
Clinical course and outcomes of ventilated critically ill COVID-19 patients in Selangor state, Malaysia
Introduction
Coronavirus disease 2019 (COVID-19) has become a pandemic since it was first reported in December 2019 (1). To date, more than 4 million cases have been detected worldwide affecting over 200 countries with mortality exceeding 200,000 patients (2). Malaysia having had its first case in early January 2020, has seen an exponential increase in cases since then (3).
Our center, originally a designated infectious disease (ID) and trauma center of the Selangor state, has been prepared and dedicated to cater for COVID-19 cases ever since. The Selangor state with its population of 6.3 million, recorded 1,604 cases as of May 10, 2020 (4). This is about a quarter of the total cases recorded in the country (6,665 cases). Our intensive care unit (ICU) is geared up to cater to up to 100 critically ill patients if the need arise. The purpose of this case series is to capture data on management and outcome of ventilated COVID-19 patients in our state.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-82).
Methods
In this observational, descriptive case series, we included 49 adult ventilated patients which were confirmed COVID-19 cases via positive reverse-transcriptase polymerase chain reaction (RT-PCR) assays of specimens collected via nasopharyngeal swabs or tracheal aspirate. These patients were admitted between 7th March 2020 until 16th April 2020. These patients were either intubated in our center following clinical deterioration or transferred from surrounding hospital following a positive COVID-19 RT-PCR results.
All mechanically ventilated adult patients admitted to Hospital Sungai Buloh Intensive Care Unit (HSB ICU) within this period were included. We have excluded patients who fell under patients under investigation (PUI) category, but tested negative for COVID-19. Twenty-six COVID-19 positive non-ventilated patients admitted for close observations while on non-invasive oxygen therapy were also excluded. Patients with missing data from electronic and manual records were excluded.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Malaysian Research and Ethics Committee (MREC) (ID: NMRR-20-2441-54853) and individual consent for this retrospective analysis was waived.
Deidentified patient data were collected from our in hospital electronic-health-information-system (e-His) and ICU nursing charts. Baseline demographics, laboratory values, ventilator days & ICU days were recorded.
Statistical analysis
Data was analyzed using IBM SPSS Statistics 23. Results were reported as means, percentage and counts as appropriate. T-tests were used to compare any significant difference between means.
Results
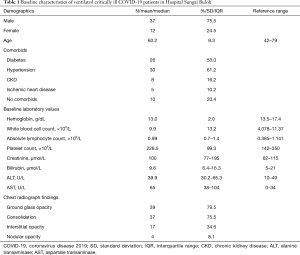
A total of 49 adult patients were included for analysis {mean age, 60 [standard deviation (SD): 9.3]; range, 40–79 years}. The majority are male patients (75%). About 80% of patients had underlying comorbidities, with hypertension being the most common (61.2%) followed by diabetes (53%) and ischemic heart disease (10.2%). A proportion of patient also had pre-existing chronic kidney disease (CKD) (8.1%) and end stage renal failure (ESRF) (8.1%) (Table 1).
Full table
Baseline laboratory values on admission to ICU showed mean Hb of 13 g/dL (SD: 2), median lymphocyte count of 0.99×109/L [interquartile range (IQR): 0.7–1.4], mean white cell count of 9.86×109/L (SD: 13.2) and mean platelet count of 234×109/L (SD: 99). Median creatinine value was above normal at 125 µmol/L (IQR: 77–195). Total bilirubin mean value was within normal range, however median aspartate transaminase (AST) value was elevated twice (65 unit/L, IQR: 38–104) above the normal range whereas median alanine transaminase (ALT) was normal. Forty-eight patients (98%) had abnormal chest radiographs findings as reported by radiologist. The most common changes were ground glass opacity 79.5%, consolidation 75.5%, interstitial opacity 34.6% and nodular opacity in 8% of patients (Table 1).
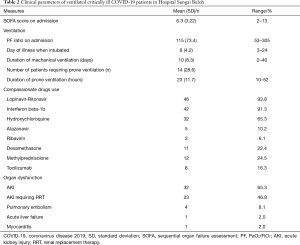
The average sequential organ failure assessment (SOFA) score on admission to ICU was 6 correlating to a predicted 21.5% mortality. Mean PaO2/FiO2 (PF) ratio on admission is 115 (73.4) mmHg reflecting a moderate acute respiratory distress syndrome (ARDS). We observed the tendency for patients to deteriorate clinically between day 4 to 10 of illness thus needing intubation by day 8 (SD: 4.2) of illness. Fourteen patients (28.6%) had to be proned while being mechanically ventilated (Table 2).
