Andrés Fabricio Caballero-Lozada, MD. 1 ,2,3,4,*, Alejandro Segura Ordoñez M.Sc. 2 ,5
Recibido: 24-03-2021
Aceptado: 12-04-2021
©2021 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 50 Núm. 5 pp. 640-645|https://doi.org/10.25237/revchilanestv5007061412
PDF|ePub|RIS
Ultrasonografía e impedancia eléctrica como herramientas de evaluación para pacientes críticos en tiempos de COVID-19
Abstract
In the COVID-19 outbreak we are living currently, the lung ultrasound can be considered as an advantageous tool to examine patients as it can be easily used by a maximum of two trained operators, at the bedside. Likewise, the Electrical impedance tomography is useful to monitor and optimize the patient’s ventilation strategies in real time. Here, we present the impact and implication of ultrasonography and electrical impedance as management tools for treating critical patients in times of COVID-19. Clinical Ultrasound has been used more and more in developing countries in Latin America such as Colombia, Argentina, and Uruguay among others, however it is still underutilized due to different issues amongst we found the absence of equipment or the lack of basic training from the medical staff and poor skills to use the machines despite their availability. The use of lung ultrasound and the Electrical impedance tomography is highlighted as a safe manner to manage COVID-19 patients, not as a replacement of a CT scan, but as an easy-to-use and fast complementary tool.
Resumen
En la pandemia de COVID-19 que se vive actualmente, la ultrasonografía pulmonar puede considerarse como una herramienta ventajosa para examinar a los pacientes, ya que puede ser utilizada fácilmente al pie de cama por un máximo de dos operadores capacitados. Asimismo, la tomografía de impedancia eléctrica es útil para monitorizar y optimizar las estrategias de ventilación del paciente en tiempo real. Aquí se presenta el impacto y la implicación de la ecografía y la impedancia eléctrica como herramientas de manejo para el tratamiento de pacientes críticos en tiempos de COVID-19. El ultrasonido clínico se ha utilizado cada vez más en países en vías de desarrollo de América Latina como Colombia, Argentina y Uruguay entre otros, sin embargo, aún está infrautilizado debido a diferentes cuestiones entre las que encontramos la ausencia de equipos o la falta de formación básica del personal médico y la poca habilidad para usar las máquinas a pesar de su disponibilidad. Se destaca el uso de la ultrasonografía pulmonar y la tomografía de impedancia eléctrica como una forma segura de manejar a los pacientes con COVID-19, no como un reemplazo de una tomografía computarizada, sino como una herramienta complementaria rápida y fácil de usar.
-
Introduction
The management of critical patients requires fast and ef- ficient evaluation and diagnosis in order to improve out- comes[1]. In Emergency Medicine (EM), the physicians have been employing a useful, noninvasive imaging tool called Point-of-care ultrasound (POCUS), which has been proven ac- curate in diagnosis and decision-making[2]. The use of this technique has been spreading worldwide mainly due to its cost- effective advantages[3]-[5]. In North America for instance, the early support from the American College of Emergency Medicine (ACEP) and the Society for Academic Emergency Medicine lead to the introduction of ultrasonography as a standard part of the training by the EM residency programs in the United States of America (U.S.A) and Canada[2],[6]. The use of this tool in medical practice has increased significantly over the past few decades as it has become easier to access due to the technology advance. Nowadays there are compact and portable Ultrasound (US) machines for bedside use and even applications for smart- phones that connect to a scanning probe, allowing the medical staff to perform a more practical ultrasonography[3],[7].
A study made by Estenssoro et al.[8] points out that 18% of the intensive care unit (ICU) in Latin-America did not own portable ultrasound devices, which adds to the inequalities in access to health services in Latin-American countries. Also, ac- cording to Blanco[9], developing countries seem to lack of local experts who can appropriately use the US and instruct other colleagues, which shows a need of medical staff capacitation in this matter. In Colombia in the last 10 years the US appears as a first-line tool in the assessment of critical patients, both in the perioperative, ICU and emergency room settings. This method has become one of the most successful at the time of making diagnoses in life threatening situations, such as shock states.
-
Impact and implications of US in developed countries
Developed countries in Europe, North-America and Asia have been training their medical staff in the use of US machines given the importance of this device in diagnosis, mainly in criti- cal patients. The Royal College of Radiologists recognizes the increasing availability of US and even published guidelines for non-radiologists who want to train in this technique[10]. In fact, a survey-study made in Europe by Galarza et al.[10] shows that UK, Italy, Netherlands, Germany and Spain have a nationally accredited programmed in Intensive Care Medicine (ICM) Echo- cardiography, meanwhile other countries also from Europe are in process of developing one. The authors also found that Lung and vascular access ultrasound are the most well-established, and that the use of US Scan in Trauma is part of the training of the majority of emergency physicians.
