Introduction
Suicide is now a leading cause of death in the US, especially for those under 35, and rates have increased over the last two decades. 1 The COVID-19 pandemic has exacerbated this suicidal trend and has contributed to worsening mental health in general. In late June 2020, 40% of US adults reported struggling with poor mental health or substance abuse, Reference Czeisler, Lane and Petrosky2 and from March–October 2020, the proportion of mental health-related emergency department visits for children and adolescents increased by 24% and 31%, respectively, compared to 2019, Reference Leeb, Bitsko, Radhakrishnan, Martinez, Njai and Holland3 with the largest increases among adolescent girls. Reference Radhakrishnan, Leeb and Bitsko4 While emergency department visits for mental health conditions can indicate an increase in mental health crises, earlier indicators of population-level behavioral health could identify issues that may benefit from prompt public health intervention.
A potential source of data on population-level behavioral health, including attempted suicides, comes from the 55 poison control centers (PCs) across the US. These centers receive calls about exposures to potentially harmful substances. Callers are asked whether the exposure was unintentional or intentional, and, if intentional, whether the exposure should be classified as a suspected suicide or overdose. Intentional ingestions represent a substantial proportion of suicide deaths; in 2019, 13% of suicide deaths were attributable to poisoning, with considerable variation by gender. 1 PCs submit data resulting from each call to the National Poison Data System® (NPDS), a data warehouse managed by America’s Poison Centers, a non-profit organization representing all PCs in the US. 5 Data from PCs are uploaded to NPDS® in near-real time (about every 8 minutes), which allows for national surveillance capabilities. Public health officials use NPDS surveillance features to identify incidents of public health significance (e.g., chemical exposures with a geographic or spatial pattern). Reference Carpenter, Chang, Bronstein, Thomas and Law6–Reference Wolkin, Martin, Law, Schier and Bronstein8 However, PC data are not yet widely used by public health officials to monitor behavioral health. After a significant public health emergency (PHE), such as a natural disaster or a pandemic, changes in the volume of calls for intentional exposure (IE) may serve as an early indicator of worsening population-level behavioral health. Although some prior research has examined total PC call volume after PHEs, Reference Klein, Herzog, Smolinske and White9,Reference Nathan, Olson, Everson, Kearney and Blanc10 no studies were identified that have examined the association between PHEs and changes in IE call rates, nor have they examined variation by gender and age. This study addresses this gap by assessing PC calls in Dallas County, Texas to: (1) explore changes in IE call volume and variation by gender and age, and (2) examine the association between two different PHEs and changes in IE call volume.
Methods
NPDS® data were obtained on calls for human exposures for Dallas County, Texas, for the time period from March 1, 2019, through April 30, 2021, which included daily call volume prior to, during, and after: (1) the COVID-19 emergency declaration by the World Health Organization on March 11, 2020, and (2) a local surge in COVID-19 cases beginning in July 2020; and (3) Winter Storm Uri in mid-February 2021 that led to widespread power outages during sub-freezing temperatures. Calls for IEs were identified as those with the following documented call reasons: ‘Intentional – Suspected suicide,’ ‘Intentional – Misuse,’ ‘Intentional – Abuse,’ and ‘Intentional – Unknown.’ Calls were categorized by date, by gender of the person of concern (female versus male), and by age group of the person of concern (children 0–5 years, children 6–12 years, youths 13–19 years, and adults 20+ years), consistent with NPDS categories, and the data was smoothed using a 7-day moving average.
7-day moving average of daily calls for IEs were plotted overall and by gender and age of the person of concern. An alert threshold was set at the 95th percentile of the distribution of the 7-day moving average in the pre-COVID-19 declaration period (i.e., prior to March 11, 2020). Single-group, segmented linear interrupted time series (ITS) analysis was then conducted with Newey-West standard errors, adjusting for day-of-the-week effects and including up to a 1-week lag in the autocorrelation structure, to examine whether the PHE time periods were associated with a change in daily IE call volume. Analyses were conducted using STATA 16.0 (Stata Corp., College Station, TX). The study team’s organizational institutional review board deemed this study to be exempt from full review. This analysis follows STROBE reporting guidelines for observational studies.
Results
Description of the sample
The study sample included 30362 calls (Table 1), with a mean weekly call volume of 266 (range: 56 to 383). More than 50% (52.1%) of calls were concerning women, and the average age of persons of concern was 19.0 years (standard deviation [SD] 22). Intentionality of the exposure (intentional versus unintentional) was documented for 91% of calls. Of those, 5281 calls (17.4%) were for IEs, with a mean weekly IE call volume of 46 (range: 8 to 82). Nearly 75% of IE calls were for suspected suicide attempts, representing 12.8% of total call volume during the study period. For suspected suicide attempt calls, 64.4% were concerning women, and the average age of persons of concern was 29.1 years (SD 16). Gender was missing for less than 1% of calls; age was missing for only 9% of all calls, and 3% of those were categorized as suspected suicide attempt.
Table 1. Characteristics of poison control center calls in Dallas County Texas March 2019 –April 2021 (N = 30362)

