Abstract
Background
COVID-19 disease affects the nervous system and led to an increase in neurological consults for patients at admission and through the period of hospitalization during the peak of the pandemic.
Methods
Patients with clinical and laboratory diagnosis of COVID-19 that required a neurologic consultation or those who presented with neurological problems on admission that led to a diagnosis of SARS-CoV-2 infection during a 2-month period at the peak of the pandemic were included in this study. Demographic and clinical variables were analyzed.
Results
Thirty-five patients were included. The presenting neurologic manifestations on admission led to the diagnosis of COVID-19 in 14 patients (40%). The most common reasons for consultation during the hospitalization period were stroke (11), encephalopathy (7), seizures (6), and neuropathies (5) followed by a miscellaneous of syncope (2), migraine (1), anosmia (1), critical illness myopathy (1), and exacerbation of residual dysarthria (1). The most common neurological disturbances were associated with severe disease except for neuropathies. Patients with encephalopathies and seizures had markedly increased D-dimer and ferritin values, even higher than stroke patients. RT-PCR was performed in 8 CSF samples and was negative in all of them.
Conclusion
Neurological disturbances represent a significant and severe burden in COVID-19 patients, and they can be the presenting condition that leads to the diagnosis of the viral infection in a high percentage of patients. Evidence of direct viral mechanisms was scarce, but the pathogenesis of the diverse manifestations remains enigmatic.
Similar content being viewed by others
Introduction
Neurological disturbances are an increasingly recognized part of the clinical spectrum of COVID-19 [1,2,3,4,5,6,7,8,9,10,11]. This has represented a diagnostic and therapeutic challenge for the attending neurologist, particularly if one considers the difficulties in performing routine ancillary examinations in these patients in isolation with such a contagious condition.
The frequency and variety of neurological disorders vary significantly depending on whether they are collected in patients admitted with moderate to severe pulmonary disease or in critically ill patients in an ICU setting and on whether data collection is retrospective or prospective. Clinical information so far derives mainly from series of respiratory patients in whom neurological problems may have been missed or underestimated as well as from case reports that do not allow an accurate estimate of the extent and description of these neurological disturbances.
Our center is a tertiary hospital that serves an area that has reported over 2000 cases of COVID-19 from March 6 to May 15, 2020 (our study period). Our neurology department provided primary assistance to all COVID-19 patients during the peak of pandemic and provided neurological consults as requested. To offer a different but complementary perspective on the neurological spectrum of SARS-CoV-2 infection, we have analyzed the reasons for neurological consults during the peak of infection in an area highly impacted by this pandemic.
Methods
This was a cross-sectional study with prospective data collection, carried out between March 6 and May 15, 2020, in which all patients who presented with or developed a neurological disorder and were diagnosed with COVID-19 were seen in consult and included and analyzed in this study. Six attending neurologists and 4 late-stage neurology residents provided the standardized data for the study. We included patients hospitalized in the general medicine wards as well as in the intensive care unit (ICU) setting. Although our protocol did not recall patients after discharge, we also consulted on patients that returned on their own to the hospital, and these were, as well, included in the study.
Variable collection
We collected the following variables:
-
a)
Demographics (age, sex, admission date, date of disease onset).
-
b)
Pulmonary disease severity according to the CURB-65 scoring system. This is a yes/no 6-point scale that evaluates confusion, BUN > 19 mg/dl, respiratory rate ≥ 30, systolic blood pressure < 90 mmHg or diastolic ≤ 60 mmHg, and age ≥ 65. Patients scoring 0–1 were classified as low risk and those scoring 2–5 as a moderate to high risk.
-
c)
Cardiovascular comorbidities, including hypertension, dyslipidemia, diabetes mellitus, tobacco use, obesity (BMI > 30), atrial fibrillation, and ischemic cardiopathy.
-
d)
Pulmonary comorbidities, including chronic obstructive pulmonary disease (COPD), asthma, and obstructive sleep apnea syndrome (OSAS).
-
e)
Neurological comorbidities.
-
f)
Reason for hospitalization, with particular emphasis on whether it was a neurological problem.
-
g)
Reason for neurological consultation in case the patient presented with or was hospitalized for a non-neurological condition.
-
h)
Neurological symptoms associated with COVID-19 and different from the reason for consultation, such as anosmia, headache, and myalgia.
-
i)
Laboratory parameters pertinent to the patient’s condition, including blood and cerebrospinal fluid (CSF) when indicated.