Mourtzakis et al.[11] explain the impact of US in the ICU for quantification of skeletal muscle, this allows the identifica- tion of the patients with low muscle quantity which has been related to poor clinical outcomes such as reduced ventilator- free days and even increased mortality. Robba et al.[12] on the other hand found that US-based non-invasive intracranial pressure (ICP) measurements combined with venous Transcra- nial Doppler are useful to diagnose patients with severe brain injury. Likewise, Cardim et al.[13] mentions that Transcranial Doppler ultrasonography has a potential advantage as it comes
handy to monitor changes of ICP in time. Vieillard-Baron and Mayo[14] also found lung US and echocardiography in the ICU to be a helpful guide in diagnosis and management of criti- cal patients, concluding that most common cases where critical care US is used are pulmonary edema, weaning failure from the ventilator and circulatory failure[15],[16]. A similar conclu- sion reached See et al.[17] in their study where they compared chest radiography and lung ultrasound for the identification of acute respiratory distress syndrome. These authors suggest to both techniques should be used to complement each other to identify patients at higher risk of death. Furthermore, Umbrello et al.[18] point out that bedside US in critically illness patients with assisted breathing is a simple and non-invasive method of quantification of diaphragm contractile activity. It also is key to directly visualize the thickness of the diaphragm, which is useful to reflect the magnitude of the diaphragm effort. This assess- ment can potentially lead to identify and improve treatment of patients recovering from diaphragm weakness[18].
-
Impact and implications of US in Latin-America
The US imaging technique has been extensively used across different health fields, but in critical patients is key to make rapid diagnosis and make decisions to improve the outcomes. Unfortunately, there are not many articles published regarding the impact of US in Latin America. Jiménez et al.[19] shows how the ocular US is a useful tool in patients with trauma brain injury in emergency service and intensive care, highlighting that the importance of bedside US as a helpful, noninvasive and fast procedure that comes as an alternative to assess patients with intracranial pressure elevated. Also, in the field of transplanta- tion is important the use of US as it was shown by the study made in Colombia by Camacho et al.[20]. This author men- tions that some potentially treatable nonvascular complications of liver transplantation are visible at imaging techniques such as US, leading to accurate diagnosis and enabling patients to benefit from treatment options. This tool is commonly the first performed in order to identify the cause of abnormal liver func- tion[20].
Although clinical ultrasound in critically ill patients is cur- rently been more and more used in developing countries in Lat- in America, such as Colombia[21], Argentina, Uruguay, Brazil and Cuba, it is still underutilized as shown in the study by Este- nssoro et al.[8]. According to Sippel et al.[22] only few studies address the impact of ultrasound use in clinics and the patient outcomes, as well as whether this tool can be sustainable in low and middle-income countries (LMICs). Medical teams that practice in remote areas have limited choices when it comes to diagnostic tools, but an interesting study made by Blaivas et al.[23] in the Amazon jungle found that a portable US can be significantly useful, beneficial, and can alter disposition and treatment for the patients drastically. One of the largest study made in Latin-American Intensive Care Units (ICUs) identifies several issues regarding the delivery of critical care in the region such as a lack of their own US devices[8]. Unfortunately, the absence of equipment is not the only cause of underuse; in the case of Argentina and Uruguay, according to Blanco[9], the use of this tool is low, the author highlights that less than 20% of the medical staff have the basic training and skills to use the machines despite their availability.
-
Advantages of using US in critical patients
Among the advantages of using US in critical patients in- stead of other imagine tools, there is the cost-effectiveness to reduce the use of tomography, given that tomographs are very expensive to use. The US should not be a replacement for the tomography by any means, but for initial diagnosis and to take quick actions on critical patients, it is a powerful and efficient technique[24]. On the other hand, when compared to the X- rays, the US would not produce radiation on patients as US uses instead, high frequency sound waves and their echoes, not exposing the users to major risks when used appropriately[25]. Similarly to tomography, X-rays should not be replaced by US, but used as a complement, when the patients are being initially treated and there is no reason to believe an X-ray is needed. Moreover, according to Marhofer & Frickey[26], the US has the advantage to be of greater patient comfort and implicates less opioid use.
