Efficacy of a 6-Week Home-Based Online Supervised Exercise Program Conducted During COVID-19 in Patients With Post Percutaneous Coronary Intervention: A Single-Blind Randomized Controlled Trial
- 1Department of Sport Rehabilitation, School of Kinesiology, Shanghai University of Sport, Shanghai, China
- 2Department of Cardiology, Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai, China
- 3Department of Health Professions, Faculty of Art, Health and Design, Swinburne University of Technology, Melbourne, VIC, Australia
- 4Research Institute for Sport and Exercise, University of Canberra, Canberra, ACT, Australia
- 5College of Rehabilitation Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, China
Objective: The aim of this study was to assess the efficacy of a 6-week cardiac rehabilitation (CR) program designed for patients with coronary artery disease (CAD) after percutaneous coronary intervention (PCI) that involved an online supervised exercise program that they could access during COVID-19.
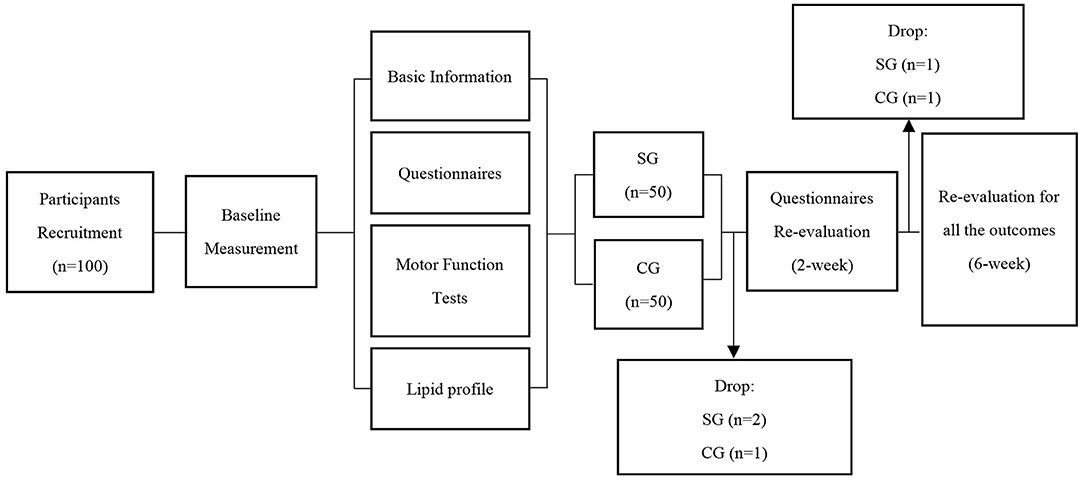
Methods: One hundred patients were randomly allocated into control group (CG) and supervision group (SG). CG accepted conventional health education with a home exercise program booklet delivered before discharge, SG had an additional home-based online supervised exercise program (HOSEP). Questionnaires, motor function and lipid profile were administered at baseline. Questionnaires included the Godin-Shephard Leisure-Time Physical Activity questionnaire (GSLTPAQ) and Bandura's Exercise Self-efficacy (ESE). Motor function included: 6-min walk test (6 MWT), timed up and go test (TUG), 30-s sit to stand (30-s STS), and Hand Grip Strength (HG). Lipid profile included: low-density lipoprotein (LDL), high-density lipoprotein (HDL), total cholesterol (TC) and triglycerides (TG). The questionnaires were re-administered after 2-weeks, all tests were re-evaluated after 6-weeks.
Results: the questionnaire results showed that scores on GSLTPAQ and ESE were significantly improved in the SG. The changes in GSLTPAQ scores from baseline to 2- and 6-weeks in the SG were significantly higher than in the CG (2-week: 6.9 ± 13.0 for SG and 0.2 ± 10.2 for CG, p = 0.005; 6-week: 9.4 ± 18.1 for SG and 0.2 ± 11.8 for CG, p = 0.003). in terms of motor function, both the CG and SG improved TUG and 6 MWT performance, with the 6 MWT improvement being significantly greater in the SG than CG (43.7 ± 39.2 m for SG and 16.6 ± 39.1 m for CG, p = 0.001). Improvement in the 30-s STS was significantly greater in the SG than CG (2.4 ± 3.6 repetitions for SG and 0.4 ± 3.5 repetitions for CG, p = 0.007). the lipid profile level significantly improved over baseline in both SG and CG after 6-week intervention, and these changes were not statistically different between groups.
