Negative Association Between Mediterranean Diet Adherence and COVID-19 Cases and Related Deaths in Spain and 23 OECD Countries: An Ecological Study
- 1Department of Nutrition, Auburn University, Auburn, AL, United States
- 2Boshell Diabetes and Metabolic Disease Research Program, Auburn University, Auburn, AL, United States
In December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-Cov2) emerged in Wuhan, China, sparking the Coronavirus disease 2019 (COVID-19) pandemic. The high prevalence of nutrition-related COVID-19 risk factors including obesity, type 2 diabetes, and hypertension, suggests that healthy dietary approaches may mitigate COVID-19 related outcomes and possibly SARS-CoV-2 infection. Based on the fundamental role of nutrition in immune function and the well-documented association between Mediterranean diet consumption and risk reduction for chronic diseases that are comorbidities in COVID-19 patients, we hypothesized that there would be a relationship between Mediterranean diet adherence and COVID-19 cases and related deaths. In this perspective, we examined the association between regional adherence to a Mediterranean diet and COVID-19 cases and deaths using an ecological study design. We observed that Mediterranean diet adherence was negatively associated with both COVID-19 cases and related deaths across 17 regions in Spain and that the relationship remained when adjusted for factors of well-being. We also observed a negative association between Mediterranean diet adherence and COVID-19 related deaths across 23 countries when adjusted for factors of well-being and physical inactivity. The anti-inflammatory properties of the Mediterranean diet - likely due to the polyphenol content of the diet - may be a biological basis to explain our findings. However, there are confounding factors unrelated to dietary factors driving COVID-19 cases and related deaths across the regions in Spain and the 23 countries examined in our analysis. Our findings will need to be confirmed and further explored in cohort studies.
Introduction
Epidemics and pandemics have shaped the historys of humanity. Deaths from pandemics have ranged from up to half of the world's population in the Post-classical period to very few deaths in the Late Modern period (1). The Coronavirus disease 2019 (COVID-19) pandemic is just the most recent of a series of epidemics and pandemics that are arising (1) likely due to environmental pressure from the expansion of human populations (2). Increasing population density and economic development, or westernization, has not only been associated with infectious diseases, but non-communicable diseases such as obesity, cardiovascular disease, and type 2 diabetes.
Consumption of a Western diet which includes high consumption of energy dense foods, such as simple sugars and fats, contributes to the development of obesity and pathophysiological chronic inflammation (3, 4) which are risk factors for the development of chronic diseases including cardiovascular disease, type 2 diabetes, and certain forms of cancer (5). In addition, obesity is associated with immunomodulatory effects related to infectious, gastrointestinal, and respiratory diseases (6). In contrast, essential micronutrients and polyphenolic compounds which are enriched in healthy diets are anti-inflammatory and may have benefits for risk reduction of communicable and non-communicable diseases (7–9). Adherence to a traditional Mediterranean diet, a plant-based diet rich in fresh fruits and vegetables, whole grains, nuts, fish and extra virgin olive oil, can reduce the risk of cardiovascular disease, type 2 diabetes, cognitive disorders, muscle atrophy and other signs of frailty (10–12). A Mediterranean diet is also rich in fiber which modulates nutrient absorption and satiety and contributes to maintaining a healthy weight (13).
Common comorbidities in COVID-19 patients include obesity, hypertension, cardiovascular disease, type 2 diabetes, chronic obstructive pulmonary disease, chronic kidney disease, cerebrovascular disease and cancer (14–16). Increased risk of COVID-19 related death - reported in a meta-analysis of studies from China and the USA - has been observed for patients with chronic renal disease (OR, 9.4; 95% CI, 3.2–27.4), cardiovascular disease (OR, 3.8; 95% CI, 2.1–6.9), hypertension (OR, 2.5; 95% CI, 2.1–3.1), type 2 diabetes (OR, 2.0; 95% CI, 1.7–2.3) (17), and in a separate analysis obesity (OR 1.7; 95% CI, 1.1–2.8) from a cohort in the USA (18). Obesity related comorbidities that increase the severity of COVID-19 include respiratory dysfunction resulting in lower lung volume, impaired gas exchange, and increased airway resistance (19). A greater association with comorbidities and in-hospital mortality has been observed in patients in America and Europe compared to Asia (20).
Because the Mediterranean diet is a dietary approach associated with overall well-being, and Mediterranean diet consumption is associated with risk reduction for the common comorbidities observed in COVID-19 patients, we hypothesized that Mediterranean diet adherence would be negatively associated with COVID-19 cases and related deaths. The absence of dietary data in COVID-19 patients precluded a direct examination of the relationship between Mediterranean diet adherence and COVID-19 cases and related deaths. Therefore, we undertook an ecological study to examine the association between regional adherence to a Mediterranean diet and COVID-19 cases and deaths.