Given the importance of performing US in critical patients, physicians must reach a suitable level of competence in using the US device and examining patients[27]. In Canada, France and the U.S.A, the use of US has been implemented as a policy in hospitals. The government of Canada in fact, has a “Guidelines for the Safe Use of Ultrasound: Part I – Medical and Paramedical Applications” which includes recommen- dations for care of equipment, operator and patient safety precautions, and operator training. According to their official web page, courses for training personal in the US technique are available in eleven universities across Canada in their pro- grams of Physical Therapy or Rehabilitation. According to a recent survey study in Canada by Mok et al.[28] all respon- dents’ residency programs provide some training in POCUS- facilitated vascular access, peripheral nerve blocks, neuraxial techniques, and transthoracic echocardiography. Also, the most frequent teaching method employed was informal bed- side teaching, among others. The respondents also agreed that POCUS should be incorporated into the National Curriculum for Canadian Anesthesiology Residency. Likewise, Atkin- son et al.[29] states that POCUS skills are critical to the clinical development of an emergency physician, and all graduating Emergency Medicine (EM) residents should be provided with a minimum skill set. On the other hand in Canada, while learn- ers advance from the medical student stage are trained in US as an educational tool, postgraduate students from medical education are trained to be more independent, and they learn skills sets that integrates focused ultrasound findings into clin- ical decision making[30].
-
Use of US in management of patients with COVID-19
Patients with symptoms of COVID-19 can be examined by using standard methods such as radiological tests or chest CT, nevertheless, the use of these methods implies the possible contamination of medical devices and medical staff, who are at high risk of contracting the infection[31]. In the COVID-19 outbreak we are living currently, we need to minimize the num- ber of medical workers and devices exposed to the coronavirus, and the lung US can be considered as an advantageous tool to examine patients as it can be easily used by a maximum of two trained operators[32], at the bedside. Moreover, there are
portable US that are compact and wireless, allowing the use of two single-use plastic covers. In addition, according to Doctor Giovanni Volpicelli, during the experience in Turin, Italy with COVID-19, the medical staff realized that they could not pre- dict which patients might develop severe pneumonia with age or comorbid conditions[33]. Doctor Volpicelli then developed a new protocol to triage patients using bedside lung ultrasounds with which they can effectively identify patients who need to be admitted and those who can be sent home under quaran- tine. Lung US can identify physical changes of superficial lung tissue as well as detect lung lesions before the development of hypoxemia. POCUS at the bedside of the patients present- ing ventilatory failure can be fundamental to evaluate the lung overload conditions and ventricular failure in these patients. Ac- cording to Soldati et al.[34] the clinical evidence found from patients with COVID-19 pneumonia, there is a pattern seen in Lung US, represented by a patchy distribution of interstitial artifactual signs, which extend to multiple areas of the lung surface. Subsequently, small subpleural consolidation with as- sociated areas of white lung appear and, when they began to expand along the lung surface, it indicated the evolution of the patient to a phase of respiratory insufficiency, requiring invasive ventilatory support (Figure 1).
Furthermore, Buonsenso et al.[35] presented a case report of a 52 year-old man who presented COVID-19 sympthoms and tested positive, received a lung US in which the medical team found on the anterior and posterior emi-thorax bilaterally, an irregular pleural line with small subpleural consolidations, areas of white lung and thick, confluents and irregular vertical artifacts (B-lines). The images obtained for the patient were then compared with a control-case, which showed a normal pleural line with A-lines regularly reverberating and only one, B- line noted in a single area. Pattern A represents a typical normal aeration condition (Figure 2), however, COVID-19 pneumonia can be represented as a storm of clusters of B-lines, in separate and coalescent forms, occasionally giving a shining white lung appearance (Figure 3).
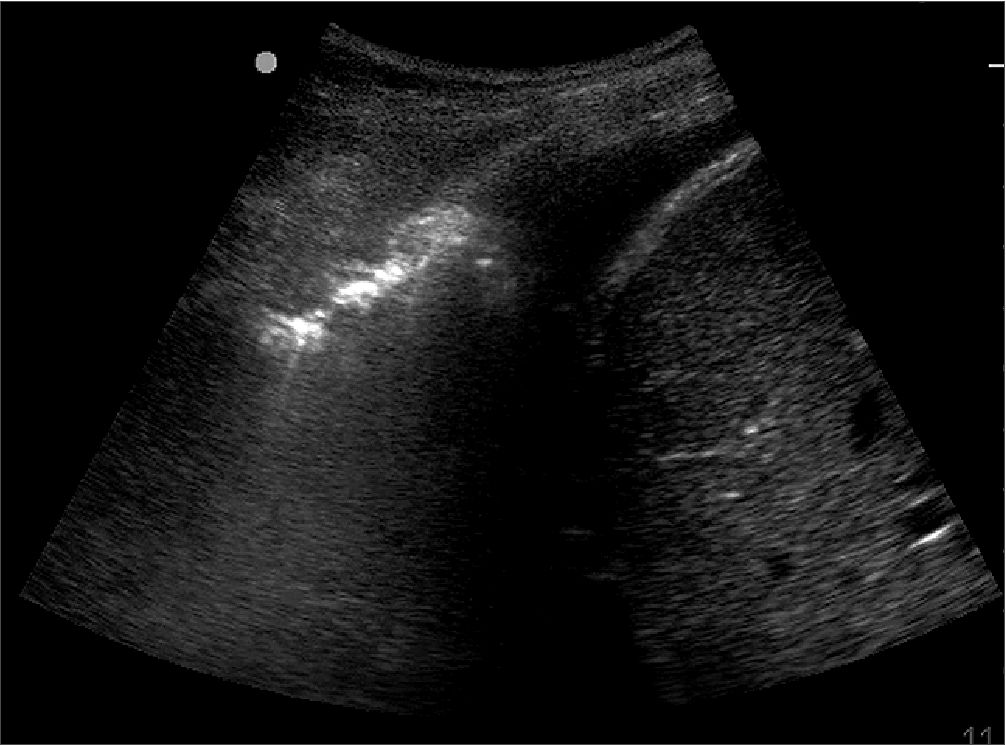
Figure 1. Consolidation pattern observed in the lung US of a patient with COVID-19.
