Abstract
Phantosmia has been described as a sense of smell without a true stimulating odor and not been reported with COVID-19 disease. Nine patients admitted to Ear Nose Throat (ENT) Clinic with complaints of a phantom smell sense after an average of 33.5 ± 9.5 days after the initial PCR diagnosis. According to the Sniffin 'Sticks test, phantosmia was associated with objective hyposmia in three patients with the persistent phantom smell, and other six patients were detected normosmic. Phantosmia or olfactory hallucinations have not been previously associated with COVID-19 disease. Additionally, COVID-19 related phantosmia showed different characteristics according to described in the literature.
Similar content being viewed by others
Introduction
Phantosmia has been described as a sense of smell without a true stimulating odor and is a subjective olfactory dysfunction. Olfactory hallucinations have been previously associated with migraine typed headaches, endoscopic skull base surgery, intracranial tumors, brain radiotherapy treatment, and head trauma in the literature [1]. As described in the literature, phantosmia can persist for years. Olfactory dysfunction is one of the preliminary symptoms of COVID-19 disease, and it can occur as hyposmia, anosmia, or and sudden loss of smell [2]. However, COVID-19 related phantosmia or olfactory hallucination has not been reported in the literature before. In this report, nine confirmed COVID-19 patients with olfactory hallucinations were presented.
Case Report
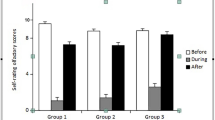
The demographic and clinical characteristics of the patients are summarized in Table 1. All of the patients admitted to Ear Nose Throat (ENT) Clinic at second referential state hospital with complaints of a phantom smell sense after an average of 33.5 ± 9.5 days after the initial PCR diagnosis. All patients had completed COVID-19 treatment and emerged from isolation. The main symptoms of the patients were fever, cough, and weakness at the initial diagnosis. Three patients had Sars-Cov-2 related thorax Computed Tomography (CT) findings. All patients confirmed for COVID-19 disease with PCR test by nasopharyngeal swabs. Aura-like phantom odor sensation noticed by three patients during two or three days of the disease when symptoms were most severe and then disappeared. Two patients reported that the phantom smell sense continued during the disease but the onset of phantom smell was not distinguished. Four (44.4%) patients still complained of phantom odor during ENT admission. According to the Sniffin' Sticks test, phantosmia was associated with objective hyposmia in three (33.3%) patients with the persistent phantom smell (TDI score between 15.5 and 30.5; odor threshold, odor discrimination, and odor identification).
Medical treatment included hydroxychloroquine (200 mg bid for 5 days), moxifloxacin (400 mg once daily for 7 days), favipiravir (Day 1: 1600 mg bid for the first day; 600 mg bid 2–5 days), enoxaparin (40–60 mg/d), dexamethasone (20 mg/d for first 3 days, then 4 mg/d) for all patients. During the disease, only a mild C-reactive protein (CRP) elevation was present in three (33.3%) patients (Table 1). In eight (88.8%) patients, the PCR test turned negative 1 week after the initiation of treatment, while PCR became negative at the 4th week for a 32-year-old male patient. Interestingly, in this patient, only dizziness continued for 40 days. In the ENT examination of the patients, septum deviation, concha hypertrophy, discharge, mucosal dryness, congestion, or nasal polyp were not detected. In addition, none of these patients had ever experienced phantosmia before. None of the patients had a history of chronic disease, chronic drug use, maxillofacial trauma, or surgery. The follow-up period was 60.4 ± 23.0 days after first ENT admission. Brain Magnetic Resonance Imaging (MRI) was performed for all patients and no pathology was found (Fig. 1). While only observation recommended for three patient with persistent phantosmia, carbamazepine (400 mg daily, p.o.) was prescribed to one patient who had difficulty eating because of nausea due to dirt smell sensation. Two months after the carbamazepine treatment, the patient reported that she could tolerate dirt smell, but her phantom sense of smell did not disappear.
