Published online Dec 28, 2020. doi: 10.4329/wjr.v12.i12.289
Peer-review started: November 11, 2020
First decision: November 29, 2020
Revised: December 3, 2020
Accepted: December 8, 2020
Article in press: December 8, 2020
Published online: December 28, 2020
Influenza viruses were responsible for most adult viral pneumonia. Presently, coronavirus disease 2019 (COVID-19) has evolved into serious global pandemic. COVID-19 outbreak is expected to persist in months to come that will be synchronous with the influenza season. The management, prognosis, and protection for these two viral pneumonias differ considerably and differentiating between them has a high impact on the patient outcome. Reverse transcriptase polymerase chain reaction is highly specific but has suboptimal sensitivity. Chest computed tomography (CT) has a high sensitivity for detection of pulmonary disease manifestations and can play a key-role in diagnosing COVID-19. We reviewed 47 studies and delineated CT findings of COVID-19 and influenza pneumonia. The differences observed in the chest CT scan can be helpful in differentiation. For instance, ground glass opacities (GGOs), as the most frequent imaging finding in both diseases, can differ in the pattern of distribution. Peripheral and posterior distribution, multilobular distribution, pure or clear margin GGOs were more commonly reported in COVID-19, whereas central or peri-bronchovascular GGOs and pure consolidations were more seen in influenza A (H1N1). In review of other imaging findings, further differences were noticed. Subpleural curvilinear lines, sugar melted sign, intra-lesional vascular enlargement, reverse halo sign, and fibrotic bands were more reported in COVID-19 than H1N1, while air space nodule, tree-in-bud, bronchiectasia, pleural effusion, and cavitation were more seen in H1N1. This delineation, when combined with clinical manifestations and laboratory results may help to differentiate these two viral infections.
Core Tip: Co-incidence of coronavirus disease 2019 (COVID-19) and influenza in the influenza season can be challenging for the health system. The management, prognosis, and protection for these two viral pneumonias differ considerably. Chest computed tomography (CT) has a high sensitivity for detection of pulmonary disease manifestations and can be helpful in diagnosing COVID-19. In this review, we made a comparative study of CT findings in COVID-19 and influenza A pneumonia, as well as their clinical manifestations, by a thorough review of literature. Delineation of differences observed in the chest CT scan of COVID-19 and influenza can be helpful in differentiation.
- Citation: Eslambolchi A, Maliglig A, Gupta A, Gholamrezanezhad A. COVID-19 or non-COVID viral pneumonia: How to differentiate based on the radiologic findings? World J Radiol 2020; 12(12): 289-301
- URL: https://www.wjgnet.com/1949-8470/full/v12/i12/289.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i12.289
Community-acquired pneumonia is a major public health concern, as it is the most common infectious disease worldwide and a significant cause of morbidity and mortality[1]. Although bacteria have been a major cause of pneumonia in adults[2], respiratory viruses are increasingly implicated recently. In some instances, they are found to be higher in incidence than bacterial etiologies[3]. Prior to the emergence of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), influenza virus was the most common cause of viral pneumonia in adults. It has been an important health challenge of recent history[4,5]. Influenza type A (H1N1) is the most common type of influenza viruses. It is also the most significant in terms of morbidity and mortality in the general population[6].
In late December 2019, a new viral pneumonia emerged in China that rapidly disseminated worldwide. On February 11, 2020, the International Committee on Taxonomy of Viruses termed this new variant, SARS-CoV-2 and World Health Organization (WHO) labelled the disease caused by this virus as corona virus disease of 2019 (COVID-19 virus)[7]. WHO designated this outbreak a public health emergency of international concern on January 30, 2020, and declared it as a global pandemic on March 11, 2020[8].
The COVID-19 outbreak is ongoing and is expected to persist a period more than a year. There is evidence that it may wax and wane, with a new incidence rise in late fall and winter months within temperate regions[9]. This timing will coincide with influenza season. Upper and lower respiratory infections due to influenza virus will also loom again in the form of common cold, pneumonias, and possible unpredictable epidemics in the next few months. This can be overwhelming, particularly for healthcare systems in resource-limited contexts[10]. Public health officials and clinicians, therefore, will be compelled to differentiate pneumonia caused by COVID-19 and influenza viruses. The impact of intercurrent infection of two viral pneumonias due to simultaneous seasonal peak occurrences in some individuals raises great concern[11,12].
Although clinical manifestations of these two respiratory viruses may have similarities, the approach with respect to health care worker precautions, treatment, and prognosis are different. Reverse transcriptase polymerase chain reaction (RT-PCR) with high specificity, is now the confirmatory and reference standard for COVID-19 diagnosis; this method is also highly accurate for detecting influenza[13]. However, suboptimal test sensitivity for COVID-19 has led to false negative results, failure to detect infected patients, and created challenges in decision making for suspected cases[14]. Studies have shown that chest computed tomography (CT) with its high sensitivity and availability can play a key role in diagnosing COVID-19, particularly in the early stages of the disease when even RT-PCR can be negative[15-17]. However, resources comparing chest CT findings of COVID-19 and influenza pneumonia, in search of differentiating characteristics of each, are of great scarcity. Therefore, given the emerging role of imaging in diagnosis of these novel viral infections with low reliability of clinical symptoms, and sub-optimal performance of RT-PCR, we have explored the added benefit of chest CT in better differentiation of COVID-19 and influenza pneumonia.