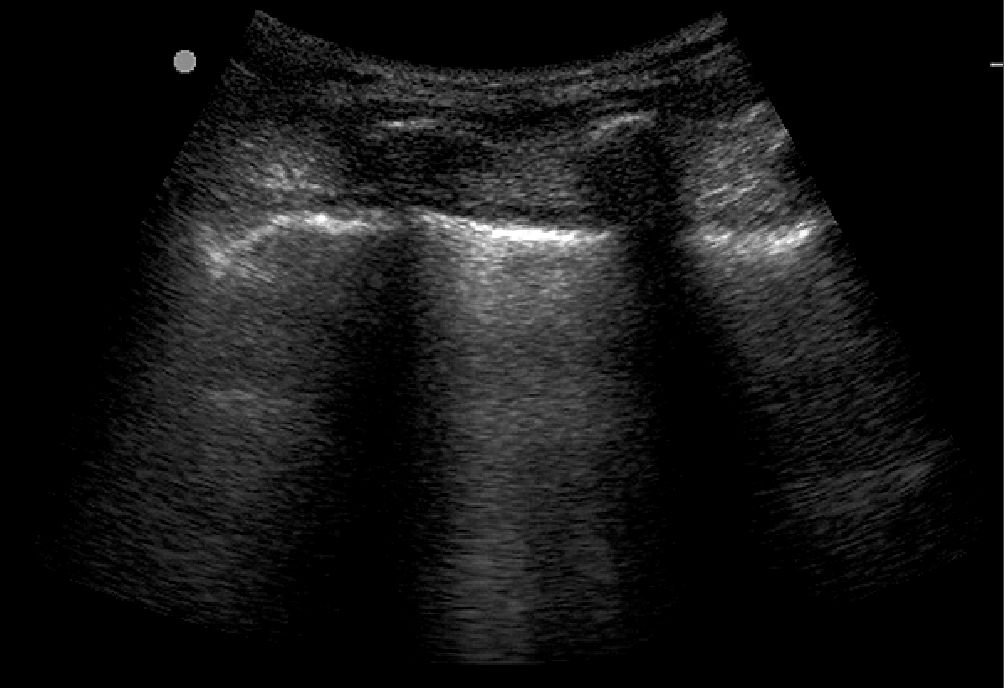
Figure 2. A-lines lung pattern observed in the US of a patient with COVID-19.
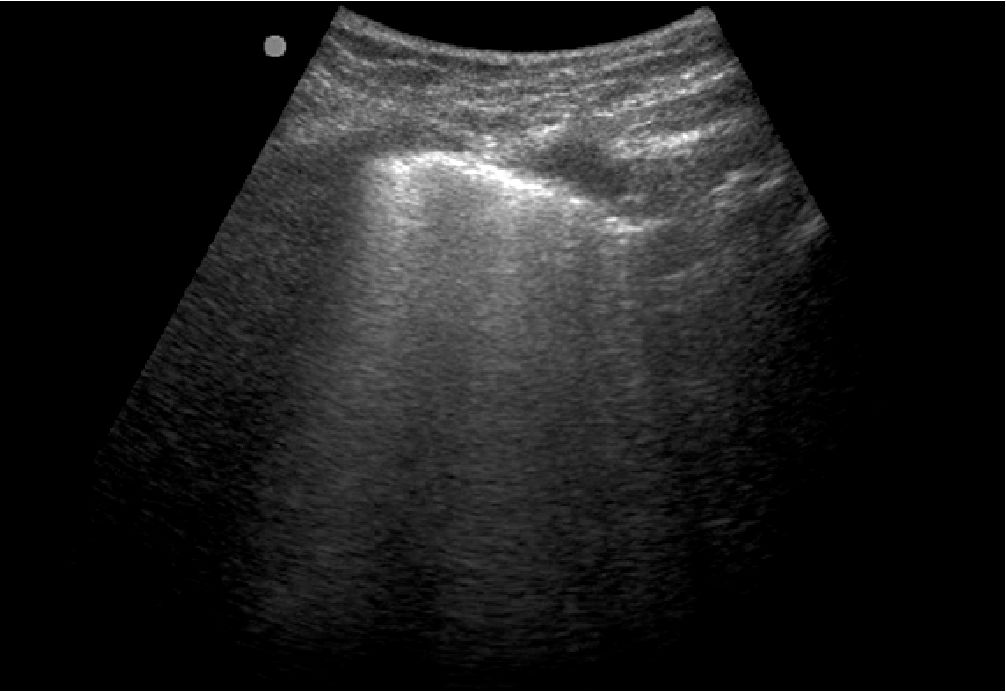
Figure 3. B-lines lung pattern observed in the US of a patient with COVID-19.
