient’s pre-anaesthesia medical comorbidities showed that there was no statistically significant difference in ASA grades [6]. A higher proportion of patients were recorded with a low level of functional mobility (54%) in the COVID-19 period relative to the pre-COVID-19 period (50%), and this was statistically significantly (p = 0.019).
Admissions
There was a 15% reduction in admissions per month (p < 0.001) during the first 6 months of the COVID-19 pandemic (Fig. 2).
Relative to the pre-COVID-19 period, there was a statistically significant increase in admissions from nursing homes during COVID-19 (p < 0.001). Furthermore, the number of home admissions was statistically significantly lower during COVID-19 (p < 0.001) (Table 1).
Irish Hip fracture standards and best practice tariff
There was a change in adherence to some of the IHFS during the COVID-19 period, as outlined in Table 2. There was an increase in the proportion of patients who were admitted to an orthopaedic ward from ED within 4 h (IHFS 1) from 27 to 36% (p < 0.001) during the COVID-19 period. No change was observed in relation to time to surgery within 48 h (IHFS 2), which remained at 75%. Similarly, no change was see in the incidence of pressure injuries (IHFS 3), which remained at 3%. There was a significant decrease in compliance with the remaining standards. The proportion of patients reviewed by a geriatrician (IHFS 4) decreased to 80% in the COVID-19 period from 85% (p < 0.001), the proportion of patients receiving a bone health assessment (IHFS 5) reduced to 90% from 95% (p < 0.001). A specialist falls assessment (IHFS 6) was carried out on 82% of patients as opposed to 88% pre-COVID-19 (p < 0.001). A reduction in compliance was noted in the proportion of patients mobilised early by a physiotherapist (IHFS 7) from 78 to 75%, however, this finding was not statistically significant.
Since 2018, the IHFS are linked to a best practice tariff (BPT). The BPT system rewards hospitals that provide high quality patient care, i.e. for each case that meets the first six clinical standards (IHFS 1–6, Fig. 1) and two data quality standards, the hospital will receive €1000 per case. The seventh clinical standard for early mobilisation will be added to the BPT in 2021. This financial incentive is paid on a quarterly basis and is used by the hospital’s hip fracture governance committee to improve care for hip fracture patients locally. There has been a decrease in compliance with the BPT which coincides with the reduction in compliance with the IHFS during the COVID-19 pandemic.
Figure 3 shows the percentage of hip fracture patients who met each of the IHFS by month (June 2019-August 2020) and highlights the initial effect on the health system created by the COVID-19 pandemic.
Discharge destination and length of stay (LOS)
Table 3 describes the destination to which patients were discharged and LOS pre-COVID-19 versus during the COVID-19 pandemic. There was a statistically significant difference for both of these parameters (p = 0.006). There was a statistically significant increase (p < 0.001) in patients discharged home, from 30 (n = 471) in the COVID-19 period to 26% (n = 722) pre-COVID-19 (Table 3). Furthermore, the percentage of patients discharged to rehabilitation decreased from 32% (n = 887) pre-COVID-19 to 28% (n = 442) in the COVID-19 period, but this was not statistically significant. Similarly, there was a reduction in the proportion of patients discharged to convalescence and nursing home care, from 29% (n = 816) pre-COVID-19 period to 27% (n = 429) in the COVID-19 period. There was a statistically significant difference (p < 0.001) in the mean length of stay of patients admitted during the pre-COVID-19 period (18.5 days) and the mean length of stay of patients admitted during the COVID-19 period (14 days).
In-patient mortality
The percentage of in-hospital deaths in the pre-COVID-19 period was 4.9 (n = 140) and 5.2% (n = 81) during the COVID-19 period. However, this difference was not statistically significant (p = 0.804) (Table 3).
Discussion
This research highlights that despite the pandemic, hip fracture patients continued to be admitted in high volumes. This reinforces the importance of preserving care pathways associated with best practice and healthcare staff resources such as geriatricians, health and social care professionals, orthopaedic doctors and orthopaedic nurses involved in the care of older patients with hip fracture throughout the COVID-19 pandemic.