Pulmonary infection with different viruses usually demonstrates common symptoms particularly in the early stages of the disease[11], although signs and symptoms can vary between individual patients. Clinical manifestations are diverse but have considerable overlap. In the Wang et al[18] comparison of the symptoms of COVID-19 and influenza pneumonia, the most common clinical manifestations were fever, cough, and malaise. Other frequently reported symptoms were sputum production, rhinorrhea, dyspnea, headache, nausea and vomiting, chest pain, fatigue, sore throat, and diarrhea[19]. Although the range of symptoms in COVID-19 and H1N1 are similar, the fraction of patients with severe disease differs significantly and the proportion of severe and critical infection in COVID-19 is higher than anticipated for influenza infection. In COVID-19, 80% of infections are asymptomatic or mild, 15% are severe, requiring oxygen therapy and 5% are critical, requiring ventilation aid[19]. As the signs and symptoms of either influenza or COVID-19 pulmonary disease cannot be used with sufficient confidence to confirm a specific viral etiology, health care providers are challenged to make a timely diagnosis for effective management. Clinical characteristics of patients with COVID-19 and Influenza are summarized
| COVID-19 | H1N1 | |
| Fever | ++++ | ++++ |
| Cough | +++ | ++++ |
| Myalgia | ++ | ++ |
| Fatigue | ++ | ++ |
| Sputum | ++ | ++ |
| Rhinorrhea | + | ++ |
| Dyspnea | ++ | ++ |
| Headache | ++ | + |
| Nausea & Vomit | + | + |
| Chest pain | + | + |
| Sore throat | + | ++ |
| Diarrhea | + | + |
| Hemoptysis | + | + |
| Skin lesions | Erythematous rash, urticarial, chickenpox-like vesicles (+)[28] | Maculopapular (+)[29] |
| Conjunctivitis | +[30] | +[31] |
| Other eyes lesions | - | Sub conjunctival hemorrhage, uveal affection, retinopathy, and optic neuritis (+)[32] |
| Anosmia, hyposmia | +/++[33,34] | +[35] |
| Ageusia, dysgeusia (loss of taste) | +[34] | +[36] |
| Transmission interval | 5-6 d | 3 d |
| Reproductive number | 2.2 | 1.3-1.7 |
Traditionally, diagnosis of viral pneumonia has been based on evaluation of respiratory tract samples and detection of the virus or its antigens by culture or immunofluorescence microscopy. Measurement of the antibodies in patients’ serum has been another useful diagnostic method. Invention of PCR has enhanced the power of detection of the causative factor of viral pneumonia[37]. Although various PCR methods such as RT, quantitative, or real time are the most specific methods for diagnosis of viral pneumonia, their sensitivity is not optimal for all viruses (e.g., 79% for COVID-19)[38].