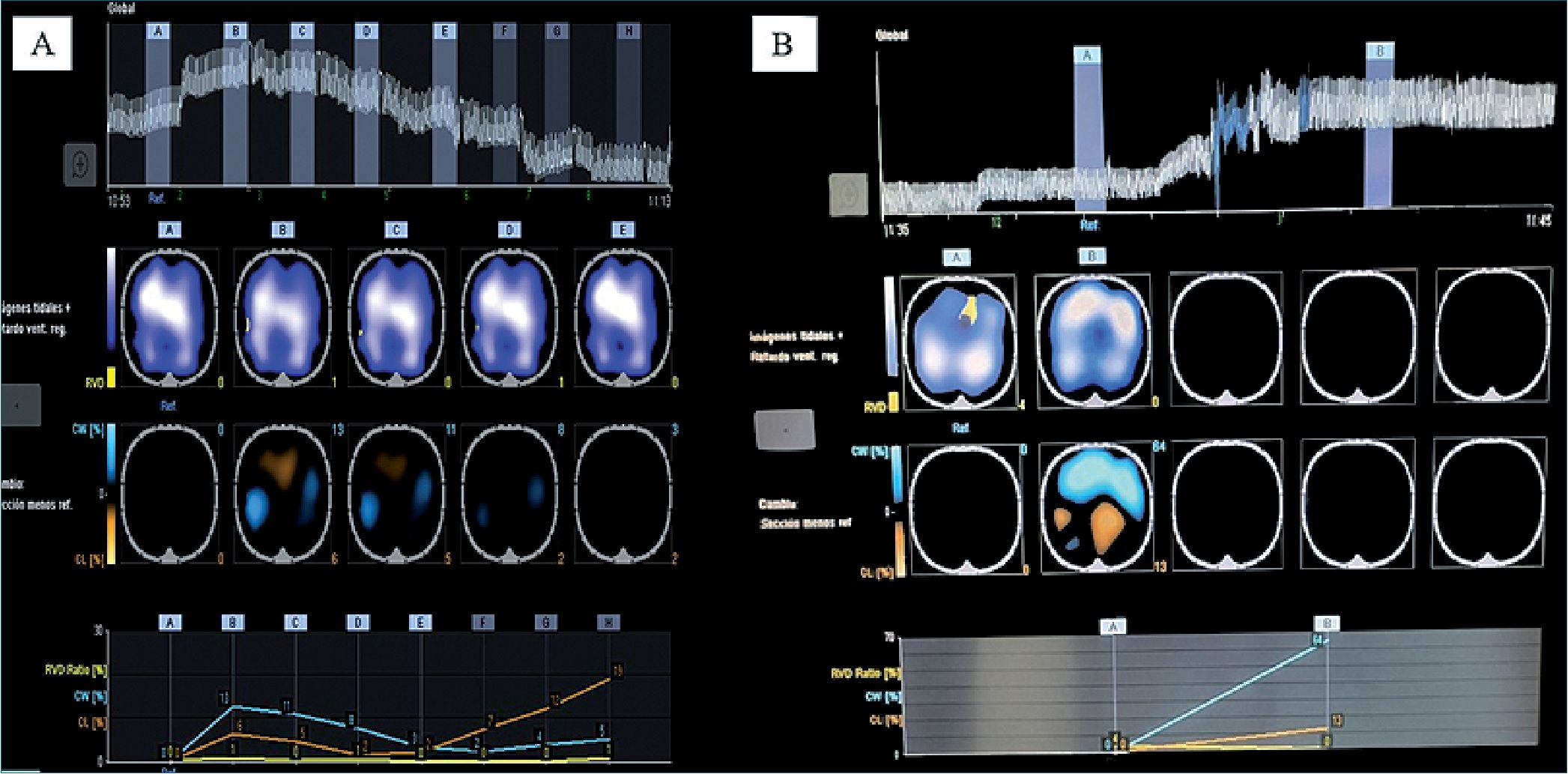
Figure 4. EIT of patient that improved with prone position.