Ecological Analysis
To determine whether there is relationship between Mediterranean diet adherence and COVID-19 cases and deaths we first chose to examine regional data from a country with a universal healthcare system to reduce confounding factors associated other healthcare models which may lack standardization of the COVID-19 response. We also sought to examine a country for which (1) regional differences in MD adherence have been reported, (2) regional COVID-19 cases and deaths, and (3) risk-modifying factors have been reported. Based on our criteria, we examined the relationship across 17 autonomous communities (regions) of Spain between Mediterranean Adequacy Index score (21) and COVID-19 cases and deaths as of June 9, 2020 (22). In an unadjusted linear model, we observed a significant negative association between Mediterranean Adequacy Index score and COVID-19 cases (p = 0.023) and COVID-19 related deaths (p = 0.032) (Table 1). We used a multivariable linear model to adjust for social determinants of health (factors of well-being) which can influence health outcomes (23–26). The factors of well-being (income, education, housing, environment, and life satisfaction) were assessed using the Organization for Economic Co-operation and Development (OECD) Well-Being Database in the 17 regions of Spain (27). As shown in Table 1, a stronger significant negative association between Mediterranean Adequacy Index score and COVID-19 cases (r2 = 0.663) and COVID-19 related deaths (r2 = 0.729) was observed. The well-being factors of income, education, and life satisfaction added significantly (p < 0.05) to the relationship between Mediterranean Adequacy Index score and both COVID-19 cases and COVID-19 related deaths.
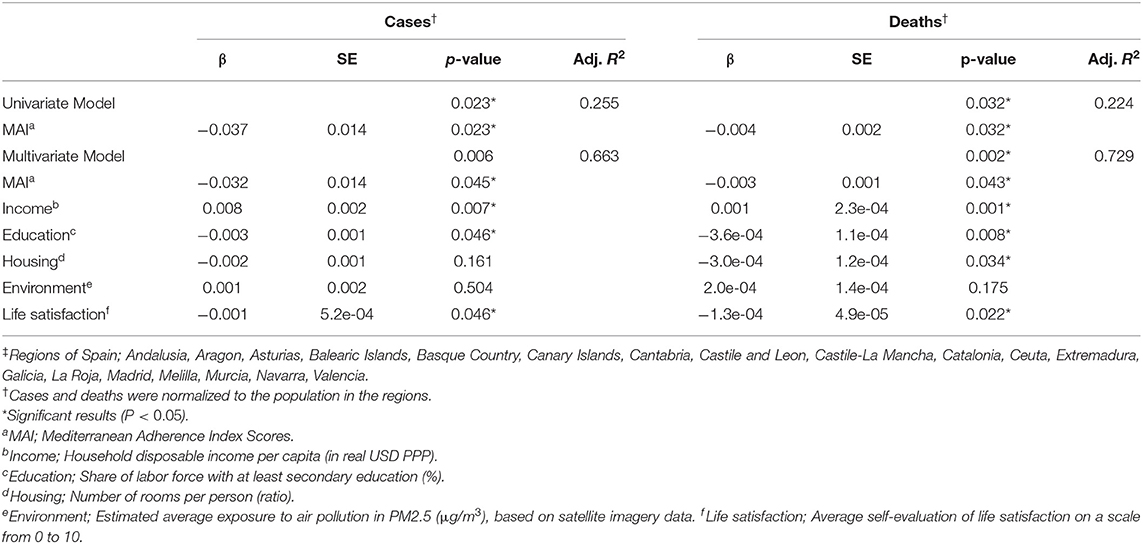
Table 1. Multivariable linear regression analysis assessing Mediterranean diet adherence and COVID-19 cases and deaths between regions in Spain‡ adjusted for well-being factors.