-
j)
Laboratory parameters: serum creatinine, transaminases, creatin kinase, C-reactive protein (CRP, coagulation parameters (International Normalized Ratio (INR), aPTT), D-dimer, ferritin, and platelet count.
Inclusion criteria
Patients were eligible if they had a positive reverse transcriptase polymerase chain reaction (RT-PCR) assay for SARS-CoV-2 in a nasopharyngeal swab (using an Xpert©Xpress SARS-CoV-2 kit; Cepheid) or a chest X-ray or CT scan showing the characteristic bilateral interstitial pneumonia of COVID-19. Cerebrospinal fluids (CSF) obtained from some patients for clinical or diagnostic purposes were also tested for the presence of SARS-Cov-2 using the same RT-PCR assay as above.
Patients either had a neurological disorder as the presenting condition that required hospitalization or developed a neurological disorder after admission for COVID-19 pneumonia or after hospital discharge when 3 patients returned to the hospital on their own.
COVID-19 influence on stroke incidence
An important question frequently asked is whether the COVID-19 pandemic has resulted in a higher incidence of stroke or in a higher stroke severity. To this end, we compared the number of patients admitted to our center in the same period of 2019, as well as their severity as measured by the National Institute of Health Stroke Score (NIHSS).
Data analysis
The description of the variables was carried out using frequency tables, means and standard deviations (SD), or median and interquartile range (IQR). Patients’ characteristics and analytical parameters were compared according to the most common neurological consultation groups. The Chi-square or Fisher’s exact tests were used for the comparison of categorical variables and the non-parametric Kruskal-Wallis test for the comparison of quantitative variables. A result was considered statistically significant at p < 0.05. All statistical analyses were performed with SAS for Windows statistical software, version 9.2 (SAS Institute, Inc., Cary, NC).
The study was approved by the Ethics Committee of the Basque Country. This study was considered exempt from informed consent because it was anonymous and only reported results derived from the medical care of the patient.
Results
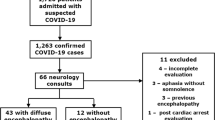
Frequency and type of neurological manifestations
A total of 35 patients were included during the study period with a median age of 66 years (range, 20–93) and a clear male predominance (71%). The clinical and demographics data are shown in Table 1. The diagnosis of SARS-CoV-2 infection was made by pulmonary imaging (Rx or CT scan) in 7 patients and nasopharyngeal RT-PCR plus imaging in 28. There were no significant differences in the means of diagnosis across groups.
Nineteen patients had been hospitalized for COVID-19 pneumonia and developed neurological problems during the period of hospitalization; 14 patients presented with a neurological disorder on admission which led to the diagnosis of COVID-19. Two patients consulted for a neurological complaint after discharge for COVID-19 (mild infection without pneumonia) and returned to the hospital on their own (1 anosmia and 1 peripheral neuropathy).
Thirty-one patients had radiologic evidence of SARS-CoV-2 pneumonia, and 4 patients had SARS-CoV-2 infection without pneumonia. Seventy-four percent (26/35) of the patients had a prior history of cardiovascular risk factors, particularly hypertension, 26% (9/35) had cardiovascular comorbidities, and 23% (8/35) had pulmonary comorbidities. Forty percent (14/35) had some neurological comorbidity.
Table 2 shows the neurological disorders that led to a neurological consultation, and whether they were the reason for admission or developed during hospitalization. The single most frequent reason was stroke (11 patients; the reason for admission in 4 patients and developed during the hospitalization period in 7 patients).
Of the 11 stroke patients, 8 had large vessel occlusion (5 middle cerebral artery, 2 carotid artery, and 2 vertebrobasilar system). Two patients presented a lacunar syndrome with a normal brain CT scan (MRI was not performed), and 1 patient had an arterial hemorrhage in the left cerebral hemisphere. There were no TIA cases. Two stroke patients died during hospitalization, both with a large vessel anterior circulation ischemic stroke. Four patients were subjected to mechanical thrombectomy with complete recanalization; 2 of them showed a significant improvement with a decrease > 4 points in the NIHSS, 1 without improvement (futile recanalization), and 1 without improvement due to a hemorrhagic transformation (vertebrobasilar stroke).