Conclusion: This pilot randomized control study demonstrated that a 6-week HOSEP, when added to education delivered pre-hospital discharge for CAD patients following PCI, was beneficial with respect to exercise self-efficacy, exercise behavior, motor function and lipid profile. Supervised exercise programs delivered online in addition to education providing effective and accessible CR during COVID-19.
Introduction
According to the Report on Cardiovascular Health and Diseases in China: an Updated Summary of 2020, the prevalence of cardiovascular disease in China is 330 million, of which 11 million are coronary artery disease (CAD) (1). Percutaneous coronary intervention (PCI) is a clinical intervention to dilate and maintain patency for narrowing of the coronary arteries with significant therapeutic efficacy (2).
Cardiac rehabilitation (CR) has been recommended as an effective treatment that reduces mortality and morbidity in CAD patients after PCI (3, 4), and is supported as secondary prevention for CAD (5). CR should commence as soon as possible after hospital admission, and continue into the community upon hospital discharge (3, 6). Although the majority of patients may commence CR after PCI whilst in hospital, many cannot continue when discharged due to a shortage of programs and health professionals to support CR programs in the community (7, 8).
Home-based CR with online supervision has shown its merit in overcoming barriers of time and distance, and thus has become successful in increasing CR participation rates (7). A systematic review has demonstrated that long term (over 3 months) supervised home-based CR is not significantly different from center-based CR with respect to improving exercise capacity, risk factors and psychosocial state (8). However, the effect of short-term supervised home-based CR has not been studied and its effect on both physical and psychological measures remains unclear. Therefore, the purpose of this study was to evaluate the safety and efficacy of a 6-week home-based online supervised exercise program (HOSEP) as CR for CAD patients after PCI. The results will inform CR practice by providing evidence regarding low-cost, more convenient home-based CR, especially during the COVID-19 pandemic.
Methods
Participants
This study was approved by the Human Subjects Committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University school of Medicine (No. XHEC-C-2020-078-1) and registered in the Chinese Clinical Registration Center (clinical trial website: http://www.chictr.org.cn/enIndex.aspx; clinical trial registry number: Chi CTR2000037435). All Participants completed informed consent before commencement of data collection. Participants included all patients with CAD after PCI in the Department of Cardiology from Xinhua Hospital during January to December 2020. Inclusion criteria were: ➀clinically diagnosed CAD with PCI; ➁Mini Mental State Examination (MMSE) ≥24 (9); ➂native language is Chinese; ➃age ≥18 years old; ➄able to evaluate and sign informed consent on time. Exclusion criteria were: ➀left ventricular ejection fraction <40% or heart function-New York Heart Association (NYHA) grade above level III (10); ➁severe cardiac arrhythmia and cardiogenic shock; ➂combined with severe hypertension, hypertrophic cardiomyopathy, moderate to severe valvular disease, acute pericarditis or myocarditis; ➃combined with any other diseases that affect activity, such as severe liver, kidney and respiratory dysfunction, nervous system diseases, musculoskeletal system diseases, visual or auditory dysfunction; ➄had or is having CR.
Procedure
Participants were tested at the Department of Cardiology of Xinhua Hospital during January to December 2020. All participants were blind to the intervention and randomly allocated into the Supervision group (SG) or the Control group (CG).
Baseline information, including questionnaires, motor function and lipid profile, were collected on the day before discharge.
Questionnaires were administered under the supervision of a CR physical therapist, motor function was assessed by another CR physical therapist, and lipid profile tests were done in a certified medical laboratory.