Recent studies have shown that chest CT with high sensitivity is a helpful modality in the early identification of pneumonia. Combination of PCR and chest CT can improve the sensitivity and specificity for diagnosing clinically suspected cases. Additionally, radiation dose can be decreased - particularly for children and pregnant women[14,18,39] - with low radiation dose protocols with greater than 50% decrease in ionizing radiation exposure and no significant impact on the diagnostic assessment[40].
Prior to the emergence of the new SARS-CoV-2 virus, other known viruses were among common causes of respiratory tract infection. In immunocompetent adults, influenza virus and human parainfluenza virus (HPIV) were the most common, followed by adenovirus and respiratory syncytial virus (RSV). In immunocompetent children, RSV and HPIV were the most common causative agents for viral pneumonia, followed by parainfluenza and human metapneumovirus (HMPV)[6].
In addition to RT-PCR, serologic tests are also helpful in supporting the diagnosis of H1N1 pneumonia. Increased levels of C-reactive protein (CRP), serum lactate dehydrogenase (LDH, can reach more than 1000 IU/L and is correlated with the severity of disease), and creatine kinase are reported in H1N1. Lymphopenia, thrombocytopenia, and elevated level of transaminase can also occur[41]. Similarly in COVID-19, increased level of CRP, LDH, aspartate aminotransferase and alanine aminotransferase, and lymphopenia has been reported[42]. In imaging-based diagnosis, viral pneumonias generally show more diffuse and bilateral pattern of involvement with greater preponderance of interstitial findings when compared to bacterial pneumonias. The latter more commonly demonstrate unilateral, segmental, or lobar consolidations, limited by pleural surfaces, centrilobular nodules, bronchial wall thickening and mucus impaction[43]. Viral agents have similar virulence factors and underlying mechanism of invasion by causing alveolar and bronchiolar injury, hemorrhage and inflammatory responses that lead to interstitial cellular infiltration, and edema. The radiologic features of viral pneumonia also demonstrate similarities concomitant with their similar means of pathogenesis.
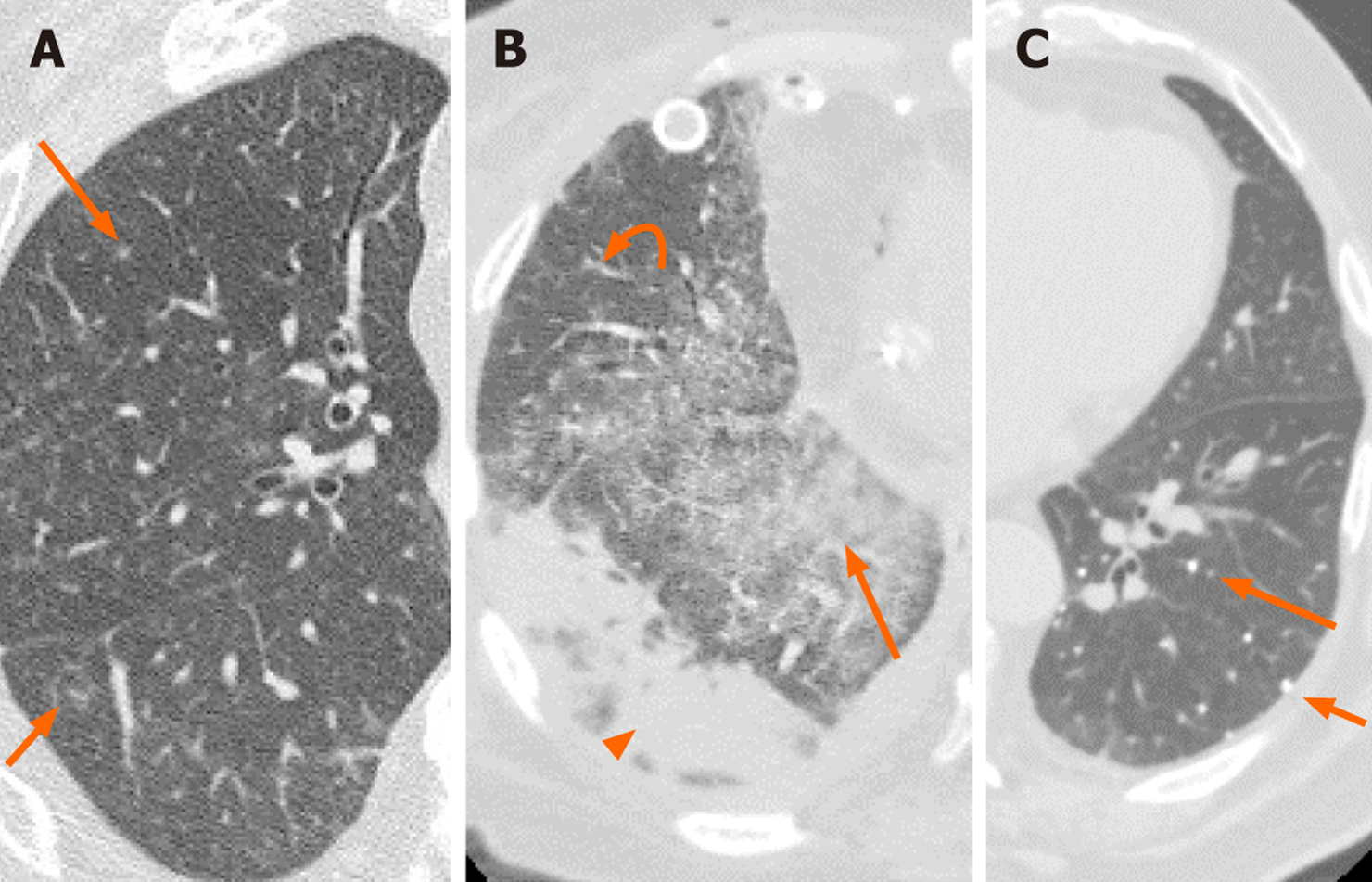
The main CT findings of viral pneumonia include changes in pulmonary parenchymal density with areas of ground glass opacity (GGO) or consolidation, nodular, or micro nodular opacities, sometimes with tree-in-bud pattern, reticular opacities as inter- or intra-lobular septal thickening and signs of bronchiolar inflammation as evidenced by increased thickness of bronchial wall[44]. However, some viral infections may have some distinctive features in chest imaging. For example, adenovirus invades terminal bronchioles causing bronchopneumonia. Cytomegalovirus leads to acute interstitial pneumonia with diffuse edema and alveolar exudate, exhibiting diffuse GGOs and interstitial reticular opacities or may exhibit nodular infiltration (Figure 1). Herpes simplex virus invades both the airways and alveoli leading to multifocal scattered airspace