Encephalopathy (7 patients, defined as impaired attention and arousal, presenting with confusion, lethargy, delirium, or coma) followed in frequency and developed while the patients were hospitalized. All had a compromised respiratory function with hypoxemia, and 4 had a moderate increase in liver enzymes. One patient developed a refractory motor focal status epilepticus and finally died. The rest of the patients improved upon the restoration of their respiratory function.
Seizures developed in 6 patients and in 2 of them led to the diagnosis of COVID-19. All were de novo seizures except for 1 patient with a hypothalamic hamartoma and refractory gelastic seizures; he was in a poor previous condition, was institutionalized, and ultimately died from respiratory failure. Two patients had generalized tonic-clonic seizures that were controlled with IV levetiracetam. One patient had a non-convulsive status epilepticus (frontal origin) that resolved with an IV combination of levetiracetam and valproate. One patient with motor focal seizures died due to respiratory insufficiency. One patient had one episode consistent with seizures that did not require therapy and did not recur.
A brain CT scan was performed in all encephalopathy and seizure patients without any relevant findings.
Cranial or peripheral neuropathy was the reason for admission in 5 patients (14%), one of them with bilateral facial palsy. One patient with acute inflammatory demyelinating disease (AIDP) improved with IV immunoglobulin therapy. One patient with facial diplegia improved spontaneously as did one patient with VI nerve and another with VII nerve palsy.
Less common reasons for consultation developed during admission and included 2 non-convulsive syncope, 1 severe migraine attack in a migraineur, 1 isolated anosmia, 1 critical illness myopathy, and exacerbation of residual dysarthria in a patient with a history of stroke.
Ten patients were hospitalized in the ICU: 3 ischemic stroke patients (2 large vessel anterior circulation and 1 vertebrobasilar with hemorrhagic transformation after mechanical thrombectomy), 1 patient with status epilepticus, 5 encephalopathies, and 1 patient with critically illness myopathy.
Associations between clinical manifestations and variables of the study (Table 3)
Male gender predominated except for neuropathies. Stroke patients were significantly older, with a median age of 77, in comparison with 64 of seizure patients, 65 of encephalopathy, and 55 of neuropathy patients (p = 0.0033). Cardiovascular risk factors and cardiovascular and pulmonary comorbidities were particularly frequent among patients with stroke, seizures, and encephalopathy and less so in neuropathy patients with no statistically significant differences among groups (p = 0.1521).
There was a lag between COVID-19 onset and the development of neurological complications that ranged from a median of 9 days (stroke) to 17 days (seizures).
As for disease severity, peripheral neuropathies occurred in patients with past or mild infection, whereas stroke, seizures, and encephalopathies developed in patients with SARS-CoV-2 pneumonia without statistically significant between-group differences in the CURB-65 score (p = 0.1756).
Some patients had more than one neurological complication: 3 of 10 stroke patients and 5 of 8 with seizures developed encephalopathy throughout the period of hospitalization, and 2 of 7 patients who presented with encephalopathy developed seizures during admission.
Among other neurological symptoms now typically associated with COVID-19, 6 patients also had anosmia, 4 migraines (3 of whom were prior migraineurs), and 4 myalgias. These were not the reason for consultation, except for 1 patient with anosmia.
Associations of laboratory values with clinical conditions
The evaluation of analytical parameters revealed an increase in CRP in all groups, particularly in stroke patients (Table 4). Another inflammatory marker, ferritin, was particularly increased in encephalopathy patients (median value of 1101 ng/ml) and less so in stroke (481 ng/ml) and seizure (949 ng/ml) patients; it was normal in neuropathy patients (137 ng/ml). Interestingly, D-dimer was increased in encephalopathy (median value 6170 ng/ml) patients at a higher level than in stroke (2400 ng/ml) or seizure (2100 ng/ml) patients; it was only slightly increased in patients with neuropathy (725 ng/ml). The coagulation parameters were within normal limits, including stroke patients. None of these parameters reached a between-group statistically significant difference.
An increase in creatinine levels was present in 2 stroke patients, 3 seizures, and 3 encephalopathies. Mild hypertransaminemia (less than three times normal) was present in 2 stroke patients, 4 seizures, 4 encephalopathies, and 2 neuropathies. Increased CK levels were present in 1 stroke, 1 seizure, 2 encephalopathies, and 1 neuropathy.
RT-PCR was performed in 8 CSF samples and was negative in all: 5 seizures, 1 syncope, 1 encephalopathy, and 1 patient with facial diplegia.