All participants had conventional face-to-face health education and the home exercise program booklet was given to the patients by a CR physical therapist before discharge. The home exercise program included walking for 30–60 min, and STS exercise for 2–3 sets every day, with scoring at 4–5 on RPE 0–10, and at 60–80% of maximum heart rate (HRmax) (HRmax = 220-age) calculated for intensity (11–13) (see Supplementary Material for an example of home exercise program). The SG had additional HOSEP, where patients were added into a WeChat virtual community and reminded every day, at 8 a.m., to 10 a.m., by CR physical therapist, to complete the walking and STS exercise as per their home exercise program.
Participants were followed up as outpatients for a 6-week period. Questionnaires were administered again at 2- and 6-weeks, motor function and lipid profile were evaluated again after the 6-week intervention. All tests were done with the same estimator and place as baseline in order to minimize sources of variability.
The study design and experiment flowchart are presented in Figure 1.
Outcome Measures
Questionnaires administered included Bandura's Exercise Self-efficacy (ESE) instrument (14) and the Godin-Shephard Leisure-Time Physical Activity Questionnaire (GSLTPAQ) (15).
Motor function tests included the 6-min Walk Test (6 MWT) (16), 30-s sit-to-stand test (30-s STS test) (17), Timed Up and Go test (TUG test) (17) and Hand Grip Strength (HG) (18). HG and TUG were assessed at first, then the 6 MWT and 30-s STS were conducted in random order. There was a 1-min interval between HG, TUG and 6 MWT, and 30 min between 6 MWT and the 30-s STS test to ensure Ratings of Perceived Exertion (RPE), heart rate and blood pressure returned to normal (18, 19). 6 MWT was conducted as per the American Thoracic Society statement (16). It was tested in a straight, unobstructed, flat corridor that was over 30 meters long. A start line was marked at one end of the corridor and the 30 m point was marked with a traffic cone as the turnaround point. For safety during the test, a chair and a source of oxygen station in the corridor were prepared. Before 6 MWT, a CR physical therapist measured patients' pulse, blood pressure, and RPE, and gave standardized instructions and encouragement. Walking distance and Post-test RPE, pulse and blood pressure were recorded.
Lipid profile included low-density lipoprotein (LDL), high-density lipoprotein (HDL), total cholesterol (TC), triglycerides (TG).
Data Analysis
SPSS 25.0 software (IBM Corp., Armonk, NY) was used for data analysis, with intention-to-treat analysis (20). Demographic characteristics were analyzed via descriptive statistical methods. The intragroup comparison was conducted via repeated measures analysis of variance (ANOVA) and intergroup comparison of value changes by independent sample t-test. All results were expressed as mean ± standard deviation () and p < 0.05 indicated a statistically significant difference.
Results
Basic Information
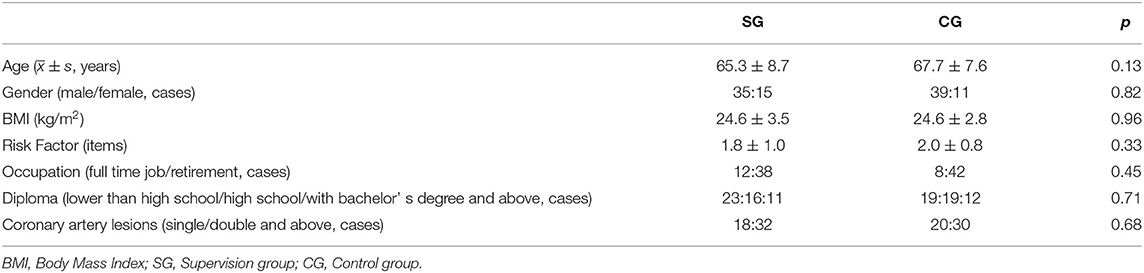
At the commencement of this study, 50 patients were randomly assigned for each SG and CG. At 2-week follow-up, two patients in the SG and one patient in CG dropped out for family reasons. At 6-week follow-up, one patient in each group decined to continue participation in the experiment. Therefore, 47 and 48 patients in the SG and CG, respectively completed the 6-week intervention. There were no adverse events reported during the intervention period. All patients were treated with dual antiplatelet therapy (Aspirin + Clopidogrel/Ticagrelor), β-Blocker and Stain. There were no differences between the two groups on antihypertensive (34:40, p = 0.17) and hypoglycemic treatments (18:15, p = 0.52). There were no significant intergroup differences in the demographic data at baseline (Table 1).