Full table
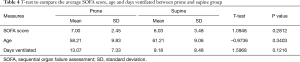
The indication for prone ventilation in our institution is PF ratio of 150 or less despite initiation of mechanical ventilation. These patients were having worsening ground glass opacities on serial chest X-ray despite initiation of mechanical ventilation and compassionate antiviral therapy. They were proned between 16–20 hours per session. In the proned group, there was improvement in mean PF ratio after proning of 155. When analyzed using t-test the P value is 0.000412 which is statistically significant (P<0.05) (Table 3). Patients who have been proned, tend to have higher mean SOFA score on admission and had prolonged mechanical ventilation. However, these differences are not statistically significant (Table 4).

Full table
Full table
All patients received compassionate use of antiviral therapies. The choice of antiviral agents were Lopinavir-Ritonavir 46 (93.8%), Interferon beta-1b 42 (91.3%), Hydroxychloroquine 32 (65.3%), Atazanavir 5 (10.2%) & Ribavirin 3 (6.1%). The selection of antiviral agents were made after joint discussion with ID physicians. Fifteen (30.6%) of patients were given corticosteroid (dexamethasone or methylprednisolone). We also had five patients admitted in the second half of the analysis period who were started on tocilizumab. More than 90% of patients received broad spectrum antibiotics for nosocomial infections throughout their ICU stay (Table 2).
A significant number of patients developed organ dysfunctions during their clinical course. The most common organ dysfunction was acute kidney injury (AKI) occurring in 32 patients (65.3%). Of this, 23 patients (46.9%) eventually needed dialysis. The latest classification by Acute Kidney Injury Working Group of KDIGO (Kidney Disease: Improving Global Outcome) is used to define AKI (5). Four patients developed pulmonary embolism diagnosed by CT pulmonary angiogram. Acute liver failure occurred in one patient, who eventually succumbed to death. A female patient also developed myocarditis which eventually progressed to fatal cardiogenic shock (Table 2).
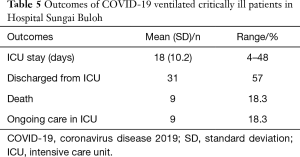
Our patients were ventilated on average of 11 days. Mean ICU stay was 18 (10.2) days. 30 patients (61%) were managed to be extubated and discharged. Eleven patients are still being managed in ICU. The remaining patients with prolonged ICU stay are either intubated due to prolonged ventilation or awaiting recovery from nosocomial infection. Of those who were extubated but remain in ICU, were the patients with AKI awaiting renal recovery. At the time of writing, we have recorded nine deaths which made up about 18.3% of ventilated patients. Majority of patients died of multiorgan failure complications (Table 5).
Full table
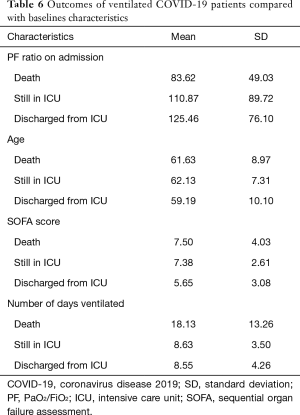
Patients with worse clinical outcomes i.e., death or prolonged ICU stay, tend to be older, had higher SOFA scores in the first 24 hours of admissions and lower baseline PF ratios (Table 6).
Full table
Discussion
This case series represented critically ill COVID-19 patients who required mechanical ventilation in our ICU. We also managed non-ventilated patient requiring oxygen therapy with hypoxemic failure or organ failure that needs close monitoring. The latter group of patients benefited from early ICU care and avoid intubation by having close monitoring & meticulous fluid balance. Thus, our ICU workload is more than what has been described.
We have observed a higher incidence of AKI, which is 65% compared to 29% in an observational study by Yang et al. in Wuhan (6). Possible factors include a large number of elderly patients with hypertension and undiagnosed CKD who presented late to the hospital. They were among our biggest group of patients who were the most ill needing multiorgan support and had prolonged ICU stay.