To further explore the relationship between Mediterranean diet adherence and COVID-19 cases and deaths, we examined Mediterranean adherence and COVID-19 cases and deaths across 23 countries in the OECD Well-Being Database for which Mediterranean Adequacy Index score (from highest to lowest: Turkey, Greece, Italy, Japan, Chile, Spain, Portugal, Israel, Finland, Norway, Iceland, United Kingdom, Ireland, France, Denmark, Sweden, Canada, Hungary, Germany, Austria, Australia, Switzerland, and United States) (28) and COVID-19 cases and deaths per million people (from highest to lowest: United Kingdom, Spain, Italy, France, Ireland, United States, Canada, Switzerland, Portugal, Chile, Germany, Denmark, Sweden, Austria, Turkey, Finland, Hungary, Norway, Israel, Iceland, Greece, Japan, and Australia) (29). As shown in Table 2, we did not observe an association between Mediterranean Adequacy Index score and COVID-19 cases or COVID-19 related deaths in an unadjusted linear model. There was also not an association between Mediterranean Adequacy Index score and COVID-19 cases when adjusted for well-being factors in the OECD Well-Being Database. However, a significant negative association between Mediterranean Adequacy Index score and COVID-19 related deaths (r2 = 0.768, p = 0.004) was observed when adjusted for well-being factors (income, education, housing, environment, and life satisfaction) in the OECD Well-Being Database and physical inactivity from the World Health Organization Global Health Observatory data repository (30). The well-being factors of education, housing, environment, and life satisfaction added significantly (p < 0.05) to the relationship between Mediterranean Adequacy Index score and COVID-19 related deaths. A sensitivity analysis was performed by removing the Mediterranean Adequacy Index score from the model. We found that the absence of the Mediterranean Adequacy Index score significantly (p < 0.01) weakened the adjusted square of the coefficient of multiple correlation from 0.768 to 0.500 (data not shown).
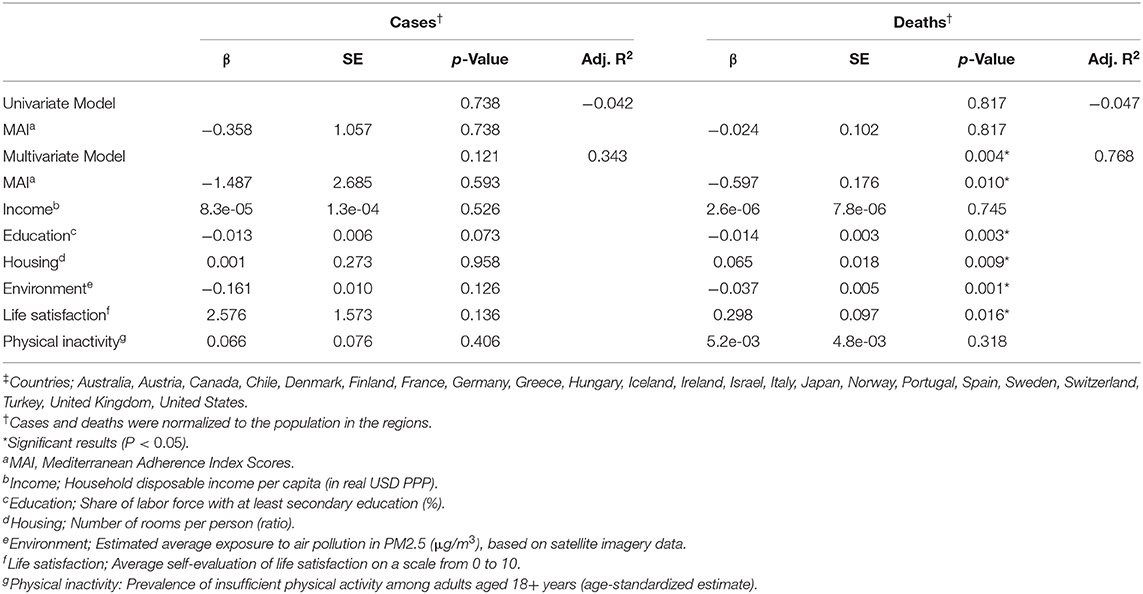
Table 2. Multivariable linear regression analysis assessing Mediterranean diet adherence and COVID-19 cases and deaths between Countries‡ adjusted for well-being factors.
In a sub-analysis of only European countries, we observed a similar significant negative association between Mediterranean Adequacy Index score and COVID-19 related deaths (r2 = 0.771, p = 0.030) when adjusted for well-being factors and physical inactivity (data not shown). We next examined whether the association between Mediterranean Adequacy Index score and COVID-19 related deaths was modified by adding country wide obesity prevalence (31) to the model adjusted for well-being factors and physical inactivity. We still observed a significant negative association (r2 = 0.751, p = 0.012) between Mediterranean Adequacy Index score and COVID-19 related deaths; however, obesity prevalence did not significantly add to the model (data not shown).