Changes in intentional exposure call volume
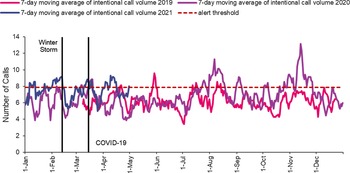
Figure 1 shows a time series plot of the seven-day moving average of IE call volume from March 1, 2019, through April 30, 2021. IE calls increased briefly immediately after the declaration of the COVID-19 pandemic then decreased to baseline until again increasing above the 95th percentile alert threshold in July 2020. IE call volume also briefly exceeded the alert threshold in early September and early October 2020, then peaked in mid-November 2020. These spikes correspond to waves of COVID-19 cases in the summer and early fall of 2020 in Dallas County as well as the start of a prolonged winter wave of COVID-19 cases that began in November 2020. In contrast to the temporal associations that corresponded to COVID-19 surges during the period studied, IE call volume declined sharply in the weeks following Winter Storm Uri in February 2021, then returned to the pre-storm baseline (Figure 1).

Figure 1. 7-day Moving Average of IE call volume, Dallas County, March 2019 – April 2021.
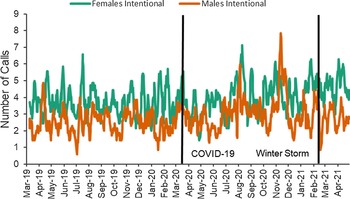
IE call volume was consistently higher for women as the person of concern compared to men, with the exception of IE call volume for men markedly exceeding call volume for women in November 2020 (Figure 2).

Figure 2. 7-day Moving Average of intentional PCC call volume stratified by gender, Dallas County, March 2019–April 2021.
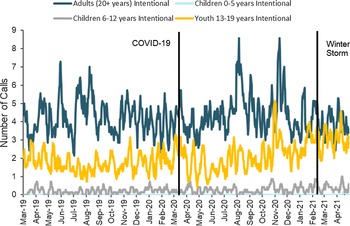
IE call volume was consistently higher for adults than for children and youths until about November 2020. The 7-day moving average of IE calls for exposures among youth (based on 2019 pre-pandemic data) trended upward after the pandemic declaration on March 11, 2020, nearly closing the historical gap between adults and youth by early 2021 (Figure 3). The peak in IE call volume among adults in August/ September 2020 did not appear to occur among children and youth, but IE volume among both adults and youth peaked in October/ November 2020, with youth calls increasing first.

Figure 3. 7-day Moving Average of IE call volume stratified by age, Dallas County, March 2019–April 2021.
Interrupted time series analysis (ITSA)
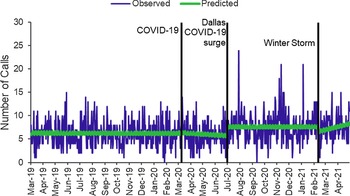
Figure 4 shows the results of the segmented linear ITS analysis, with observed versus model-fitted call volume. Neither the declaration of the COVID-19 pandemic nor Winter Storm Uri was associated with a significant change in the level of IE calls in Dallas County, but the level of daily IE calls was 1.9 calls greater after the start of the summer wave of COVID-19 cases in Dallas County beginning in July, 2020 (95% CI 0.7 to 3.1). Another peak can be seen in November, occurring at the same time as another surge in local COVID-19 burden.