Although all our patients received one or more types of antiviral or immunomodulator agents, we could not comment on the efficacy of one over the other agents as we have not had a standard regime and there are many confounding factors affecting mortality and survival. The selection of antiviral agents were made after joint discussion with ID physicians. Some patients received more than 1 different combinations of antiviral agents. A combination of lopinavir/ritonavir, interferon beta and hydroxychloroquine were initially used. These combinations were later switched to atazanavir and ritonavir. Patients who later developed prolonged QT on electrocardiogram (ECG) or worsening liver enzymes were subsequently withheld from antiviral therapy. The group of patients were started on corticosteroid or immunomodulator were the ones which demonstrated signs and symptoms of cytokine release syndrome (CRS) or sepsis related ARDS based on inflammatory markers and chest X-ray. Again the usage of corticosteroids and tocilizumab were compassionate and patient selection were done by ID physician and intensivists. At present, no drugs have been proven to be safe and effective at treating COVID-19 patients (7).
We practiced early proning for severe ARDS with PF ratio of <150 mmHg together with neuromuscular blockade. Similar rescue strategies has been reported by Yang et al. in Wuhan (6). Ten out of 14 of our patients who were ventilated prone managed to be extubated and discharged out of ICU.
The majority of our patients had received broad spectrum antibiotics. The threshold to initiate antibiotics were low especially for patients who were started on corticosteroids or immunomodulators as they were at high risk to develop nosocomial infections. However, most patients were often culture negative. Other co-factors that put patients at risk of cross infection include limited nursing care especially on viral filters change and endotracheal tube suctioning and presence of indwelling catheters. The initiation of antimicrobial agents was as suggested by the Society of Critical Care Medicine (SCCM) through their Surviving Sepsis Campaign COVID-19 Guidelines but with de-escalation and daily evaluation of treatment duration (8).
Our fatality rate of 18.3% out of the ventilated patients is currently lower than reported by Richardson et al. The latter reported 24.5% death among ventilated patients in New York City area (9). The initial mortality rate among ventilated critically ill in Hubei Province in China was even higher at between 81–97% (10). Our lower mortality rate might be as a results of early ICU admission and early intubation policy. Malaysia currently implementing a policy of admitting positive COVID-19 patients either to a low risk quarantine center or hospital if they exhibit symptoms. In wards, patients who needed higher oxygen requirement of more than 3 L/min will be referred for ICU care. Thus, we were able avoid catastrophic hypoxic arrest that might go unnoticed in wards. Patients who required more than 8 L/min of non-rebreather mask will be electively intubated as we did not practice applying non-invasive ventilation (NIV) for newly diagnosed COVID-19 patients.
Limitations of this study includes being in a single center within a state. However, as the state of Selangor recorded the highest number of cases, it did reflect the severity of cases in Malaysia’s worst affected region. Second, is the absence of post discharge follow up to determine patient outcome following ICU discharge.
Conclusions
This case series reflected the clinical management and outcome of ventilated critically ill COVID-19 patients in the Selangor state of Malaysia. Although the fight against COVID-19 is far from over, we have seen a plateauing of cases due to movement control order that has been ongoing nationwide. Until definite treatment or vaccination is found, we were hoping that the numbers of severe cases can be controlled and that those critically ill, can be better managed on supportive treatments.
Acknowledgments
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-82
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jeccm-20-82
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-82). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Malaysian Research and Ethics Committee (MREC) (ID: NMRR-20-2441-54853) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organisation. Q&A on Coronavirus (COVID-19). Available online: (Accessed 12 April 2020).https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
- World Health Organisation. Coronavirus disease (COVID-19) pandemic. Available online: (Accessed 12 April 2020).https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Abdullah NH. Kementerian Kesihatan Malaysia. Kenyataan Akhbar Ketua Pengarah Kesihatan Malaysia. Available online: (Accessed 12 April 2020).http://www.moh.gov.my/index.php/pages/view/2019-ncov-wuhan-kenyataan-akhbar
- Department of Statistics Malaysia, Official Portal. Available online: (Accesed 13 April 2020).https://ukkdosm.github.io/covid-19
- Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 2012;120:c179-84. [PubMed]
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475-81. [Crossref] [PubMed]
- National Institutes of Health. COVID-19 treatment guidelines. April 21, 2020. Available online: https://covid19treatmentguidelines.nih.gov/introduction/
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med 2020;46:854-87. [Crossref] [PubMed]
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020;323:2052-9. [Crossref] [PubMed]
- Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. Lancet 2020;395:1014-5. [Crossref] [PubMed]
Cite this article as: Zainol Abidin NH, Lee CK, Zakaria SA, Ramaiah Y, Hilmi ZS, Syed Maule S. Clinical course and outcomes of ventilated critically ill COVID-19 patients in Selangor state, Malaysia. J Emerg Crit Care Med 2021;5:6.