Discussion
In the current ecological study, we observed that Mediterranean diet adherence was negatively associated with both COVID-19 cases and related deaths across 17 regions in Spain. The relationship between Mediterranean diet adherence and COVID-19 cases and related deaths remained when adjusted for factors of well-being. We then examined the relationship between Mediterranean diet adherence and COVID-19 cases and related deaths across 23 countries for which data was available for Mediterranean diet adherence, COVID-19 cases and deaths, and factors of well-being. In the models adjusted for factors of well-being and physical inactivity we observed a negative association between Mediterranean diet adherence and COVID-19 related deaths. Our findings that the socioeconomic factors of income and education added significantly to our models is consistent with prior work that income and education are significant factors in viral infection related hospitalization (32–35) and Mediterranean diet adherence (23, 36–40). The finding that life satisfaction added significantly to the adjusted models is consistent with epidemiological evidence linking life satisfaction to risk of chronic disease and mortality (41–43). It is important to note that our findings with COVID-19 cases and deaths pre-dated use and approval of medical treatments known to reduce mortality such as dexamethasone and remdesivir (44).
In the analysis of the 23 OECD countries we observed that the United States and the United Kingdom had the 1st and 11th lowest Mediterranean diet adherence, respectively, and the 6th and 1st highest COVID-19 related deaths per million, respectively. In contrast, Italy and Spain were outliers in the association between Mediterranean diet adherence and COVID-19 related deaths in the 25 OECD countries. Italy and Spain had the 3rd and 6th highest in Mediterranean Adequacy Index score, respectively, yet high COVID-19 mortality (3rd and 2nd highest in deaths per million people, respectively). Italy and Spain along with China, Iran, Germany, France, South Korea, and Japan were the eight earliest majorly effected countries in the COVID-19 pandemic. The doubling time of COVID-19 cases in Italy during the first and second 3-week interval was greatest among the eight countries while the growth rate of COVID-19 cases from the first to second 3-week interval in Spain was greatest among the eight countries (45). Whether poor early containment was a factor in the high COVID-19 death rate is not known. Factors ranging from socio-cultural to health systems likely have contributed to the high COVID-19 death rate in Italy and Spain (46–48). Interestingly, Lombardy, Italy, a region in northern Italy which has low Mediterranean diet adherence compared to southern Italy (38, 49, 50), was the epicenter of COVID-19 cases in Europe.
The current study design does not allow for causative conclusions to be reached on our findings. However, there is a biological basis for our findings. Severe complications of COVID-19 include acute respiratory distress syndrome and death. In the subset of patients with severe complications, a hyper inflammation (a.k.a. the cytokine storm) state is observed (51) possibility due to a dysregulated macrophage response (52). It has been proposed that comorbidities including obesity, type 2 diabetes, cardiovascular disease, and hypertension contribute to the inflammation response leading to severe complications of COVID-19 (53).
Adherence to plant-based dietary approaches, including the Mediterranean diet, are associated with a reduction in the risk of developing major chronic diseases including the COVID-19 comorbidities of obesity, type 2 diabetes, cardiovascular disease, and hypertension (54–59). Low-grade chronic inflammation underlies the COVID-19 comorbidities (60). Importantly, consumption of a Mediterranean diet is associated with a reduction in the inflammation, coagulation, and endothelial dysfunction markers including c-reactive protein (CRP), interleukin 6 (IL-6), fibrinogen, homocysteine, and E-selectin (61–63) which is consistent with findings of a reduction in inflammation markers across plant-based diet consumption (64). An assessment of overall inflammatory potential of a diet, the dietary inflammatory index (DII) (65, 66) has been shown to link dietary inflammation to communicable disease and inflammation-related disease. A high DII has been reported to be associated with higher risk for stomach and intestinal illness (67) and with increased systemic inflammation and lower lung function (68). Importantly, a high DII is associated with low grade inflammation and low Mediterranean diet score (69). It has been proposed that the anti-inflammatory properties of the Mediterranean diet are due to the high polyphenol content (70–72) from fruits, vegetables and extra virgin olive oil (73). In the SUN cohort, participants with the highest Mediterranean diet adherence and polyphenol intake of flavonoids had a significantly lower incidence of cardiovascular disease events compared to participants with the lowest Mediterranean diet adherence and polyphenol intake of flavonoids (74). Consistent with these findings, it was observed in high cardiovascular disease risk patients in the PREDIMED study that the greatest reduction in plasma levels of inflammatory markers occurred in participants with the highest urinary total polyphenols (75). It should be noted that the PREDIMED study did not have full randomization to the Mediterranean diet treatment groups (76).