The data presented in this paper showed that there was no change in the patient demographics in the first 6 months of the COVID-19 pandemic. However, there was a change in admission source with an increase in the proportion of patients admitted from long-term care 9% to 13% (p < 0.001) owing to the fact that patients in long-term care are generally a frailer cohort. The reduction in LOS and change in discharge destination during the first 6 months needs to be further explored. During the first wave of the pandemic, many of the rehabilitation hospitals were closed to admissions which may have played a role in more patients being discharged directly home. Future research is needed to assess the consequences of the reduced length of stay or direct discharge home.
One of the most interesting findings from this research has been the impact on the Irish Hip Fracture Standards. The first standard (IHFS 1) for time of admission through the emergency department (ED) improved and continued to improve throughout the first 6-months most likely owing to the change in admission pathways in the ED due to COVID-19. Time to surgery stayed the same which has been seen in a study published from a Major Trauma Centre in Scotland which also had a significant reduction in LOS 12 days to 6.5 days (< 0.005) [10]. The pressure ulcer incidence remained the same (IHFS 3). The rest of the IHFS were negatively impacted due to COVID-19, meaning less patients were seen by a geriatrician, less received a bone health and specialist falls assessments and less were mobilised early after surgery. This may have been related to the shorter length of stay noted in this study cohort and also due to the redeployment of many key specialties during this time including geriatricians and physiotherapists. There have been many publications about the benefits of early mobilisation in hip fracture patients and as a consequence this was introduced as a new standard (IHFS 7) at the start of 2020 [10, 11].
Thus far, there has been no change to in-patient mortality rate of 5% compared to the pre-COVID levels, however, it is imperative to interpret this with caution as there were very few patients with hip fracture and a diagnosis of COVID-19 during the first 6 months (n = 45). It is anticipated that the next 6 months of data (September 2020-February 2021) from the IHFD will be able to share more detail on patients with hip fracture and a COVID-19 diagnosis as the numbers were much greater during this period.
Lessons can be learnt from the unprecedented challenge facing health services worldwide. This paper describes the pre- and post-impact from COVID-19 on admissions, case-mix, care standards and outcomes from the IHFD database. A recent publication from the National Hip Fracture Database (NHFD) in the UK describes the impact from COVID-19 on the BPT and shows strong similarities to this paper in that there were reductions in orthogeriatric review, bone health assessment and BPT [7]. It is encouraging to see a number of other publications using hip fracture database or registry data, be that from single sites such as the publication from Madrid, Spain [4] using the Spanish Hip Fracture Registry or the multicentre study from the UK [8] using NHFD data which showed no change in case-mix during the pre- and post-COVID-19 periods starting to emerge. In Scotland, the hip fracture registry ceased data collection for a period due to the disruption caused by the COVID-19 pandemic; however, an international collaboration of existing hip fracture registries and databases was developed through the IMPACT: International Multicentre Project Auditing COVID-19 in Trauma and Orthopaedics global study being led by Scotland. This project is still ongoing and presents an exciting opportunity for hip fracture registries and databases to collaborate and share learnings about the impact from COVID-19.
Limitations
This paper outlines the impact of COVID-19 on hip fracture care for the first 6 months of the pandemic. The HIPE dataset for this paper was created earlier than normal without full validation to facilitate rapid learning during this unprecedented health crisis. Second, a small number of public hip fracture patients may have been treated in private hospitals during the study period. Data for the hip fracture patients treated in private hospitals have not been included in this report as private hospitals do not routinely provide data to the IHFD or to HIPE.
Conclusion
This paper describes the impact of the first 6 months of the COVID-19 pandemic on the standards of hip fracture care in Ireland. There was a reduction in the number of hip fracture admissions by 15% during this period. The age, gender, ASA grade and baseline functional status were similar between the periods observed. There was an increase in admission from long-term care facilities. Hip fracture standards affected negatively included review by a geriatrician, secondary prevention for falls and bone health and early mobilisation. There were positive impacts also noted in terms of improved admission time to an orthopaedic ward, and time to surgery and pressure ulcer incidence remained unchanged. The notable decrease in LOS and increase in the number of patients being discharged home directly needs further evaluation to determine if this expedited discharge had any longer term impacts such as increased readmission rates. This research highlights the value of clinical audit data in-monitoring the impact on care from an unprecedented situation like the global COVID-19 pandemic.
Data availability
Data from the Irish Hip Fracture Database can be requested from the National Office of Clinical Audit, Ireland.