The influence of COVID-19 on stroke incidence and severity
During the same period of the study in 2019, a total of 123 stroke patients were admitted to our department, in contrast to 87 patients in 2020 (Table 5). The mean age was slightly higher in 2019 (74.53 vs. 72.31 years, p = 0.24), and stroke severity was significantly lower in 2019 (NIHSS 4.8 vs. 7.0, p = 0.027). The severity of the 11 strokes during the pandemic was not different from that of the total of patients admitted in the same period of 2020 (Table 5).
Discussion
Our study shows that neurological disturbances are a prominent part of the spectrum of COVID-19, a primarily pulmonary disease. The mortality in our series was 11.4% (4/35, 2 from stroke, 1 with encephalopathy, and 1 from a seizure) which underscores the seriousness of COVID-19 disease.
The main reasons for neurological consultation during the COVID-19 pandemic were stroke, seizures, encephalopathy, and neuropathies, in that order. The first three entities developed in patients with severe disease whereas neuropathies did not. These diverse neurological manifestations reflect the ability of the SARS-CoV-2 virus to involve both the central and the peripheral nervous system.
The apparently low number of neurological consultations during the initial pandemic wave may have reflected an underestimation of the neurological abnormalities in severely compromised respiratory patients. A systematic neurologic evaluation of a series of unselected, consecutively hospitalized patients in our center showed a high frequency of neurological disturbances [8].
In the absence of evidence of direct infection of neural cells by SARS-CoV-2, and the general lack of expression of the ACE2 receptor in cells of the nervous system, the logical conclusion is that there are indirect disease-causing mechanisms at play in this infection. This is consistent with the lack of specific viral changes in the brain of 2 recent series of autopsies [12, 13]. The neurological manifestations appeared after a period from COVID-19 onset of 10 to 17 days (median), which also suggests that indirect mechanisms play an important role or that the virus takes some time to be able to attack the nervous system. In support of indirect mechanisms is also the negative RT-PCR in 8 CSF samples. There was a clear male predominance (71%), which contrasts with a moderate female predominance (59.3%) in a retrospective Chinese series [5], but it is in line with the almost universal greater incidence of severe disease in males [1, 2].
Stroke was the main reason for consultation (11/35, 31%) and has been associated with the coagulopathy resulting in arterial and venous thrombosis, being more common in patients with severe disease [5, 14]. These data clearly illustrate that SARS-CoV-2 is responsible for coagulation disorders not normally associated with other viral respiratory infections. The question arises as to whether COVID-19 strokes are more severe and occur in younger patients than usual, and whether COVID-19 has resulted in an increase in the incidence of stroke. A comparison between the number of strokes admitted to our center during the period of this study in 2019 and 2020 shows that there was in fact a reduction of approximately one-third in the number of strokes. However, stroke severity was higher during the 2020 pandemic as reflected by an NIHSS twice as high as compared with 2019. This likely reflects that only patients with more severe strokes came to the hospital, a fact that has been observed in different parts of the world [15], and presents an important morbidity corollary to this pandemic. The average severity and age of the 11 COVID-19 related strokes were similar to that of the non-COVID-19 patients admitted in the same period of 2020. Our stroke patients had an increased D-dimer with a median value of 2400 ng/ml (equivalent to μg/L), higher than reported in a series of COVID-19 patients (900 μg/L) [5]. An increasingly appreciated feature of severe COVID-19 is the activation of coagulation pathways with development of disseminated intravascular coagulation. Thrombogenesis could be the result of activation of the endothelium in this infection [16] by direct infection with the virus or by the release of cytokines also resulting in the disruption of vascular integrity. This developing activation process results in clot formation and subsequent fibrin degradation leading to high levels of D-dimers, as we saw in our patients as predictive of poor outcome. While the association of increased levels of D-dimers in our stroke patients is consistent with its pathogenesis, the presence of markedly increased levels of D-dimers in patients with encephalopathy is not readily explained.