opacities and consolidations mainly in peribronchial distribution (Figure 2)[6]. Varicella-zoster virus exhibits well defined or ill- defined tiny nodules with or without surrounding halo or patchy bilateral GGOs. On the healing process, the lesions can calcify and persist as randomly scattered calcified nodules (Figure 1). However, this appearance is not specific and, in appropriate clinical context, can be seen with various other conditions, such as pulmonary hemosiderosis, Goodpasture syndrome, silicosis, pulmonary alvelolar microlithiasis, and in some calcified metastasis, such as osteosarcoma[6,44,45].
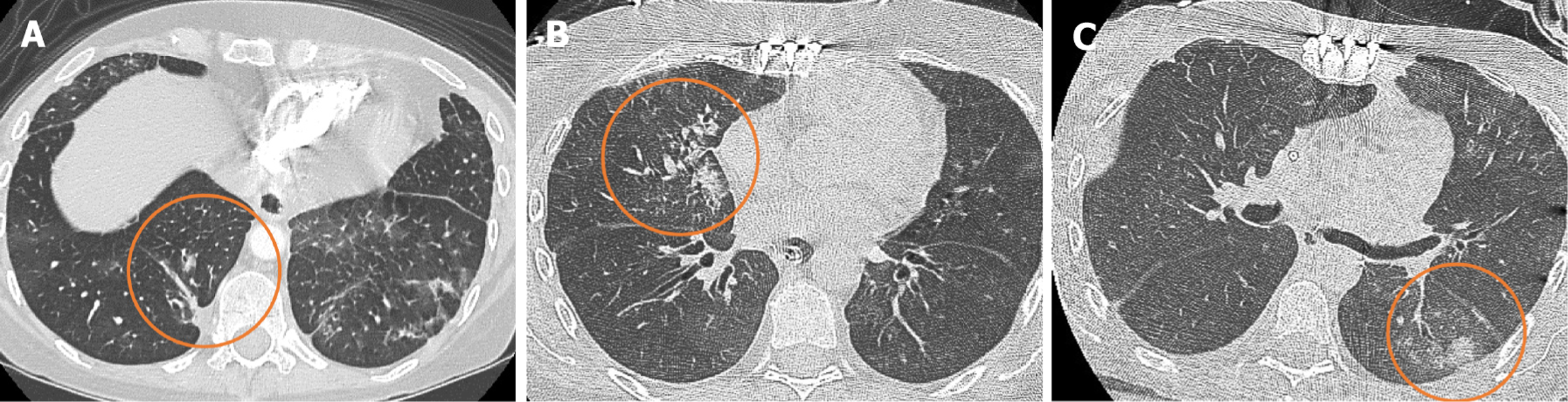
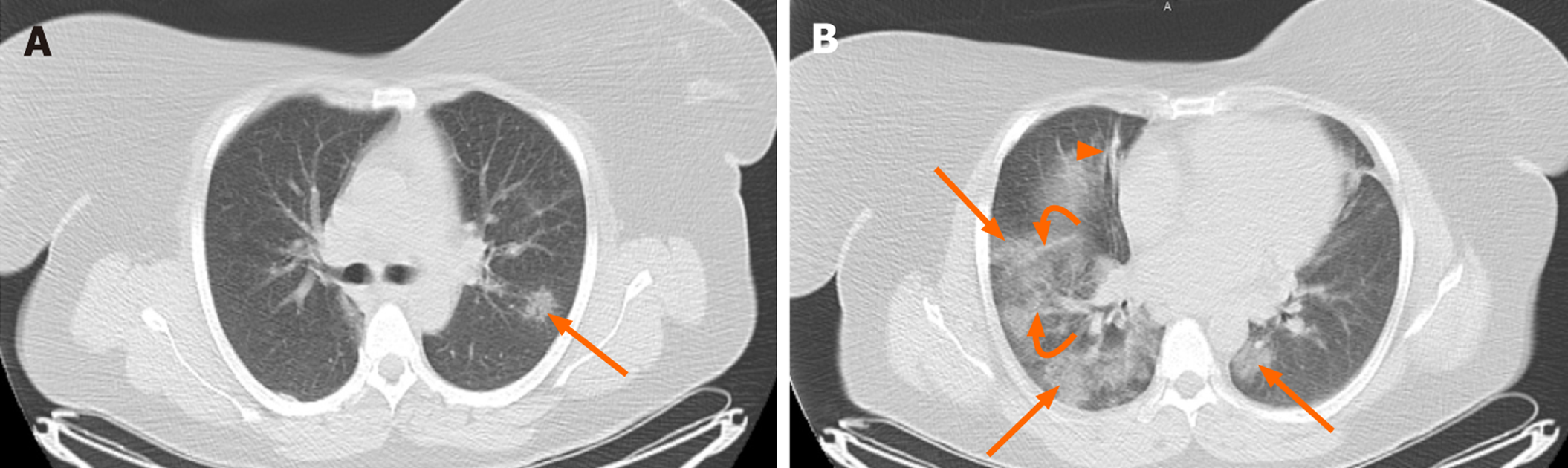
Chest CT features of HPIV, RSV, and HMPV can be similar and include multifocal patchy GGOs, consolidation, centrilobular nodules, and bronchial wall thickening. Influenza virus usually involves lung parenchyma extensively, leading to diffuse and multifocal parenchymal lesions[6,46]. Influenza pneumonia can be classified into different types based on parenchymal changes that include interstitial pneumonia with patchy GGOs and interlobular septal thickening as the main findings; bron-chopneumonia with multifocal consolidations more along the bronchovascular bundles; and an uncommon type histologically consistent with cryptogenic organizing pneumonia (COP)[47]. Diffuse parenchymal damage can be indicated by peribronchovascular interstitial thickening and air space or centrilobular nodules; the latter may demonstrate the “tree-in-bud” pattern that is usually associated with small airways disease and/or endobronchial spread of disease. Bronchial wall thickening and centrilobular nodules (including tree-in-bud) are signs of bronchiolitis or bronchitis; GGOs, consolidations, and crazy-paving (thick septal line over areas of GGOs or consolidation) pattern indicate parenchymal involvement of pneumonia[48]. Although there is no specific CT for diagnosing H1N1, the main suggestive findings are scattered lung consolidations, GGOs, or both in a z or peripheral distributing pattern, air bronchograms, and septal thickening (Figure 3)[49]. Crazy paving, halo sign (GGO surrounding a consolidation), nodules, irregular lines of fibrotic change associated bronchiectasis, round mass-like opacity, pleural effusion, and adenopathy are more uncommon findings[50,51].
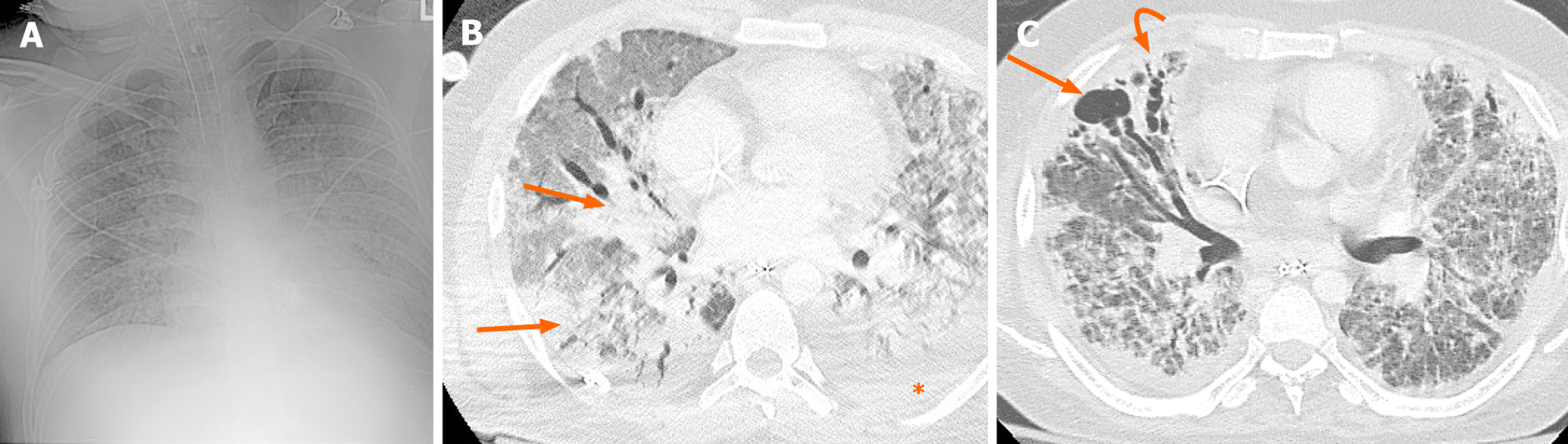
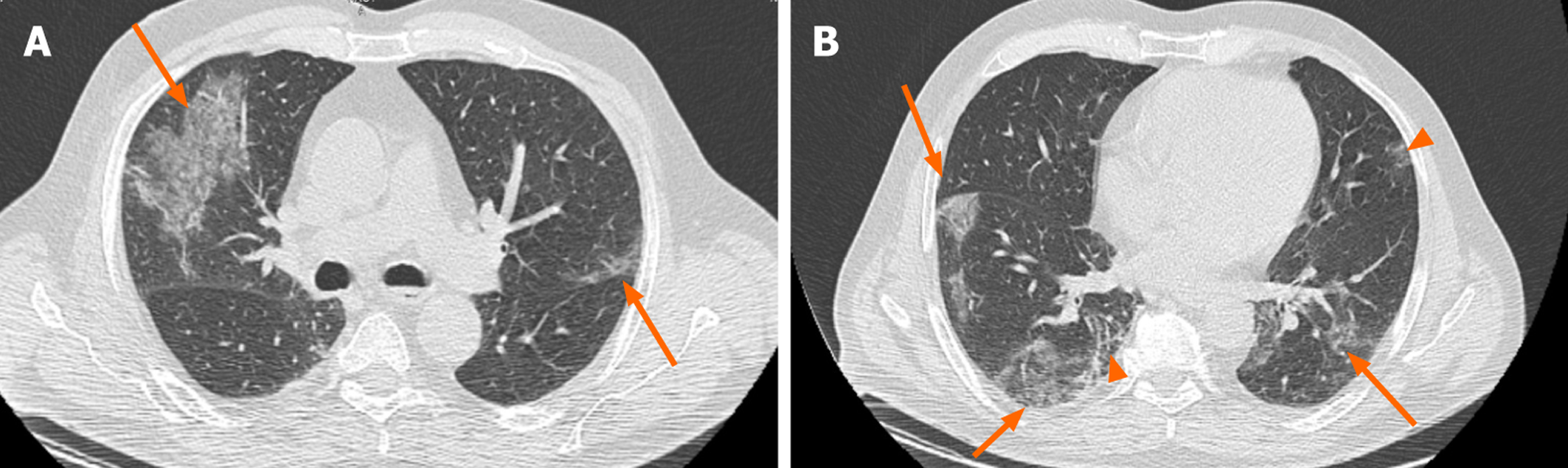
In COVID-19 pneumonia, the main CT features are pure GGOs, GGO with superimposed consolidation, bronchiolar wall thickening, rounded opacities, and interlobular septal thickening (Figure 4-6). GGOs, as the most frequent finding, are mainly seen as bilateral and multifocal opacities, with peripheral and posterior distribution. Pure consolidations are less common and can be seen later in the course of the disease or in older ages[43,52,53].