Questionnaires
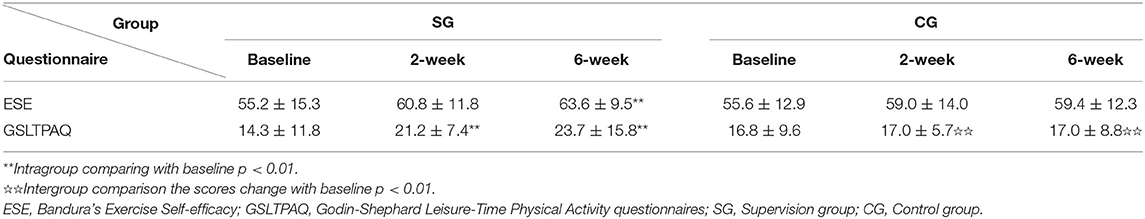
The intergroup comparison showed no statistically significant differences in the baseline questionnaire results (Table 2).
Obtained p in the SG showed that, compared with baseline, the ESE scores significantly improved at 6-weeks (p = 0.001, 95% CI: 2.8–13.8), and the GSLTPAQ scores significantly improved at 2- and 6-weeks (2-week: p < 0.01, 95% CI: 2.9–10.9; 6–week: p < 0.01, 95% CI: 4.2–14.6). The intragroup comparison in the CG showed no significant differences in ESE and GSLTPAQ scores across the 3 testing points.
The intergroup comparison for the score change in GSLTPAQ showed significantly greater progress at 2- and 6-week in the SG compared with CG (2-week: 6.9 ± 13.0 vs. 0.2 ± 10.2, p = 0.005, 95% CI: 2.1–11.4. 6-week: 9.4 ± 18.1 vs. 0.2 ± 11.8, p = 0.003, 95% CI: 3.1–15.2).
Motor Function Tests
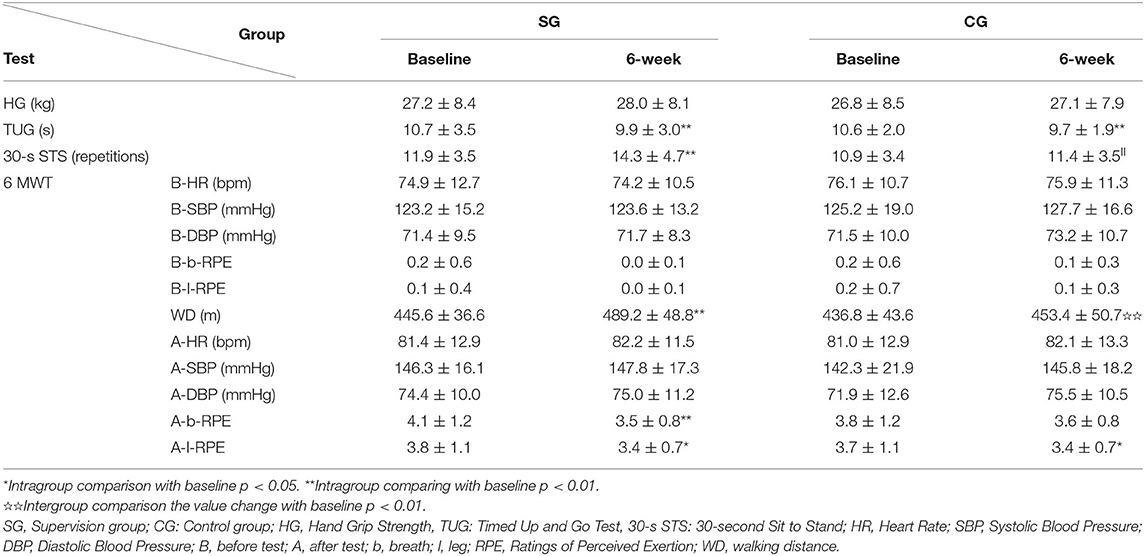
The intergroup motor function tests comparisons showed no statistically significant differences at baseline (Table 3).