There are limitations to the current study. Importantly, the ecological design of the current study does not allow for direct examination of the relationship between Mediterranean diet adherence and COVID-19 cases and related deaths. The observational methodology used may be a source of errors that could lead to wrong conclusions on the association between Mediterranean diet adherence and COVID-19 cases and related deaths. Thus, causation cannot be inferred from these findings. Additionally, the possible age effect of each group (the habits and behaviors of each stage of life are different) and the period effect (events that occur over time that affect all age groups and can alter the association) are limitations. Further, the Mediterranean diet adherence data may not reflect current dietary patterns in the regions of Spain and the OECD countries examined. Even though Mediterranean diet adherence has declined in Spain and other OECD countries in the Mediterranean Sea basin compared to historical data from the 1960s, it has stabilized in the past decades (21, 28). In addition, Mediterranean diet adherence assessed at two time points in the past two decades highly correlates across countries (r2 = 0.969, p < 0.001) (data not shown). We acknowledge that there are confounding factors related to societal norms, cultural factors, and the governmental response to the COVID-19 pandemic and differences in health care systems across countries that may influence COVID-19 cases and deaths in Spain and the countries examined in the current study. As the COVID-19 pandemic continues our findings represent a snapshot in time of the pandemic.
Even though our findings suggest a negative relationship between Mediterranean diet adherence and COVID-19 cases and related deaths, further studies are required to examine whether Mediterranean diet consumption reduces the risk of COVID-19 and/or chronic disease risk reduction associated with Mediterranean diet consumption reduces the risk of COVID-19 death. In conclusion, the Mediterranean diet and other dietary approaches that reduce inflammation and risk for chronic disease might reduce the risk for severe COVID-19 pathology and mortality.
Data Availability Statement
The datasets generated for this study can be obtained from the corresponding author (mwgreene@auburn.edu).
Author Contributions
MG conceived of the work, performed data and statistical analysis, contributed to the writing, and offered critical comments. AR performed data analysis, wrote the first draft of the manuscript, and provided critical revisions to the content. AF provided critical revisions to the content. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Alabama Agricultural Experiment Station and the Hatch program of the National Institute of Food and Agriculture, U.S. Department of Agriculture (Project number ALA044-1-18037) (MG).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Morens DM, Daszak P, Markel H, Taubenberger JK. Pandemic COVID-19 joins history's pandemic legion. Mbio. (2020) 11:e00812–20. doi: 10.1128/mBio.00812-20
2. Di Marco M, Baker ML, Daszak P, De Barro P, Eskew EA, Godde CM, et al. Opinion: sustainable development must account for pandemic risk. Proc Natl Acad Sci USA. (2020) 117:3888–92. doi: 10.1073/pnas.2001655117
3. de Heredia FP, Gómez-Martínez S, Marcos A. Obesity, inflammation and the immune system. Proc Nutr Soc. (2012) 71:332–8. doi: 10.1017/S0029665112000092
4. Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. (2007) 132:2169–80. doi: 10.1053/j.gastro.2007.03.059
5. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC public health. (2009) 9:88. doi: 10.1186/1471-2458-9-88
6. Myles IA. Fast food fever: reviewing the impacts of the Western diet on immunity. Nutr J. (2014) 13:1–17. doi: 10.1186/1475-2891-13-61
7. Farhadi S, Ovchinnikov RS. The relationship between nutrition and infectious diseases: a review. Biomed Biotechnol Res J. (2018) 2:168. doi: 10.4103/bbrj.bbrj_69_18
8. Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune System–Working in harmony to reduce the risk of infection. Nutrients. (2020) 12:236. doi: 10.3390/nu12010236