By reviewing the literature and comparing CT findings of COVID-19 and H1N1 pneumonia, the following information was extracted and charted in Table 2; important differences are annotated (1). Although both infections commonly involve multiple lobes bilaterally, GGOs were more common in patents with COVID-19, while consolidations were more common in H1N1. In COVID-19, mainly peripheral and posterior zones were involved, whereas in H1N1 pneumonia, the pattern of involvement was more diffuse with both central and peripheral involvement. It is noteworthy that in the advanced stage of COVID 19 infection, the imaging findings become non-specific and indistinguishable from other pneumonias.
| COVID-19 | H1N1 | |
| GGO | ++++ | +++/++++ |
| Unilateral distribution | -/+ (++ in asymptomatic patients) | + |
| Bilateral distribution | ++++ | +++/++++ |
| Posterior distribution1 | ++++ | N/A |
| Peripheral distribution1 | +++/++++ | ++ |
| Multi-lobar distribution | ++++ | +++ |
| Mixed (peripheral and central) distribution | ++ | +++ |
| Pure GGO1 | ++/+++ | +/++ |
| Clear margin GGO | ++ | + |
| Cluster GGOs around bronchial tree1 | + | +++ |
| Patchy GGO | +++ | ++ |
| GGO with consolidation | ++/+++ | +++ |
| Pure consolidation | +/++ | ++/+++ |
| Reticulation (linear opacities) | ++/+++ | ++/+++ |
| Subpleural curvilinear line1 | + | N/A |
| Rounded opacities | ++ | ++ |
| Crazy paving | ++ | +/++ |
| Halo sign | -/+ | -/+ |
| Air space nodules1 | + | +/++ |
| Tree-in-bud1 | -/+ | ++ |
| Air bronchogram | +/++ (in later stages) | ++ |
| Interstitial septal thickening | +/++ (increased in later stages) | +/++ |
| Bronchiolar wall thickening | ++ | +/++ |
| Pleural effusion1 | -/+ | ++ |
| White lung (ARDS) | +/++ | +/++ in general (+ in mild, ++ in moderate and+++ in severe influenza) |
| Fibrotic bands | +/++ (in late stages) | + (++ for H7N9) |
| Melted sugar sign1 | ++ | N/A |
| Air way secretions | -/+ | N/A |
| Lymphadenopathy | + | + |
| Bronchiectasis | -/+ | + |
| Intra-lesional vascular enlargement1 | ++/+++ | N/A |
| Bronchial wall thickening | + | + |
| Focal pleural thickening | +/++ | +/++ |
| Pericardial effusion | -/+ | -/+ |
| Bronchiectasis | -/+ | + |
| Reverse halo sign | + | -/+ |
| Pneumothorax | -/+ | -/+ |
| Cavitation | - | -/+ |
The incidence of air space nodules ranges widely in reviewed studies. However, most studies demonstrated that air space nodules and tree-in-bud nodules (as clustered 1-4 mm nodules with a linear branching pattern) were more frequently seen in H1N1. Some combination of simultaneous findings can be more suggestive for each. For example, pure GGOs, interlobular septal thickening, and the absence of nodules and pleural effusions were more suggestive of COVID-19[43,53]. The incidence of interlobular septal thickening was equivocal in the reviewed literature. These findings were more commonly reported in COVID-19 than H1N1. The discrepant incidence of interlobular septal thickenings has been postulated to reflect evaluation of patients in different stages of disease. Interstitial disease appears to present in latter and more advanced stages of disease[18,54,55]. Subsegmental vascular enlargement is a unique and not uncommon finding observed COVID-19 patients. This finding is not greatly reported in H1N1 pneumonia. Therefore, its appearance may be more specific for COVID-19, especially if observed with imaging manifestations that support a diagnosis of COVID-19[54,56].
Another non-specific CT finding is interstitial thickening within areas of GGOs - the “crazy paving” disease pattern, which was more reported in COVID-19 patients[57]. Reticular opacities refer to opacification in or around interstitial septal structures[58]. Causes of interstitial thickening include edema, fibrosis, and other parenchymal opacification around septal lines (including GGOs) can cause reticular opacifications. This definition may explain why the reviewed literature report more linear opacities than septal thickening in COVID-19 patients. However, this finding is not an uncommon finding in H1N1 as well. Fibrotic lines with appearance of linear opacities were reported at a higher rate at the third week after H1N1 pneumonia; these findings can resolve slowly over time[59].