-
Use of Electrical impedance tomography in management of patients with COVID-19
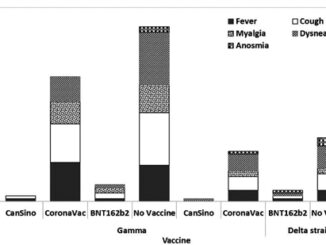
EIT is a technique related to the length generated by the distension of the alveolus when it is ventilated, being able to in- dicate if the patient is optimally ventilated or if he / she presents an overdistention due to ventilation. The image obtained with this technique is similar to a tomography. With this technique it is possible to monitor and optimize the patient’s ventilation strategies in real time[36],[37], allowing the analysis of the im- pedance generated by the tissues, in this specific case, the lung tissue. In summary, the technique can provide information on over-inflation, recruitment, and cyclical alveolar collapse at the bedside, thereby improving the ventilation strategies used[38]. The impedance analysis can indicate if a patient has an ade-
quate ventilation or if, on the contrary, it is diminished, and if it is potentially recruitable for optimal oxygenation of ventila- tion. Figure 4 shows the results of an EIT analysis, the zone of adequate ventilation (white zone) increased, and the zone of slow filling (yellow zone) was reduced, indicating a complete optimization of the patient’s ventilation.
-
Conclusions
In Colombia, specifically in the perioperative and critical care area, the use of the US has not become widespread due to the high cost of the equipment and the poor training of medical staff. In this sense, the implementation of US within the training of anesthesiology residency programs should be
promoted in a formal manner; even from undergraduate in care-related courses, as it is a tool that allows an early diagnosis of life-threatening diseases and helps define a much faster behavior by the medical team. Moreover, there is still no clarity about the pathophysiology of lung injury associated with CO- VID-19, however, with impedance tomography and US, earlier and more timely changes can be made in patient management since they are techniques that are done in bedside in real time. These changes can define the ideal PEEP, whether the patient should pronate, or if more invasive procedures are required, such as the placement of pleural fluid drainage catheters. Given our current situation, the use of lung US is needed as a safe manner to examine patients with COVID-19 symptoms, identi- fying lung involvement and severity, reducing the risk of spread the virus. The utility of the EIT and the lung US to manage CO- VID-19 patients is highlighted, not as a replacement of a CT scan, but as an easy-to-use and fast complementary tool.
Funding sources: This research did not receive funding for its realization.
Conflicts of interest: The authors have no conflicts of interest to disclosure regarding the publication of this article.
References
1. Stowell JR, Kessler R, Lewiss RE, Barjaktarevic I, Bhattarai B, Ayutyanont N, et al. Critical care ultrasound: A national survey across specialties. J Clin Ultrasound. 2018 Mar;46(3):167–77. https://doi.org/10.1002/jcu.22559 PMID:29131347
2. Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care. 2016 Aug;20(1):227. https://doi.org/10.1186/s13054-016-1399-x PMID:27523885
3. Charron C, Repessé X, Bodson L, Au SM, Vieillard-Baron A. Ten good reasons why everybody can and should perform cardiac ultrasound in the ICU. Anaesthesiol Intensive Ther. 2014 Nov-Dec;46(5):319–22. https://doi.org/10.5603/AIT.2014.0055 PMID:25432551
4. Yin W, Li Y, Zeng X, Qin Y, Wang D, Zou T, et al. The utilization of critical care ultrasound to assess hemodynamics and lung pathology on ICU admission and the potential for predicting outcome. PLoS One. 2017 Aug;12(8):e0182881. https://doi.org/10.1371/journal.pone.0182881 PMID:28806783
5. Zieleskiewicz L, Bouvet L, Einav S, Duclos G, Leone M. Diagnostic point-of-care ultrasound: applications in obstetric anaesthetic management. Anaesthesia. 2018 Oct;73(10):1265–79. https://doi.org/10.1111/anae.14354 PMID:30047997