References
Rolling updates on coronavirus disease. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-asthey-happen
National Office of Clinical Audit, (2020) Irish Hip Fracture Database National Report 2019. Dublin: National Office of Clinical Audit. http://s3-eu-west-1.amazonaws.com/nocauploads/general/Irish_Hip_Fracture_Database_National_Report_2019_10.11.2020.pdf
National Office of Clinical Audit, 2020. IHFD COVID-19 Report Issue 1: Service impact from COVID-19: analysis based on Irish Hip Fracture Database June 2019-May 2020. [Online]. Available at: http://s3-eu-west-1.amazonaws.com/noca-uploads/general/NOCA_COVID_Report_Issue_1_IHFD_Final.pdf
Ojeda-Thies, C., Cuarental-García, J. and Ramos-Pascua, L.R., 2021. Decreased volume of hip fractures observed during COVID-19 lockdown. European Geriatric Medicine, pp.1–8. https://doi.org/10.1007/s41999-020-00447-3
National Hip Fracture Database (NHFD) 2020: National Hip Fracture Database (NHFD) Annual Report 2020. Available: https://www.nhfd.co.uk/files/2020ReportFiles/NHFD_Annual_Report_2020.pdf
Dripps R (1963) New classification of physical status. Anesthesiology 24:111. https://doi.org/10.4103/0019-5049.79879
Tyas, B., Wilkinson, M. and Singisetti, K., 2021. Effect of Covid-19 on best practice care of hip fracture patients: An analysis from the National Hip Fracture Database (NHFD). The Surgeon.
Wignall A, Giannoudis V, De C, Jimenez A, Sturdee S, Nisar S, Pandit H, Gulati A, Palan J (2021) The impact of COVID-19 on the management and outcomes of patients with proximal femoral fractures: a multi-centre study of 580 patients. J Orthop Surg Res 16(1):1–7
Hall, A.J., Clement, N.D., Farrow, L., IMPACT-Scot Study Group, MacLullich, A.M., Dall, G.F., Scott, C.E., Jenkins, P.J., White, T.O. and Duckworth, A.D (2020) IMPACT-Scot report on COVID-19 and hip fractures: a multicentre study assessing mortality, predictors of early SARS-CoV-2 infection, and the effects of social lockdown on epidemiology. Bone Jt J 102(9):1219–1228
Greensmith, T.S., Faulkner, A.C., Davies, P.S., Sinnerton, R.J., Cherry, J.V., Supparamaniam, S., MacInnes, A.G.M. and Dalgleish, S., 2021. Hip Fracture Care During 2020 COVID-19 First-Wave A Review of the Outcomes of Hip Fracture Patients at a Scottish Major Trauma Centre. The Surgeon
Sheehan KJ, Goubar A, Almilaji O, Martin FC, Potter C, Jones GD, Sackley C, Ayis S (2021) Discharge after hip fracture surgery by mobilisation timing: secondary analysis of the UK National Hip Fracture Database. Age Ageing 50(2):415–422. https://doi.org/10.1093/ageing/afaa204
Ferris H, Brent L, Coughlan T (2020) Early mobilisation reduces the risk of in-hospital mortality following hip fracture. Eur Geriatr Med 11(4):527–533. https://doi.org/10.1007/s41999-020-00317-y
Acknowledgements
The authors would like to acknowledge: all the audit coordinators and clinical leads in our trauma hospitals participating in the IHFD, Healthcare Pricing Office, Irish Hip Fracture Database Governance Committee, Irish Institute of Trauma and Orthopaedic Surgery, Irish Gerontological Society, Health Service Executive—Quality Improvement Team, and Timothy WeiSiangLai—3rd Year Medical Student, RCSI.
Funding
The Irish Hip Fracture Database is supported by the National Office of Clinical Audit, which is funded by the Quality Improvement Team of the Health Service Executive. No additional funding supported the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Availability of data and material
This study involved analysis of anonymous IHFD data which have been described in previously published reports.
Ethics approval
Formal ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brent, L., Ferris, H., Sorensen, J. et al. Impact of COVID-19 on hip fracture care in Ireland: findings from the Irish Hip Fracture Database. Eur Geriatr Med 13, 425–431 (2022). https://doi.org/10.1007/s41999-021-00600-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00600-6