Results of 30-s STS tests improved significantly only in the SG (p < 0.01, 95% CI: 1.4–3.4). In addition, the repetitions changes in the SG were significantly better than those in CG (SG: 2.4 ± 3.6 repetitions; CG: 0.4 ± 3.5 repetitions, p = 0.007, 95% CI: 0.5–3.3). The 6 MWT performance increased significantly after 6-weeks in both the SG and CG (SG: p < 0.01, 95% CI: 32.7–54.7; CG: p = 0.003, 95% CI: 5.6–27.6), and the distance changes of 6 MWT in SG were significantly better than those in CG (SG: 43.7 ± 39.2 m, CG: 16.6 ± 39.1 m, p = 0.001, 95% CI: 11.5–42.6). After 6-weeks, the RPE scores for 6 MWT decreased significantly in the SG (RPE for respiration: p = 0.002, 95% CI: 0.2–0.9; RPE for leg fatigue: p = 0.01, 95% CI: 0.1–0.7), while in the CG only lower extremity fatigue RPE decreased significantly (p = 0.03, 95% CI: 0.04–0.64). Results for the TUG after the 6-week intervention improved significantly in both groups (SG: p = 0.001, 95% CI: 0.3–1.2; CG: p < 0.01, 95% CI: 0.4–1.3). There was no significant change in HG in either group.
Lipid Profile
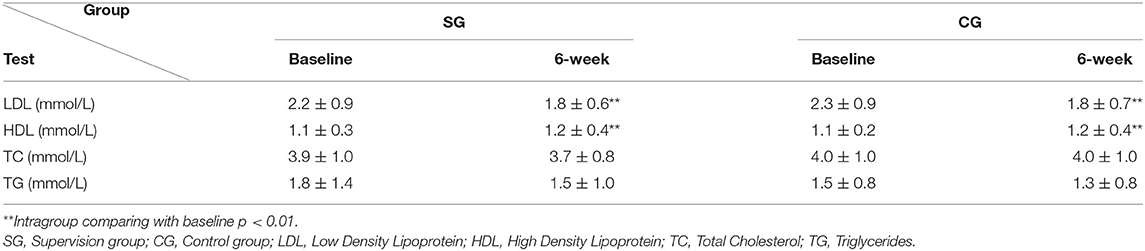
The intergroup analysis showed no statistically significant differences at baseline for lipid profile (Table 4). Both LDL and HDL changed significantly compared with baseline at 6-weeks in both groups, and the value changes did not differ significantly between groups.
Discussion
This randomized controlled pilot study showed that both conventional education with a home exercise program booklet delivered before hospital discharge and an additional 6-week HOSEP were safe and effective for improving motor function and lipid profile in early Phase II community CR for CAD patients after PCI. More importantly, compared to conventional intervention, the patients who received additional HOSEP showed further improvements in their exercise self-efficacy, exercise behavior and motor function, suggesting that 6-week HOSEP, as a short-term intervention, was a feasible and valid home-based CR. These findings provide evidence regarding a low-cost, more convenient, short-term, supervised home-based CR program, especially during the COVID-19 pandemic.
In this study, WeChat (a messaging and calling app for smartphones) was used as the online supervision platform. WeChat-based CR intervention for CAD has been shown to be promising in China, with advantages such as convenience, popularity and flexibility (21). More importantly, the WeChat app has been found to be client-friendly and easy to use, even for older people (8, 22, 23). With the video call function, patients could have immediate access to medical support through their WeChat group or use one-to-one chat.
The motor function performance of both groups improved significantly. Specifically, the 6 MWT and TUG improved significantly in both groups, and the SG also improved their performance on the 30-s STS tests.
The 6 MWT is an important indicator of cardiopulmonary function in patients with CAD (16). After a 6-week intervention, both groups improved their walking distance over 450 m, indicating that their cardiopulmonary fitness may be close to normal (24). Further, the distance change in the SG was more than the minimal clinically important difference (MCID) (22), suggesting that the beneficial effect from the additional HOSEP was clinically significant. In addition, the RPE of lower extremity fatigue after 6 MWT was significantly reduced in both groups, whereas the RPE for respiratory fatigue was significantly reduced only in the SG. These findings suggest that the additional HOSEP had benefits in both musculoskeletal and respiratory systems. This is consistent with previous research, where the researchers found that aerobic exercise combined with resistance exercise improved musculoskeletal and cardiopulmonary fitness of patients with CAD (23, 25).