Reverse halo sign (consolidation surrounding central GGO was reported previously in few infectious diseases such as TB, invasive pulmonary aspergillosis, Pneumocystis jiroveci pneumonia, histoplasmosis, and cryptococcosis or in non-infectious granulomatosis diseases such as sarcoidosis, granulomatosis with polyangiitis, and COP[60]. This CT sign is also reported in COVID-19 patients. In a study by Zhao et al[61] the reverse halo sign was observed in 25.2% of COVID-19 patients. Such finding suggests that organizing pneumonia can be one of the mechanisms for parenchymal damage in COVID-19[62]. This finding was reported in relatively fewer cases of H1N1[63]. It is not uncommon for consolidations in both COVID-19 and H1N1 to present as a round opacity. In few studies the incidence of round opacity was slightly higher in COVID-19 than H1N1[64,65]. In a study by Liu et al[22] the combination of round opacity with absence of nodule was significantly more in COVID-19 than in H1N1. They found some other statistically significant combination of CT findings in favor of COVID-19 included the presence of pure GGO with absence of nodules; GGO and septal thickening; septal thickening and absence of nodules; and the combined presence of rounded opacities, septal thickening, and the absence of pleural effusion.
In a follow up evaluation of patients with H1N1, evidence of traction bronchiectasis was reported in some cases in the regions of previous consolidation suggestive of fibrotic changes[66]. This finding appears to be rare in COVID-19, although it was reported in few cases[15]. No cavitation has been reported in COVID-19 patients thus far; these are rarely reported in influenza, especially in more severe forms of avian influenza (H5N1). Cavitation was described in a case report of an immuno-compromised patient with H1N1[44,67].
Focal pleural thickening in the setting of other suggestive COVID-19 findings is not uncommon; however, pleural effusion is an atypical finding for COVID-19. Pleural effusions have been reported in some H1N1 patients[56]. Mediastinal lymphadenopathy is an atypical finding in both COVID and H1N1; however, it was more reported in influenza especially in younger ages and in children[68-71]. Pneumothorax is a rare finding in both COVID-19 and H1N1[72,73]. Just few cases with this finding as the complication of COVID-19 or during recovery phase of H1N1 have been reported in literature[74-77].
COVID-19 and influenza pneumonia have relatively similar clinical manifestations. However, the precautions required of the public and health workers to prevent transmission, the disease management protocols, and prognosis are quite different. Therefore, differentiating COVID-19 and influenza pneumonia is important in the early stages of the infection for a well-timed and appropriate management plan. There are imaging features of influenza and COVID-19 that sufficiently differ such that the two may be distinguishable. However, even in cases where CT findings have overlap, the addition of clinical history, lab data (including RT-PCR) has potential to improve diagnostic accuracy.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tan CH S-Editor: Huang P L-Editor: A P-Editor: Zhang YL
| 1. | Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095-2128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9500] [Cited by in F6Publishing: 9076] [Article Influence: 756.3] [Reference Citation Analysis (0)] |
| 2. | National Heart, Lung, and Blood Institute. Pneumonia. 2020 [cited 2020 June 3]. In: Nhlbi.nih.gov [Internet]. Available from: https://www.nhlbi.nih.gov/health-topics/pneumonia. [Cited in This Article: ] |
| 3. | Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM, Chappell JD, Qi C, Hart EM, Carroll F, Trabue C, Donnelly HK, Williams DJ, Zhu Y, Arnold SR, Ampofo K, Waterer GW, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, McCullers JA, Pavia AT, Edwards KM, Finelli L; CDC EPIC Study Team. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med. 2015;373:415-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1370] [Cited by in F6Publishing: 1482] [Article Influence: 164.7] [Reference Citation Analysis (0)] |
| 4. | Dandachi D, Rodriguez-Barradas MC. Viral pneumonia: etiologies and treatment. J Investig Med. 2018;66:957-965. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Sullivan CJ, Jordan MC. Diagnosis of viral pneumonia. Semin Respir Infect. 1988;3:148-161. [Cited in This Article: ] |
| 6. | Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT Features of Viral Pneumonia. Radiographics. 2018;38:719-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 382] [Cited by in F6Publishing: 386] [Article Influence: 64.3] [Reference Citation Analysis (0)] |
| 7. | Wu Y, Ho W, Huang Y, Jin DY, Li S, Liu SL, Liu X, Qiu J, Sang Y, Wang Q, Yuen KY, Zheng ZM. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395:949-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 208] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 8. | World Health Organization. WHO Timeline - COVID-19. 2020 [cited 2020 May 21]. Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline-covid-19. [Cited in This Article: ] |
| 9. | Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A. Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19). JAMA Netw Open. 2020;3:e2011834. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 359] [Article Influence: 89.8] [Reference Citation Analysis (0)] |
| 10. | Li Q, Tang B, Bragazzi NL, Xiao Y, Wu J. Modeling the impact of mass influenza vaccination and public health interventions on COVID-19 epidemics with limited detection capability. Math Biosci. 2020;325:108378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 11. | Ding Q, Lu P, Fan Y, Xia Y, Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020;92:1549-1555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 238] [Cited by in F6Publishing: 274] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 12. | Khodamoradi Z, Moghadami M, Lotfi M. Co-infection of Coronavirus Disease 2019 and Influenza A: A Report from Iran. Arch Iran Med. 2020;23:239-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 13. | Maignan M, Viglino D, Hablot M, Termoz Masson N, Lebeugle A, Collomb Muret R, Mabiala Makele P, Guglielmetti V, Morand P, Lupo J, Forget V, Landelle C, Larrat S. Diagnostic accuracy of a rapid RT-PCR assay for point-of-care detection of influenza A/B virus at emergency department admission: A prospective evaluation during the 2017/2018 influenza season. PLoS One. 2019;14:e0216308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3542] [Cited by in F6Publishing: 3187] [Article Influence: 796.8] [Reference Citation Analysis (0)] |