9. González-Gallego J, García-Mediavilla MV, Sánchez-Campos S, Tuñón MJ. Fruit polyphenols, immunity and inflammation. Br J Nutr. (2010) 104:S15–27. doi: 10.1017/S0007114510003910
10. Romagnolo DF, Selmin OI. Mediterranean diet and prevention of chronic diseases. Nutr Today. (2017) 52:208. doi: 10.1097/NT.0000000000000228
11. Sánchez-Sánchez ML, García-Vigara A, Hidalgo-Mora JJ, García-Pérez M, Tarín J, Cano A. Mediterranean diet and health: a systematic review of epidemiological studies and intervention trials. Maturitas. (2020) 136:25–37. doi: 10.1016/j.maturitas.2020.03.008
12. Tosti V, Bertozzi B, Fontana L. Health benefits of the Mediterranean diet: metabolic and molecular mechanisms. J Gerontol A Biol Sci Med Sci. (2018) 73:318–26. doi: 10.1093/gerona/glx227
13. Chen J-P, Chen G-C, Wang X-P, Qin L, Bai Y. Dietary fiber and metabolic syndrome: a meta-analysis and review of related mechanisms. Nutrients. (2018) 10:24. doi: 10.3390/nu10010024
14. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. (2020) 323:2052–9. doi: 10.1001/jama.2020.6775
15. Singh AK, Gillies CL, Singh R, Singh A, Chudasama Y, Coles B, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab. (2020) 22:1915–24. doi: 10.1111/dom.14124
16. Onder G, Rezza G, Brusaferro S. Case-Fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
17. Tian W, Jiang W, Yao J, Nicholson CJ, Li RH, Sigurslid HH, et al. Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol. (2020) 92:1875–83. doi: 10.1002/jmv.26050
18. Pettit NN, MacKenzie EL, Ridgway J, Pursell K, Ash D, Patel B, et al. Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19. Obesity. (2020) 28:1806–10. doi: 10.1002/oby.22941
19. Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. (2020) 16:341–2. doi: 10.1038/s41574-020-0364-6
20. Goel S, Jain T, Hooda A, Malhotra R, Johal G, Masoomi R, et al. Clinical characteristics and in-hospital mortality for COVID-19 across the globe. Cardiol Therapy. (2020) 9:553–9. doi: 10.1007/s40119-020-00189-0
21. Bach-Faig A, Fuentes-Bol C, Ramos D, Carrasco JL, Roman B, Bertomeu IF, et al. The Mediterranean diet in spain: adherence trends during the past two decades using the mediterranean adequacy index. Public Health Nutr. (2011) 14:622–8. doi: 10.1017/S1368980010002752
23. Lowcock EC, Rosella LC, Foisy J, McGeer A, Crowcroft N. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health. (2012) 102:e51–8. doi: 10.2105/AJPH.2012.300814
24. Wong CM, Yang L, Thach TQ, Chau PYK, Chan KP, Thomas GN, et al. Modification by influenza on health effects of air pollution in Hong Kong. Environ Health Perspect. (2009) 117:248–53. doi: 10.1289/ehp.11605
25. Cordoba E, Aiello AE. Social determinants of influenza illness and outbreaks in the United States. North Carolina Med J. (2016) 77:341–5. doi: 10.18043/ncm.77.5.341
26. Marmot M. Social determinants of health inequalities. Lancet. (2005) 365:1099–04. doi: 10.1016/S0140-6736(05)71146-6
27. Regional well-being (Edition 2016) (2016). Available from: https://www.oecd-ilibrary.org/content/data/d147c81c-en (accessed January 13, 2021).
28. Vilarnau C, Stracker DM, Funtikov A, da Silva R, Estruch R, Bach-Faig A. Worldwide adherence to mediterranean diet between 1960 and 2011. Eur J Clin Nutr. (2019) 72:83–91. doi: 10.1038/s41430-018-0313-9
29. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Geneva: World Health Organization (2020).
30. Global Health Observatory Data Repository. World Health Organization (2021). Available from: https://apps.who.int/gho/data/node.main.A893?lang=en (accessed January 16, 2021).
31. Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
32. Chandrasekhar R, Sloan C, Mitchel E, Ndi D, Alden N, Thomas A, et al. Social determinants of influenza hospitalization in the United States. Influenza Other Respir Viruses. (2017) 11:479–88. doi: 10.1111/irv.12483
33. Brownstein JS, Pena BG, Mandl KD. Characterizing socioeconomic disparities in the burden of influenza and RSV using surveillance data. Adv Dis Surveill. (2007) 2:94.