Encephalopathy followed stroke in frequency as a reason for consultation (7/35, 20%). Manifested as disorientation, confusion, and agitation in different combinations, encephalopathy is a complication of severe COVID-19 and has a multifactorial origin that includes the viral infection as well as the secondary inflammatory response and multiorgan failure. In our series, encephalopathy always required a neurologic consultation and was associated with markedly increased levels of D-dimer (tripling those of stroke patients), ferritin, and CRP levels. These increased values could be indicators of severe disease and suggest that fibrin degradation products could have a pathophysiological role. Encephalopathy often complicated the course and management of COVID-19 patients. It developed in 3 of 10 patients with ischemic stroke and 5 of 8 patients with seizures. In turn, 2 of 7 patients with encephalopathy developed seizures. These facts again reflect the difficulty in diagnosing and treating patients with severe SARS-CoV-2 infection who have multisystemic organ involvement and overlapping neurological complications. The role of neurologists in the care and recovery of these patients has been highlighted, emphasizing the benefit of multidisciplinary care [17].
Seizures in COVID-19 patients are infrequent but have been associated with features of encephalopathy or encephalitis [5, 18,19,20,21,22,23,24,25]. Seizures pose a particular diagnostic challenge, since performing an EEG, often in an ICU setting, is particularly difficult. Furthermore, treating these patients is also challenging due to the high number of interactions between antiepileptics and the variety of drugs employed in COVID-19 patients. Levetiracetam was successful in all cases and seems a safe drug in these patients. Seizures may appear in patients with no history of seizures and no other evident etiology except for the viral infection. The CSF analysis showed normal biochemistry, and RT-PCR was negative in 8 patients, suggesting that infectious encephalitis was not present, and thus offering no further clues to the etiology of seizures in this infection. A similar situation has been described in influenza patients [26, 27].
Neurological complications can represent the debut of undiagnosed SARS-CoV-2 infection, usually representing a severe condition with evidence of systemic inflammation and coagulation abnormalities that require prompt and specific management measures. In other patients, the complications will develop during admission, complicating the management of COVID-19 patients, especially considering the difficulties in performing ancillary diagnostic tests in these patients. It is now clear that COVID-19 is a protean infection with an equally clear role for the neurologist.
References
Chang LM, Wei L, Xie L, Zhu G, Dela Cruz CS, Sharma L (2020) Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan. China JAMA 323:1092. https://doi.org/10.1001/jama.2020.1623
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223):507–513. https://doi.org/10.1016/S0140-6736(20)30211-7
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, DSC H, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for C (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Collange O, Boulay C, Fafi-Kremer S, Ohana M, Anheim M, Meziani F (2020) Neurologic features in severe SARS-CoV-2 infection. N Engl J Med 382(23):2268–2270. https://doi.org/10.1056/NEJMc2008597
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 77(6):683–690. https://doi.org/10.1001/jamaneurol.2020.1127
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan. China JAMA 323:1061. https://doi.org/10.1001/jama.2020.1585
Wang Y, Wang Y, Chen Y, Qin Q (2020) Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol 92:568–576. https://doi.org/10.1002/jmv.25748
Garcia-Monco JC, Cabrera Muras A, Erburu Iriarte M, Rodrigo Armenteros P, Collía Fernández A, Arranz-Martínez J, Kapetanovic S, Lorenzo-García A, Bilbao González A, Gomez-Beldarrain M (2020) Neurological manifestations in a prospective unselected series of hospitalized COVID-19 patients. Neurology: Clin Pract. https://doi.org/10.1212/cpj.0000000000000913
Karadas O, Ozturk B, Sonkaya AR (2020) A prospective clinical study of detailed neurological manifestations in patients with COVID-19. Neurol Sci. https://doi.org/10.1007/s10072-020-04547-7
Vacchiano V, Riguzzi P, Volpi L, Tappata M, Avoni P, Rizzo G, Guerra L, Zaccaroni S, Cortelli P, Michelucci R, Liguori R (2020) Early neurological manifestations of hospitalized COVID-19 patients. Neurol Sci 41:2029–2031. https://doi.org/10.1007/s10072-020-04525-z