| 15. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020;30:4930-4942. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 101] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 16. | Huang EP, Sung CW, Chen CH, Fan CY, Lai PC, Huang YT. Can computed tomography be a primary tool for COVID-19 detection? Crit Care. 2020;24:193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115-E117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2088] [Cited by in F6Publishing: 1809] [Article Influence: 452.3] [Reference Citation Analysis (2)] |
| 18. | Wang H, Wei R, Rao G, Zhu J, Song B. Characteristic CT findings distinguishing 2019 novel coronavirus disease (COVID-19) from influenza pneumonia. Eur Radiol. 2020;30:4910-4917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 19. | Yang Y, Sugimoto JD, Halloran ME, Basta NE, Chao DL, Matrajt L, Potter G, Kenah E, Longini IM Jr. The transmissibility and control of pandemic influenza A (H1N1) virus. Science. 2009;326:729-733. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 413] [Cited by in F6Publishing: 416] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 20. | Jiang C, Yao X, Zhao Y, Wu J, Huang P, Pan C, Liu S, Pan C. Comparative review of respiratory diseases caused by coronaviruses and influenza A viruses during epidemic season. Microbes Infect. 2020;22:236-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 21. | Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin Imaging. 2020;66:35-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 176] [Cited by in F6Publishing: 172] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 22. | Liu M, Zeng W, Wen Y, Zheng Y, Lv F, Xiao K. COVID-19 pneumonia: CT findings of 122 patients and differentiation from influenza pneumonia. Eur Radiol. 2020;30:5463-5469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 23. | Niu S, Tian S, Lou J, Kang X, Zhang L, Lian H, Zhang J. Clinical characteristics of older patients infected with COVID-19: A descriptive study. Arch Gerontol Geriatr. 2020;89:104058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 159] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 24. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32663] [Cited by in F6Publishing: 28495] [Article Influence: 7123.8] [Reference Citation Analysis (3)] |
| 25. | Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK, Franco-Paredes C, Henao-Martinez AF, Paniz-Mondolfi A, Lagos-Grisales GJ, Ramírez-Vallejo E, Suárez JA, Zambrano LI, Villamil-Gómez WE, Balbin-Ramon GJ, Rabaan AA, Harapan H, Dhama K, Nishiura H, Kataoka H, Ahmad T, Sah R; Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Electronic address: https://www.lancovid.org. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1542] [Cited by in F6Publishing: 1374] [Article Influence: 343.5] [Reference Citation Analysis (0)] |
| 26. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13871] [Cited by in F6Publishing: 12369] [Article Influence: 3092.3] [Reference Citation Analysis (1)] |
| 27. | Bai L, Gu L, Cao B, Zhai XL, Lu M, Lu Y, Liang LR, Zhang L, Gao ZF, Huang KW, Liu YM, Song SF, Wu L, Yin YD, Wang C. Clinical features of pneumonia caused by 2009 influenza A(H1N1) virus in Beijing, China. Chest. 2011;139:1156-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212-e213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 634] [Cited by in F6Publishing: 786] [Article Influence: 196.5] [Reference Citation Analysis (1)] |
| 29. | Lee HJ, Shin DH, Choi JS, Kim KH. Leukocytoclastic vasculitis associated with influenza A virus infection. J Korean Med Sci. 2012;27:1601-1603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Seah IYJ, Anderson DE, Kang AEZ, Wang L, Rao P, Young BE, Lye DC, Agrawal R. Assessing Viral Shedding and Infectivity of Tears in Coronavirus Disease 2019 (COVID-19) Patients. Ophthalmology. 2020;127:977-979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 275] [Cited by in F6Publishing: 287] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 31. | Belser JA, Lash RR, Garg S, Tumpey TM, Maines TR. The eyes have it: influenza virus infection beyond the respiratory tract. Lancet Infect Dis. 2018;18:e220-e227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 32. | Mansour DE, El-Shazly AA, Elawamry AI, Ismail AT. Comparison of ocular findings in patients with H1N1 influenza infection versus patients receiving influenza vaccine during a pandemic. Ophthalmic Res. 2012;48:134-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Reinhard A, Ikonomidis C, Broome M, Gorostidi F. [Anosmia and COVID-19]. Rev Med Suisse. 2020;16:849-851. [PubMed] [Cited in This Article: ] |
| 34. | Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and Ageusia: Common Findings in COVID-19 Patients. Laryngoscope. 2020;130:1787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 378] [Cited by in F6Publishing: 449] [Article Influence: 112.3] [Reference Citation Analysis (0)] |
| 35. | de Haro-Licer J, Roura-Moreno J, Vizitiu A, González-Fernández A, González-Ares JA. Long term serious olfactory loss in colds and/or flu. Acta Otorrinolaringol Esp. 2013;64:331-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Henkin RI, Larson AL, Powell RD. Hypogeusia, dysgeusia, hyposmia, and dysosmia following influenza-like infection. Ann Otol Rhinol Laryngol. 1975;84:672-682. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 84] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 37. | Ruuskanen O, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011;377:1264-1275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 786] [Cited by in F6Publishing: 756] [Article Influence: 58.2] [Reference Citation Analysis (0)] |
| 38. | He JL, Luo L, Luo ZD, Lyu JX, Ng MY, Shen XP, Wen Z. Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19) patients outside Wuhan, China. Respir Med. 2020;168:105980. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 155] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 39. | Hu L, Wang C. Radiological role in the detection, diagnosis and monitoring for the coronavirus disease 2019 (COVID-19). Eur Rev Med Pharmacol Sci. 2020;24:4523-4528. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 10] [Reference Citation Analysis (0)] |