6. AlEassa EM, Ziesmann MT, Kirkpatrick AW, Wurster CL, Gillman LM. Point of care ultrasonography use and training among trauma providers across Canada. Can J Surg. 2016 Feb;59(1):6–8. https://doi.org/10.1503/cjs.010215 PMID:26574705
7. Enriquez JL, Wu TS. An introduction to ultrasound equipment and knobology. Crit Care Clin. 2014 Jan;30(1):25–45. https://doi.org/10.1016/j.ccc.2013.08.006 PMID:24295840
8. Estenssoro E, Alegría L, Murias G, Friedman G, Castro R, Nin Vaeza N, et al.; Latin-American Intensive Care Network (LIVEN). Organizational Issues, Structure, and Processes of Care in 257 ICUs in Latin America: A Study From the Latin America Intensive Care Network. Crit Care Med. 2017 Aug;45(8):1325–36. https://doi.org/10.1097/CCM.0000000000002413 PMID:28437376
9. Blanco P. Critical Care Ultrasound in Developing Countries of Latin America: A Long Way to Go. J Ultrasound Med. 2019 Jun;38(6):1617–8. https://doi.org/10.1002/jum.14833 PMID:30269337
10. Galarza L, Wong A, Malbrain ML. The state of critical care ultrasound training in Europe: A survey of trainers and a comparison of available accreditation programmes. Anaesthesiol Intensive Ther. 2017;49(5):382–6. https://doi.org/10.5603/AIT.a2017.0075 PMID:29192421
11. Mourtzakis M, Parry S, Connolly B, Puthucheary Z. Skeletal muscle ultrasound in critical care: A tool in need of translation. Ann Am Thorac Soc. 2017 Oct;14(10):1495–503. https://doi.org/10.1513/AnnalsATS.201612-967PS PMID:28820608
12. Robba C, Cardim D, Tajsic T, Pietersen J, Bulman M, Donnelly J, et al. Ultrasound non-invasive measurement of intracranial pressure in neurointensive care: A prospective observational study. PLoS Med. 2017 Jul;14(7):e1002356. https://doi.org/10.1371/journal.pmed.1002356 PMID:28742869
13. Cardim D, Robba C, Bohdanowicz M, Donnelly J, Cabella B, Liu X, et al. Non-invasive Monitoring of Intracranial Pressure Using Transcranial Doppler Ultrasonography: Is It Possible? Neurocrit Care. 2016 Dec;25(3):473–91. https://doi.org/10.1007/s12028-016-0258-6 PMID:26940914
14. Vieillard-Baron A, Mayo P. Lung ultrasonography and echocardiography in the Intensive Care Unit: a combined and practical approach. Minerva Anestesiol. 2018 Mar;84(3):398–408. https://doi.org/10.23736/S0375-9393.17.12264-9 PMID:29027776
15. Antonio AC, Knorst MM, Teixeira C. Lung ultrasound prior to spontaneous breathing trial is not helpful in the decision to wean. Respir Care. 2018 Jul;63(7):873–8. https://doi.org/10.4187/respcare.05817 PMID:29666295
16. Brogi E, Gargani L, Bignami E, Barbariol F, Marra A, Forfori F, et al. Thoracic ultrasound for pleural effusion in the intensive care unit: a narrative review from diagnosis to treatment. Crit Care. 2017;21(1):1–11. https://doi.org/10.1186/s13054-017-1897-5 PMID:28057037
17. See KC, Ong V, Tan YL, Sahagun J, Taculod J. Chest radiography versus lung ultrasound for identification of acute respiratory distress syndrome: a retrospective observational study. Crit Care. 2018 Aug;22(1):203. https://doi.org/10.1186/s13054-018-2105-y PMID:30119687
18. Umbrello M, Formenti P. Ultrasonographic Assessment of Diaphragm Function in Critically Ill Subjects. Respir Care. 2016 Apr;61(4):542–55. https://doi.org/10.4187/respcare.04412 PMID:26814218
19. Jiménez Restrepo JN, León OJ, Quevedo Florez LA. Ocular Ultrasonography: A Useful Instrument in Patients with Trauma Brain Injury in Emergency Service. Emerg Med Int. 2019 Jan;2019:9215853. https://doi.org/10.1155/2019/9215853 PMID:30805217
20. Camacho JC, Coursey-moreno C, Telleria JC, Aguirre DA, Torres WE, Mittal PK. Nonvascular Post – Liver Trans plantation Complications : From US Screening to Cross-sectional and. Radiographics. 2015;1963(2):87–104. https://doi.org/10.1148/rg.351130023 PMID:25590390
21. Caballero AF, Villarreal K. Ultrasound for central vascular access. A safety concept that is renewed day by day [Review]. Colomb J Anesthesiol. 2018;46:35–41. https://doi.org/10.1097/CJ9.0000000000000043.