Figure 4. Observed versus predicted IE call volume around COVID-19 and Winter Storm Uri, ITSA, Dallas County, March 2019–April 2021.
Limitations
NPDS® data are routinely used for public health surveillance by government agencies, but these data have not been used to monitor population behavioral health. Since PC data are collected for the clinical management of poison patients, specific data elements pertaining to population behavioral health are limited. This data is not representative of all potential intentional exposures in a population but only of those for which a call was made to a PC for a potentially affected individual, meaning some cases of exposure may not be captured. Increasingly, people may seek information about a potential exposure through the PC website or via text message rather than phone call, such that temporal changes in call volume may be related to broader changes in how people seek information about exposures. Furthermore, there may be misclassification of the intentionality of the exposure or other key variables, especially when call volumes surge during PHEs. Reference Vassilev, Kashani, Ruck, Hoffman and Marcus11 Although the demographic data for gender and age of the person of concern are relatively complete, data on race/ ethnicity, socioeconomic status, or educational attainment are not collected. Finally, our dataset did not include the details of the specific substance to which the individual was exposed.
Discussion
In this analysis of IE calls in Dallas County, Texas, during a period that included the declaration of the COVID-19 pandemic, a local surge in COVID-19 cases, and Winter Storm Uri, IE call volume was associated with a local wave of COVID-19 infections. However, there was no association with the declaration of the pandemic nor with a severe winter storm. IE call volume also varied by gender and age, with a notable increase among youth ages 13 to 19 during the pandemic.
Calls for IEs indicate that individuals are experiencing behavioral health challenges, and in aggregate, call volume to PCs for IEs provides a window into these challenges at a population level. It is known that PHEs can negatively impact population-level behavioral health, Reference Newnham, Mergelsberg and Chen12 and our study extends this literature by showing that the association between IE call volume and a PHE may depend on both the type of PHE and its local impact. For instance, IE call volume did not significantly increase immediately after the COVID-19 national emergency declaration, but a local surge in the summer of 2020 correlated with increased IE call volume. This finding is consistent with other research documenting increases in call volume in the context of PHEs, including a multi-state power outage in 2003, Reference Klein, Herzog, Smolinske and White9 and a 1989 earthquake in California. Reference Nathan, Olson, Everson, Kearney and Blanc10 Since the pandemic has impacted communities across the US differently and at different times, depending on a variety of contextual factors, local policies, and transmission patterns, Reference White and Hebert-Dufresne13–Reference Block, Martin and Boscardin15 local variation in timing of behavioral health impacts is expected.
This study also found that IE call volume varied by gender in the context of both PHEs, with higher IE call volume for women, except in November 2020, when calls for men exceeded those for women. Gender differences in suicidality during the pandemic have been demonstrated in other studies of suicide attempts from emergency department visits, Reference Yard, Radhakrishnan and Ballesteros16 and surveys. Reference Jones and Hertz17 This finding highlights the importance of considering differential needs of sociodemographic groups and the potentially differential behavioral health impacts of PHEs on those groups as well as the potential value of collecting other demographic data, such as race and ethnicity, where differences have been previously demonstrated. Reference Mitchell and Li18
There was an increase in IE calls among youth, nearly approximating adult levels by a year after the PHE was declared, which is consistent with documented increases in youth suicidal ideation, attempts, and general mental health problems during the pandemic. Reference Czeisler, Lane and Petrosky2–Reference Radhakrishnan, Leeb and Bitsko4,Reference Jones and Hertz17,Reference Otto, Jary and Sturza19 For example, a national study of high school students based on the 2021 Adolescent Behaviors and Experiences Survey found that in the past 12 months, 44% experienced ‘persistent feelings of sadness or hopelessness,’ almost 20% had seriously considered attempting suicide, and 9% had actually attempted suicide. Reference Jones and Hertz17 Isolation, fear, anxiety, and financial impacts of the pandemic likely contributed to this trend, though more research is needed to pinpoint the causes and the potential targets for intervention. Reference Hossain, Tasnim and Sultana20,Reference Brasso, Bellino, Blua, Bozzatello and Rocca21 The consistency of these findings for demographic subgroups with existing research supports the usefulness of this data for tracking suicidal ideation.
Strengths of these data include their temporal granularity (i.e., available weekly), the standardized format in which PC calls are reported across the country and their historical availability, their geographic granularity down to the zip code level, and their consistent documentation of gender and age as well as intentionality of the exposure. Reference Law, Schier, Schauben, Wheeler and Mulay22 PC IE call data are therefore a promising data source for monitoring population-level behavioral health in the PHE context. However, depending on arrangements with Poison Control Centers, it may take several weeks for public health officials to request and receive data, and public health officials may incur a cost to obtain these data. Additionally, the lack of race and ethnicity data means that behavioral health inequities cannot be easily explored. Furthermore, like any data not intended for surveillance purposes, caution is warranted, as these data are not population-representative.
Conclusions
This analysis of intentional poisoning calls in Dallas County from March 2019 through April 2021 demonstrates that PC call data show variation in IE call volume based on age, and gender and that IE call volume was temporally associated with local severity of the COVID-19 pandemic. Public health and behavioral health officials could consider monitoring IE call volume as a timely, local-level indicator of population behavioral health, thereby allowing them to anticipate and address emerging behavioral health crises in their communities.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2023.6
Acknowledgments
We would like to thank America’s Poison Centers for their help providing the data and the regional poison control centers we spoke with for their important input. We also thank RAND colleague Hilary Peterson for her assistance with preparing this manuscript for submission.
Research reported in the manuscript has been funded by the US Centers for Disease Control and Prevention (CDC), an Agency of the Department of Health and Human Services, under CDC contract 75D30119C06926: public health use of current resources and existing surveillance systems to monitor mental and behavioral health during and after an emergency; turning data into action. The ideas expressed in the articles are those of the authors and do not necessarily reflect the official position of the CDC.
Author contributions
All authors (SHF, RKL, JDA, and LJF) collaborated on the conceptualization of the research; SHF drafted the manuscript; RKL conducted the analysis and edited the manuscript; JDA and LJF offered significant feedback on the analysis and on the manuscript.
Funding statement
Research reported in the manuscript has been funded by the US Centers for Disease Control and Prevention (CDC), an Agency of the Department of Health and Human Services, under CDC contract 75D30119C06926.
Abbreviations
IE, Intentional Exposure; ITS, Interrupted Time Series; ITSA, Interrupted Time Series Analysis; NPDS, National Poison Data System®; PHE, Public Health Emergency; PC, Poison Center