34. González-Candelas F, Astray J, Alonso J, Castro A, Cantón R, Galán JC, et al. Sociodemographic Factors and Clinical Conditions Associated to Hospitalization in Influenza A (H1N1) 2009 Virus Infected Patients in Spain, 2009–2010. PLoS ONE. (2012) 7:e33139. doi: 10.1371/journal.pone.0033139
35. Levy NS, Nguyen TQ, Westheimer E, Layton M. Disparities in the severity of influenza illness: a descriptive study of hospitalized and nonhospitalized novel H1N1 influenza–positive patients in New York City 2009–2010 Influenza Season. J Public Health Manag Pract. (2013) 19:16–24. doi: 10.1097/PHH.0b013e31824155a2
36. Cavaliere A, De Marchi E, Banterle A. Exploring the adherence to the Mediterranean diet and its relationship with individual lifestyle: the role of healthy behaviors, pro-environmental behaviors, income, and education. Nutrients. (2018) 10:141. doi: 10.3390/nu10020141
37. Knight CJ, Jackson O, Rahman I, Burnett DO, Frugé AD, Greene MW. The Mediterranean diet in the Stroke Belt: a cross-sectional study on adherence and perceived knowledge, barriers, and benefits. Nutrients. (2019) 11:1847. doi: 10.3390/nu11081847
38. Ruggiero E, Di Castelnuovo A, Costanzo S, Persichillo M, Bracone F, Cerletti C, et al. Socioeconomic and psychosocial determinants of adherence to the Mediterranean diet in a general adult Italian population. Eur J Public Health. (2019) 29:328–35. doi: 10.1093/eurpub/cky127
39. Tong TY, Imamura F, Monsivais P, Brage S, Griffin SJ, Wareham NJ, et al. Dietary cost associated with adherence to the Mediterranean diet, and its variation by socio-economic factors in the UK Fenland Study. Br J Nutr. (2018) 119:685–94. doi: 10.1017/S0007114517003993
40. Rodrigues S, Caraher M, Trichopoulou A, De Almeida M. Portuguese households' diet quality (adherence to Mediterranean food pattern and compliance with WHO population dietary goals): trends, regional disparities and socioeconomic determinants. Eur J Clin Nutr. (2008) 62:1263–72. doi: 10.1038/sj.ejcn.1602852
41. Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy finnish adults. Am J Epidemiol. (2000) 152:983–91. doi: 10.1093/aje/152.10.983
42. Diener E, Chan MY. Happy people live longer: subjective well-being contributes to health and longevity. Appl Psychol Health Well-Being. (2011) 3:1–43. doi: 10.1111/j.1758-0854.2010.01045.x
43. Rosella LC, Fu L, Buajitti E, Goel V. Death and chronic disease risk associated with poor life satisfaction: a population-based cohort study. Am J Epidemiol. (2018) 188:323–31. doi: 10.1093/aje/kwy245
44. World Health Organization. Clinical Management of COVID-19: Interim Guidance. Geneva: World Health Organization (2020).
45. Khosrawipour V, Lau H, Khosrawipour T, Kocbach P, Ichii H, Bania J, et al. Failure in initial stage containment of global COVID-19 epicenters. J Med Virol. (2020) 92:863–7. doi: 10.1002/jmv.25883
46. Degiuli F. Caring for a Living: Migrant Women, Aging Citizens, and Italian Families. New York, NY: Oxford University Press (2016).
47. Legido-Quigley H, Mateos-García JT, Campos VR, Gea-Sánchez M, Muntaner C, McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. lancet Public Health. (2020) 5:e251–2. doi: 10.1016/S2468-2667(20)30060-8
48. Armocida B, Formenti B, Ussai S, Palestra F, Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. (2020) 5:e253. doi: 10.1016/S2468-2667(20)30074-8
49. Noale M, Nardi M, Limongi F, Siviero P, Caregaro L, Crepaldi G, et al. Adolescents in southern regions of Italy adhere to the Mediterranean diet more than those in the northern regions. Nutr Res. (2014) 34:771–9. doi: 10.1016/j.nutres.2014.08.001
50. Pelucchi C, Galeone C, Negri E, La Vecchia C. Trends in adherence to the Mediterranean diet in an Italian population between 1991 and 2006. Eur J Clin Nutr. (2010) 64:1052–6. doi: 10.1038/ejcn.2010.158
51. Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. (2020) 20:363–74. doi: 10.1038/s41577-020-0311-8
52. Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. (2020) 20:355–62. doi: 10.1038/s41577-020-0331-4
53. de Lucena TMC, da Silva Santos AF, de Lima Fabrício BR, de Albuquerque Borborema ME, de Azevêdo Silva J. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes Metab Syndr Clin Res Rev. (2020) 14:597–600. doi: 10.1016/j.dsx.2020.05.025
54. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. (2010) 92:1189–96. doi: 10.3945/ajcn.2010.29673
55. Estruch R, Ros E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev Endocr Metab Disord. (2020) 21:315–27. doi: 10.1007/s11154-020-09579-0
56. Salas-Salvadó J, Becerra-Tomás N, Papandreou C, Bulló M. Dietary patterns emphasizing the consumption of plant foods in the management of type 2 diabetes: a narrative review. Adv Nutr. (2019) 10:S320–31. doi: 10.1093/advances/nmy102
57. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. (2015) 31:350–8. doi: 10.1016/j.nut.2014.09.002
58. Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: a randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. (2017) 7:e256. doi: 10.1038/nutd.2017.3
59. Buckland G, Bach A, Serra-Majem L. Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev. (2008) 9:582–93. doi: 10.1111/j.1467-789X.2008.00503.x
60. Scrivo R, Vasile M, Bartosiewicz I, Valesini G. Inflammation as “common soil” of the multifactorial diseases. Autoimmun Rev. (2011) 10:369–74. doi: 10.1016/j.autrev.2010.12.006
61. Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: the ATTICA study. J Am Coll Cardiol. (2004) 44:152–8. doi: 10.1016/j.jacc.2004.03.039
62. Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Int Med. (2006) 145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004
63. Fung TT, McCullough ML, Newby P, Manson JE, Meigs JB, Rifai N, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. (2005) 82:163–73. doi: 10.1093/ajcn/82.1.163
64. Eichelmann F, Schwingshackl L, Fedirko V, Aleksandrova K. Effect of plant-based diets on obesity-related inflammatory profiles: a systematic review and meta-analysis of intervention trials. Obes Rev. (2016) 17:1067–79. doi: 10.1111/obr.12439
65. Cavicchia PP, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A new dietary inflammatory index predicts interval changes in serum high-sensitivity c-reactive protein. J Nutr. (2009) 139:2365–72. doi: 10.3945/jn.109.114025
66. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. (2013) 17:1689–96. doi: 10.1017/S1368980013002115
67. Wirth MD, Robinson C, Murphy EA, Shivappa N, Hébert JR. The dietary inflammatory index is associated with gastrointestinal infection symptoms in the national health and nutrition examination survey. Int J Food Sci Nutr. (2020) 71:106–15. doi: 10.1080/09637486.2019.1614539
68. Wood LG, Shivappa N, Berthon BS, Gibson PG, Hebert JR. Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy. (2015) 45:177–83. doi: 10.1111/cea.12323
69. Shivappa N, Bonaccio M, Hebert JR, Di Castelnuovo A, Costanzo S, Ruggiero E, et al. Association of proinflammatory diet with low-grade inflammation: results from the moli-sani study. Nutrition. (2018) 54:182–8. doi: 10.1016/j.nut.2018.04.004
70. Razquin C, Martinez-Gonzalez MA. A traditional Mediterranean diet effectively reduces inflammation and improves cardiovascular health. Nutrients. (2019) 11:1842. doi: 10.3390/nu11081842
71. Bonaccio M, Pounis G, Cerletti C, Donati MB, Iacoviello L, de Gaetano G. Mediterranean diet, dietary polyphenols and low grade inflammation: results from the moli-sani study. Br J Clin Pharmacol. (2017) 83:107–13. doi: 10.1111/bcp.12924
72. Finicelli M, Squillaro T, Di Cristo F, Di Salle A, Melone MAB, Galderisi U, et al. Metabolic syndrome, Mediterranean diet, and polyphenols: evidence and perspectives. J Cell Physiol. (2019) 234:5807–26. doi: 10.1002/jcp.27506
73. Martínez-González MA, Salas-Salvadó J, Estruch R, Corella D, Fitó M, Ros E, et al. Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis. (2015) 58:50–60. doi: 10.1016/j.pcad.2015.04.003
74. Mendonça RD, Carvalho NC, Martin-Moreno JM, Pimenta AM, Lopes ACS, Gea A, et al. Total polyphenol intake, polyphenol subtypes and incidence of cardiovascular disease: the SUN cohort study. Nutr Metab Cardiovasc Dis. (2019) 29:69–78. doi: 10.1016/j.numecd.2018.09.012
75. Medina-Remón A, Casas R, Tressserra-Rimbau A, Ros E, Martínez-González MA, Fitó M, et al. Polyphenol intake from a Mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a substudy of the PREDIMED trial. Br J Clin Pharmacol. (2017) 83:114–28. doi: 10.1111/bcp.12986
Keywords: COVID-19, mediterranean diet, coronavirus, chronic disease, healthy diet, pandemic
Citation: Greene MW, Roberts AP and Frugé AD (2021) Negative Association Between Mediterranean Diet Adherence and COVID-19 Cases and Related Deaths in Spain and 23 OECD Countries: An Ecological Study. Front. Nutr. 8:591964. doi: 10.3389/fnut.2021.591964
Received: 05 August 2020; Accepted: 10 February 2021;
Published: 05 March 2021.
Edited by:
Alexandros Tsoupras, University of Limerick, IrelandReviewed by:
Jose Paulo Andrade, Universidade do Porto, PortugalRosa Casas Rodriguez, Institut de Recerca Biomèdica August Pi i Sunyer (IDIBAPS), Spain
Copyright © 2021 Greene, Roberts and Frugé. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael W. Greene, mwg0006@auburn.edu
 Michael W. Greene
Michael W. Greene Alexis P. Roberts
Alexis P. Roberts Andrew D. Frugé
Andrew D. Frugé