22. Sippel S, Muruganandan K, Levine A, Shah S. Review article: use of ultrasound in the developing world. Int J Emerg Med. 2011 Dec;4(1):72. https://doi.org/10.1186/1865-1380-4-72 PMID:22152055
23. Blaivas M, Kuhn W, Reynolds B, Brannam L. Change in differential diagnosis and patient management with the use of portable ultrasound in a remote setting. Wilderness Environ Med. 2005;16(1):38–41. https://doi.org/10.1580/1080-6032(2005)16[38:CIDDAP]2.0.CO;2 PMID:15813146
24. Panés J, Bouzas R, Chaparro M, García-Sánchez V, Gisbert JP, Martínez de Guereñu B, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment Pharmacol Ther. 2011 Jul;34(2):125–45. https://doi.org/10.1111/j.1365-2036.2011.04710.x PMID:21615440
25. Jain R, Jain N, Sheikh T, Yadav C. Early scaphoid fractures are better diagnosed with ultrasonography than X-rays: A prospective study over 114 patients. Chin J Traumatol. 2018 Aug;21(4):206–10. https://doi.org/10.1016/j.cjtee.2017.09.004 PMID:29551580
26. Marhofer P, Frickey N. Ultrasonographic guidance in pediatric regional anesthesia Part 1: theoretical background. Paediatr Anaesth. 2006 Oct;16(10):1008–18. https://doi.org/10.1111/j.1460-9592.2006.02020.x PMID:16972828
27. Andruszkiewicz P, Sobczyk D. Ultrasound in critical care. Anaesthesiol Intensive Ther. 2013 Jul-Sep;45(3):177–81. https://doi.org/10.5603/AIT.2013.0036 PMID:24092516
28. Mok D, Schwarz SK, Rondi K. Point-of-care ultrasonography in Canadian anesthesiology residency programs: a national survey of program directors. Can J Anaesth. 2017 Oct;64(10):1023–36. https://doi.org/10.1007/s12630-017-0935-8 PMID:28755100
29. Atkinson P, Ross P, Henneberry R. Coming of age: emergency point of care ultrasonography in Canada. CJEM. 2014 Jul;16(4):265–8. https://doi.org/10.2310/8000.2013.131186 PMID:25060078
30. Ma IW, Steinmetz P, Weerdenburg K, Woo MY, Olszynski P, Heslop CL, et al. The Canadian Medical Student Ultrasound Curriculum: A Statement From the Canadian Ultrasound Consensus for Undergraduate Medical Education Group. J Ultrasound Med. 2020 Jul;39(7):1279–87. https://doi.org/10.1002/jum.15218 PMID:31943311
31. Cheung JC, Ho LT, Cheng JV, Cham EY, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020 Apr;8(4):e19. https://doi.org/10.1016/S2213-2600(20)30084-9 PMID:32105633
32. Buonsenso D, Pata D, Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med. 2020 May;8(5):e27. https://doi.org/10.1016/S2213-2600(20)30120-X PMID:32203708
33. Trivedi JN. An economical model for mastering the art of intubation with different video laryngoscopes. Indian J Anaesth. 2014 Jul;58(4):394–6. https://doi.org/10.4103/0019-5049.138967 PMID:25197105
34. Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, et al. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J Ultrasound Med. 2020 Jul;39(7):1459–62. https://doi.org/10.1002/jum.15284 PMID:32198775
35. Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020 Mar;24(5):2776–80. https://doi.org/10.26355/eurrev_202003_20549 PMID:32196627
36. Safaee Fakhr B, Araujo Morais CC, De Santis Santiago RR, Di Fenza R, Gibson LE, Restrepo PA, et al. Bedside monitoring of lung perfusion by electrical impedance tomography in the time of COVID-19. Br J Anaesth. 2020 Nov;125(5):e434–6. https://doi.org/10.1016/j.bja.2020.08.001 PMID:32859359
37. Moerer O, Hahn G, Quintel M. Lung impedance measurements to monitor alveolar ventilation. Curr Opin Crit Care. 2011 Jun;17(3):260–7. https://doi.org/10.1097/MCC.0b013e3283463c9c PMID:21478747
38. Liu S, Tan L, Möller K, Frerichs I, Yu T, Liu L, et al. Identification of regional overdistension, recruitment and cyclic alveolar collapse with electrical impedance tomography in an experimental ARDS model. Crit Care. 2016 May;20(1):119. https://doi.org/10.1186/s13054-016-1300-y PMID:27142073

 ORCID
ORCID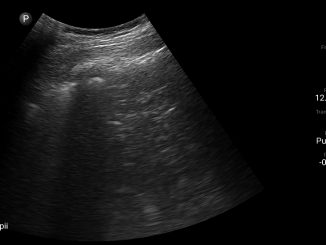

 Creative Commons Attribution
Creative Commons Attribution