Romero-Sanchez CM, Diaz-Maroto I, Fernandez-Diaz E, Sanchez-Larsen A, Layos-Romero A, Garcia-Garcia J, Gonzalez E, Redondo-Penas I, Perona-Moratalla AB, Del Valle-Perez JA, Gracia-Gil J, Rojas-Bartolome L, Feria-Vilar I, Monteagudo M, Palao M, Palazon-Garcia E, Alcahut-Rodriguez C, Sopelana-Garay D, Moreno Y, Ahmad J, Segura T (2020) Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology. 95:e1060–e1070. https://doi.org/10.1212/WNL.0000000000009937
Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, Adams G, Hornick JL, Padera RF Jr, Sabeti P (2020) Neuropathological features of Covid-19. N Engl J Med 383:989–992. https://doi.org/10.1056/NEJMc2019373
Schaller T, Hirschbuhl K, Burkhardt K, Braun G, Trepel M, Markl B, Claus R (2020) Postmortem examination of patients with COVID-19. JAMA. 323:2518. https://doi.org/10.1001/jama.2020.8907
Fatima N, Saqqur M, Qamar F, Shaukat S, Shuaib A (2020) Impact of COVID-19 on neurological manifestations: an overview of stroke presentation in pandemic. Neurol Sci:1–5. https://doi.org/10.1007/s10072-020-04637-6
Markus HS, Brainin M (2020) COVID-19 and stroke-a global world stroke organization perspective. Int J Stroke 15(4):361–364. https://doi.org/10.1177/1747493020923472
Teuwen LA, Geldhof V, Pasut A, Carmeliet P (2020) COVID-19: the vasculature unleashed. Nat Rev Immunol 20:389–391. https://doi.org/10.1038/s41577-020-0343-0
Gupta R, Gupta A, Ghosh AK, Stein J, Lindsay L, Beckley A, Labella AM, Tassy R, Rivera L, Rodriguez G, Katz MD, Howard LH, Shapiro A, Deland EL, Heilpern KL (2020) A paradigm for the pandemic unit: a Covid-19 recovery unit. New Engl J Med Catalyst. https://doi.org/10.1056/CAT.20.0238
Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M (2020) Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA 323(16):1612–1614. https://doi.org/10.1001/jama.2020.4326
Duong L, Xu P, Liu A (2020) Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown Los Angeles, early April 2020. Brain Behav Immun 87:33. https://doi.org/10.1016/j.bbi.2020.04.024
Hung EC, Chim SS, Chan PK, Tong YK, Ng EK, Chiu RW, Leung CB, Sung JJ, Tam JS, Lo YM (2003) Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem 49(12):2108–2109. https://doi.org/10.1373/clinchem.2003.025437
Karimi N, Sharifi Razavi A, Rouhani N (2020) Frequent convulsive seizures in an adult patient with COVID-19: a case report. Iran Red Crescent Med J 22(3). https://doi.org/10.5812/ircmj.102828
Lu L, Xiong W, Liu D, Liu J, Yang D, Li N, Mu J, Guo J, Li W, Wang G, Gao H, Zhang Y, Lin M, Chen L, Shen S, Zhang H, Sander JW, Luo J, Chen S, Zhou D (2020) New-onset acute symptomatic seizure and risk factors in corona virus disease 2019: a retrospective multicenter study. Epilepsia. 61:e49–e53. https://doi.org/10.1111/epi.16524
Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S (2020) A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis 94:55–58. https://doi.org/10.1016/j.ijid.2020.03.062
Sohal S, Mossammat M (2020) COVID-19 presenting with seizures. IDCases:e00782. https://doi.org/10.1016/j.idcr.2020.e00782
Vollono C, Rollo E, Romozzi M, Frisullo G, Servidei S, Borghetti A, Calabresi P (2020) Focal status epilepticus as unique clinical feature of COVID-19: a case report. Seizure 78:109–112. https://doi.org/10.1016/j.seizure.2020.04.009
Mylonaki E, Harrer A, Pilz G, Stalzer P, Otto F, Trinka E, Wipfler P (2020) Neurological complications associated with influenza in season 2017/18 in Austria- a retrospective single center study. J Clin Virol 127:104340. https://doi.org/10.1016/j.jcv.2020.104340
Ruisanchez-Nieva A, Martinez-Arroyo A, Gomez-Beldarrain M, Bocos Portillo J, Garcia-Monco JC (2017) Influenza-associated seizures in healthy adults: report of 3 cases. Epilepsy Behav Case Rep 8:12–13. https://doi.org/10.1016/j.ebcr.2017.01.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement and informed consent
The study was approved by the Ethics Committee of the Basque Country. This study was considered exempt from informed consent because it was anonymous and only reported results derived from the medical care of the patient.
Additional information
The data that support the findings of this study are available on request from the corresponding author.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Moncó, J.C., Cabrera-Muras, A., Collía-Fernández, A. et al. Neurological reasons for consultation and hospitalization during the COVID-19 pandemic. Neurol Sci 41, 3031–3038 (2020). https://doi.org/10.1007/s10072-020-04714-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04714-w