TUG is a test that reflects the quality of dynamic balance function (17), which involves both proprioceptive input and motor output (26). In the current study, both groups showed significant improvement in TUG but lower limb strength, i.e., motor output, only improved in the SG, suggesting that the change in observed TUG performance may be also related to proprioceptive change through exercise intervention. Future study is needed to explore the effect of CR on proprioceptive function, and how it contributes to dynamic balance control after PCI.
Lower limb muscle strength, measured by using STS, is an important contributor to CAD patients' daily living, because it has been found to be strongly associated with exercise capacity and risk of all-cause and cardiovascular mortality (27, 28). Studies by Fujita (29) found that regular STS can be used as an effective resistance exercise to improve lower extremity strength. In this study, although we prescribed for both groups to perform regular STS, only patients in the SG improved their STS performance significantly. This is likely because the HOSEP improved patients' motivation to perform the hop exercise regularly.
For the lipid profile, the blood results showed that HDL and LDL were more ideal in both groups after 6-weeks of CR. The results were comparable to other long-term HOSEP studies (30, 31), suggesting that short-term HOSEP can also benefit participants' lipid profile. Additionally, research has shown that long-term (more than 3 months intervention) HOSEP can also improve TC and TG (32). However, we did not find any significant change in TC and TG in this short-term (6 week) study. Further work is needed to determine how long the intervention needs to be to achieve effective change in TC and TG. In addition, there is a need to consider including more biochemical/physiological parameters, such as blood morphology, electrocardiogram, or respiratory fitness tests, in that this information feedback may contribute to greater patient motivation to continue physical activity.
The questionnaire results showed that the score change on GSLTPAQ in the SG was significantly higher than the CG. Scores for ESE significantly improved between baseline and 6 weeks in the SG. These findings suggest that patients in the HOSEP group may have developed a better sense of self-efficacy and exercised more regularly at home, a result which is also similar to the effects found in a long-term online exercise study (33).
Conclusion
Both conventional education and the additional 6-week HOSEP were safe and beneficial with respect to motor function and lipid profile. HOSEP can further improve patients' exercise behavior and motor function over conventional treatment. Therefore, a 6-week HOSEP in early phase II CR should be considered as an effective intervention as it can be conducted at home, especially during the COVID-19 pandemic, and it provides safe access to all patients following PCI in the community, thereby reducing demand on services.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by Human Subjects Committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JL, ZW, BL, JH, and SM designed the study and had primary responsibility for this work. JL, ZW, and BL responsible for the execution of the trial and data collection. JL and ZW analyzed the data and discussed with JH and SM. JL wrote the first draft, which was improved by SM and JH. DE-A and RA critically reviewed and improved the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the 2021 Curriculum Construction Project of Xinhua Hospital affiliated to Shanghai Jiaotong University School of Medicine.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors express their gratitude to all the volunteers who took part.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.853376/full#supplementary-material
References
1. The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on cardiovascular health and diseases burden in China: An updated summary of 2020. Chin Circul J. (2021) 36:521–45. doi: 10.3969/j.issn.1000-3614.2021.06.001