Discussion
Hyposmia, anosmia, or sudden onset of anosmia were shown significant symptoms for asymptomatic or mild COVID-19 disease although the mechanism of the olfactory dysfunction was not understood [3]. Phantosmia was classified as a qualitative disturbance of smell function and during the COVID-19 pandemic, this phenomenon was not reported. Phantosmia occurs due to a number of etiologies, including chronic rhinosinusitis, cranial trauma, intracranial hemorrhage, epilepsy, psychiatric conditions, brain radiotherapy, neurologic disorders, iatrogenic causes, and neurologic and neurodegenerative disorders and conductive or sensorineural pathophysiology of this specific symptom is still unclear [1]. The frequency of phantosmia has been reported by up to 25% in patients with odor disorder, and the incidence is higher in the elderly compared to the young population [3]. Sjölund et al. [4] reported that phantom smells were experienced less than once a month (54%) and the most frequently reported phantom smell was smoky or burnt (46%) in a population-based study. In addition, in this study, it was reported that only 17% of patients with a phantom sense of smell had this entity for less than a year. Long-term phantosmia impairs quality of life so, medical, surgical, and olfactory training as treatment options have been reported in current literature [5].
Gender distribution of the patient similar to reported literature, but despite the increasing frequency of phantosmia with age, all of the patients presented were in the young age group (< 40 y/o). All patients in this study had not previously noted olfactory disturbance or phantosmia. Five of nine (55.5%) patient has not experienced olfactory hallucination again after their symptoms of COVID-19 has regressed. In addition, three patients reported that the phantom smell sensation very obvious at the most severe period of COVID-19 symptoms. Interestingly, five (55.5%) patients had no complaints of anosmia or hyposmia during COVID-19 disease, but hyposmia with phantosmia was detected in a female patient on ENT admission (TDI score: 25.8). While phantosmia persisted in four (44.4%) patients, the sense of phantom smell disappeared in five (55.5%) patients with recovery from COVID-19 disease. Although follow without any treatment was recommended for all patients, a patient with persisted phantosmia requested medical treatment because of the unbearable dirty smell. Monthly control was recommended for all patients with persistent phantosmia. The patient with carbamazepine treatment reported that the sensation of dirty smell decreased in the second month of the follow-up and the treatment was stopped. The request for treatment of the patient disappeared in the 3rd month of follow-up.
Phantosmia or olfactory hallucinations have not been previously associated with COVID-19 disease, however, the development of phantosmia due to olfactory dysfunction is a predictable situation. Although the pathological mechanism is unclear, phantosmia emerged with COVID-19 infection and disappeared after the disease recovery. Although the short follow-up period, this case report showed the presence of a new unusual symptom with COVID-19-associated odor dysfunction.
References
Saltagi MZ, Rabbani CC, Ting JY, Higgins TS (2018) Management of long-lasting phantosmia: a systematic review. Int Forum Allergy Rhinol 8(7):790–796. https://doi.org/10.1002/alr.22108
Parma V, Ohla K, Veldhuizen MG et al (2020) More than smell-COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses 45(7):609–622. https://doi.org/10.1093/chemse/bjaa041
Rawal S, Hoffman HJ, Bainbridge KE, Huedo-Medina TB, Duffy VB (2016) Prevalence and risk factors of self-reported smell and taste alterations: results from the 2011–2012 US National Health and Nutrition Examination Survey (NHANES). Chem Senses 41(1):69–76. https://doi.org/10.1093/chemse/bjv057
Sjölund S, Larsson M, Olofsson JK, Seubert J, Laukka EJ (2017) Phantom smells: prevalence and correlates in a population-based sample of older adults. Chem Senses 42(4):309–318. https://doi.org/10.1093/chemse/bjx006
Morrissey DK, Pratap U, Brown C, Wormald PJ (2016) The role of surgery in the management of phantosmia. Laryngoscope 126(3):575–578. https://doi.org/10.1002/lary.25647
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.


Rights and permissions
About this article
Cite this article
İşlek, A., Balcı, M.K. Phantosmia with COVID-19 Related Olfactory Dysfunction: Report of Nine Case. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2891–2893 (2022). https://doi.org/10.1007/s12070-021-02505-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02505-z