2. Bhatt DL. Percutaneous coronary intervention in 2018. JAMA (2018) 319:2127–8. doi: 10.1001/jama.2018.5281
3. Smith SC, Benjamin Jr. EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American heart association and american college of cardiology foundation. Circulation. (2011) 124:2458–73. doi: 10.1161/CIR.0b013e318235eb4d
4. Thomas RJ, King M, Lui K, Oldridge N, Piña IL, Spertus J. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation. (2007) 116:1611–42. doi: 10.1161/CIRCULATIONAHA.107.185734
5. Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. (2021) 42:17–96. doi: 10.1093/eurheartj/ehaa605
6. Piepoli MF, Corrà U, Adamopoulos S, Benzer W, Bjarnason-Wehrens B, Cupples M, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European association for cardiovascular prevention & rehabilitation. endorsed by the committee for practice guidelines of the european society of cardiology. Eur J Prev Cardiol. (2014) 21:664–81. doi: 10.1177/2047487312449597
7. Brouwers RWM, van der Poort EKJ, Kemps HMC, van den Akker-van Marle ME, Kraal JJ. Cost-effectiveness of cardiac telerehabilitation with relapse prevention for the treatment of patients with coronary artery disease in the Netherlands. JAMA Netw Open. (2021) 4: e2136652. doi: 10.1001/jamanetworkopen.2021.36652
8. Huang K, Liu W, He D, Huang B, Xiao D, Peng Y, et al. Tele health interventions versus center-based cardiac rehabilitation of coronary artery disease: A systematic review and meta-analysis. Eur J Prevent Cardiol. (2015) 22:959–71. doi: 10.1177/2047487314561168
9. Li H, Jia J, Yang Z. Mini-mental state examination in elderly chinese: A population-based normative study. J Alzheimer Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
10. Caraballo C, Desai NR, Mulder H, Alhanti B, Wilson FP, Fiuzat M. et al Clinical implications of the new york heart association classification. J Am Heart Associat. (2019) 8:e014240. doi: 10.1161/JAHA.119.014240
11. Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, et al. Home-based cardiac rehabilitation: a scientific statement from the American association of cardiovascular and pulmonary rehabilitation, the American heart association, and the American college of cardiology. J Am Coll Cardiol. (2019) 74:133–53. doi: 10.1016/j.jacc.2019.03.008
12. Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. (2001) 37:153–6. doi: 10.1016/s0735-1097(00)01054-8
13. Chen YW, Wang CY, Lai YH, Liao YC, Wen YK, Chang ST, et al. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine. (2018) 97:e9629. doi: 10.1097/MD.0000000000009629
14. Everett B, Salamonson Y, Davidson PM. Bandura's exercise self-efficacy scale: validation in an Australian cardiac rehabilitation setting. Int J Nurs Stud. (2009) 46:824–9. doi: 10.1016/j.ijnurstu.2009.01.016
15. São-João TM, Rodrigues RCM, Gallani MCBJ, Miura CTdP, Domingues GdBL, Godin G. Cultural adaptation of the Brazilian version of the godin-shephard leisure-time physical activity questionnaire. Revista de saude publica. (2013) 47:479–87. doi: 10.1590/S0034-8910.2013047003947
16. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Critic Care Med. (2020) 166:111–7. doi: 10.1164/ajrccm.166.1.at1102
17. Kahraman BO, Ozsoy I, Akdeniz B, Ozpelit E, Sevinc C, Acar S. et al Test-retest reliability and validity of the timed up and go test and 30-second sit to stand test in patients with pulmonary hypertension. Int J Cardiol. (2020) 304:159–63. doi: 10.1016/j.ijcard.2020.01.028
18. ErkolInal E, Çarli AB, Çanak S, Aksu O, Köroglu BK, Savaş S. Effects of hyperthyroidism on hand grip strength and function. J Rehabil Res Dev. (2015) 52:663–8. doi: 10.1682/JRRD.2014.09.0221
19. Gurses HN, Zeren M, Kulli HD, Durgut E. The relationship of sit-to-stand tests with 6-minute walk test in healthy young adults. Medicine (2018) 97:e9489. doi: 10.1097/MD.0000000000009489
20. McCoy CE. Understanding the intention-to-treat principle in randomized controlled trials. West J Emerg Med. (2017) 18:1075-8. doi: 10.5811/westjem.2017.8.35985
21. Dorje T, Zhao G, Scheer A, Tsokey L, Wang J, Chen Y. SMARTphone and social media-based Cardiac Rehabilitation and Secondary Prevention (SMART-CR/SP) for patients with coronary heart disease in China: a randomised controlled trial protocol. BMJ Open (2018) 8:e021908. doi: 10.1136/bmjopen-2018-021908
22. Gremeaux V, Troisgros O, Benaïm S, Hannequin A, Laurent Y, Casillas JM, et al. Determining the minimal clinically important difference for the six-minute walk test and the 200-meter fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome. Arch Phys Med Rehabil. (2011) 92:611–9. doi: 10.1016/j.apmr.2010.11.023
23. Gayda M, Choquet D, Ahmaidi S. Effects of exercise training modality on skeletal muscle fatigue in men with coronary heart disease. J Electromyograph Kinesiol. (2009) 19:e32–9. doi: 10.1016/j.jelekin.2007.08.009
24. Chinese Society of Cardiology of Chinese Medical Association. Cardiovascular committee of chinese association of rehabilitation medicine, & committee of cardio-cerebral-vascular diseases of gerontological society of China. Chin J Cardiol. (2013) 41:267–75. doi: 10.3760/cma.j.issn.0253-3758.2013.04.003
25. Marzolini S, Oh PI, Brooks D. Effect of combined aerobic and resistance training versus aerobic training alone in individuals with coronary artery disease: a meta-analysis. Eur J Prevent Cardiol. (2012) 19:81–94. doi: 10.1177/1741826710393197
26. Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: A critical review of methods. J Sport Health Sci. (2016) 5:80–90. doi: 10.1016/j.jshs.2014.10.004
27. Kamiya K, Masuda T, Tanaka S, Hamazaki N, Matsue Y, Mezzani A. Quadriceps strength as a predictor of mortality in coronary artery disease. Am J Med. (2015) 128:1212–9. doi: 10.1016/j.amjmed.2015.06.035
28. Wang D, Yao J, Zirek Y, Reijnierse EM, Maier AB. Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle. (2020) 11:3–25. doi: 10.1002/jcsm.12502
29. Fujita E, Taaffe DR, Yoshitake Y, Kanehisa H. Repeated sit-to-stand exercise enhances muscle strength and reduces lower body muscular demands in physically frail elders. Exp Gerontol. (2019) 116:86–92. doi: 10.1016/j.exger.2018.12.016
30. Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, et al. Stevens, the Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess. (2007) 11:1–118. doi: 10.3310/hta11350
31. Gordon NF, English CD, Contractor AS, Salmon RD, Leighton RF, Franklin BA, et al. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. Am J Cardiol. (2002) 89:1263–8. doi: 10.1016/S0002-9149(02)02323-8
32. Oerkild B, Frederiksen M, Hansen JF, Simonsen L, Skovgaard LT, Prescott E. Home-based cardiac rehabilitation is as effective as centre-based cardiac rehabilitation among elderly with coronary heart disease: results from a randomised clinical trial. Age Ageing. (2011) 40:78–85. doi: 10.1093/ageing/afq122
33. Kraal JJ, Van den Akker-Van Marle ME, Abu-Hanna A, Stut W, Peek N, Kemps HM. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@Home study. Eur J Prev Cardiol. (2017) 24:1260–73. doi: 10.1177/2047487317710803
Keywords: coronary artery disease, percutaneous coronary intervention, cardiac rehabilitation, home-based, education, exercise, COVID-19
Citation: Li J, Liu B, Wang Z, El-Ansary D, Adams R, Han J and Meng S (2022) Efficacy of a 6-Week Home-Based Online Supervised Exercise Program Conducted During COVID-19 in Patients With Post Percutaneous Coronary Intervention: A Single-Blind Randomized Controlled Trial. Front. Cardiovasc. Med. 9:853376. doi: 10.3389/fcvm.2022.853376
Received: 12 January 2022; Accepted: 07 March 2022;
Published: 07 April 2022.
Edited by:
Yan Zhang, Peking University, ChinaReviewed by:
Christopher Kovacs, Western Illinois University, United StatesTakanori Yasu, Dokkyo Medical University, Japan
Anna Pieniazek, University of Łódz, Poland
Copyright © 2022 Li, Liu, Wang, El-Ansary, Adams, Han and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Han, jia.han@canberra.edu.au; Shu Meng, msdoctor@126.com
†These authors have contributed equally to this work
 Jiajia Li
Jiajia Li Bo Liu
Bo Liu Zheng Wang
Zheng Wang Doa El-Ansary1,3
Doa El-Ansary1,3  Roger Adams
Roger Adams Jia Han
Jia Han