| 40. | Tofighi S, Najafi S, Johnston SK, Gholamrezanezhad A. Low-dose CT in COVID-19 outbreak: radiation safety, image wisely, and image gently pledge. Emerg Radiol. 2020;27:601-605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 41. | Amorim VB, Rodrigues RS, Barreto MM, Zanetti G, Hochhegger B, Marchiori E. Influenza A (H1N1) pneumonia: HRCT findings. J Bras Pneumol. 2013;39:323-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Mardani R, Ahmadi Vasmehjani A, Zali F, Gholami A, Mousavi Nasab SD, Kaghazian H, Kaviani M, Ahmadi N. Laboratory Parameters in Detection of COVID-19 Patients with Positive RT-PCR; a Diagnostic Accuracy Study. Arch Acad Emerg Med. 2020;8:e43. [PubMed] [Cited in This Article: ] |
| 43. | Hani C, Trieu NH, Saab I, Dangeard S, Bennani S, Chassagnon G, Revel MP. COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101:263-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 231] [Cited by in F6Publishing: 248] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 44. | Franquet T. Imaging of pulmonary viral pneumonia. Radiology. 2011;260:18-39. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 239] [Cited by in F6Publishing: 252] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 45. | Khan AN, Al-Jahdali HH, Allen CM, Irion KL, Al Ghanem S, Koteyar SS. The calcified lung nodule: What does it mean? Ann Thorac Med. 2010;5:67-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 46. | Kim MC, Kim MY, Lee HJ, Lee SO, Choi SH, Kim YS, Woo JH, Kim SH. CT findings in viral lower respiratory tract infections caused by parainfluenza virus, influenza virus and respiratory syncytial virus. Medicine (Baltimore). 2016;95:e4003. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 47. | Fujita J, Bandoh S, Yamaguchi M, Higa F, Tateyama M. Chest CT findings of influenza virus-associated pneumonia in 12 adult patients. Influenza Other Respir Viruses. 2007;1:183-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 48. | Rodrigues RS, Marchiori E, Bozza FA, Pitrowsky MT, Velasco E, Soares M, Salluh JI. Chest computed tomography findings in severe influenza pneumonia occurring in neutropenic cancer patients. Clinics (Sao Paulo). 2012;67:313-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 49. | Marchiori E, Zanetti G, D'Ippolito G, Verrastro CG, Meirelles GS, Capobianco J, Rodrigues RS. Swine-origin influenza A (H1N1) viral infection: thoracic findings on CT. AJR Am J Roentgenol. 2011;196:W723-W728. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 50. | Rostami M, Javadi AA, Khorvash F, Mostafavizadeh K, Adibi A, Babak A, Ataei B, Meidani M, Naeini AE, Salehi H, Avijgan M, Yazdani MR, Rezaei F. Thoracic computerized tomographic (CT) findings in 2009 influenza A (H1N1) virus infection in Isfahan, Iran. J Res Med Sci. 2011;16:591-597. [PubMed] [Cited in This Article: ] |
| 51. | Abbo L, Quartin A, Morris MI, Saigal G, Ariza-Heredia E, Mariani P, Rodriguez O, Muñoz-Price LS, Ferrada M, Ramee E, Rosas MI, Gonzalez IA, Fishman J. Pulmonary imaging of pandemic influenza H1N1 infection: relationship between clinical presentation and disease burden on chest radiography and CT. Br J Radiol. 2010;83:645-651. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 52. | Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447-451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 272] [Cited by in F6Publishing: 275] [Article Influence: 68.8] [Reference Citation Analysis (0)] |
| 53. | Tang X, Du RH, Wang R, Cao TZ, Guan LL, Yang CQ, Zhu Q, Hu M, Li XY, Li Y, Liang LR, Tong ZH, Sun B, Peng P, Shi HZ. Comparison of Hospitalized Patients With ARDS Caused by COVID-19 and H1N1. Chest. 2020;158:195-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 235] [Cited by in F6Publishing: 220] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 54. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 769] [Cited by in F6Publishing: 822] [Article Influence: 205.5] [Reference Citation Analysis (0)] |
| 55. | Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425-434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2493] [Cited by in F6Publishing: 2226] [Article Influence: 556.5] [Reference Citation Analysis (0)] |
| 56. | Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, Guido G, Bracci B, De Dominicis C, Laghi A. Chest CT Features of COVID-19 in Rome, Italy. Radiology. 2020;296:E79-E85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 391] [Cited by in F6Publishing: 368] [Article Influence: 92.0] [Reference Citation Analysis (0)] |
| 57. | Yang W, Sirajuddin A, Zhang X, Liu G, Teng Z, Zhao S, Lu M. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol. 2020;30:4874-4882. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 165] [Article Influence: 41.3] [Reference Citation Analysis (0)] |
| 58. | Bell DJ, Jones J. Reticular and linear pulmonary opacification. 2020 [cited 2020 December 2]. In: Radiopaedia [Internet]. Available from: https://radiopaedia.org/articles/reticular-and-linear-pulmonary-opacification?lang=us. [Cited in This Article: ] |
| 59. | Li P, Zhang JF, Xia XD, Su DJ, Liu BL, Zhao DL, Liu Y, Zhao DH. Serial evaluation of high-resolution CT findings in patients with pneumonia in novel swine-origin influenza A (H1N1) virus infection. Br J Radiol. 2012;85:729-735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Marchiori E, Zanetti G, Hochhegger B. Reversed halo sign. J Bras Pneumol. 2015;41:564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 61. | Zhao HF, Liang T, Wu CC, Jin C, Liu Z, Wang Y, Liu Y, Li H, Wang ZK, Zhou J, Liang YK, Zhou HP, Wang XB, Ren ZQ, Yang J. The Reversed Halo Sign in COVID-19 Pneumonia. 2020. Preprint. Available from: Research Square. [DOI] [Cited in This Article: ] |
| 62. | Farias LPG, Strabelli DG, Sawamura MVY. COVID-19 pneumonia and the reversed halo sign. J Bras Pneumol. 2020;46:e20200131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 63. | Maturu VN, Agarwal R. Reversed halo sign: a systematic review. Respir Care. 2014;59:1440-1449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 64. | Aviram G, Bar-Shai A, Sosna J, Rogowski O, Rosen G, Weinstein I, Steinvil A, Zimmerman O. H1N1 influenza: initial chest radiographic findings in helping predict patient outcome. Radiology. 2010;255:252-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 65. | Zhou Z, Guo D, Li C, Fang Z, Chen L, Yang R, Li X, Zeng W. Coronavirus disease 2019: initial chest CT findings. Eur Radiol. 2020;30:4398-4406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 66. | Singh N, Singh S, Sharma BB, Singh V. Swine flu fibrosis: Regressive or progressive? Lung India. 2016;33:219-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 67. | Kohr JR, Bhargava P, Takasugi J, Goodman RB, Medverd JR. Imaging appearance of swine-origin influenza A (novel 2009 H1N1) pneumonia in an immunocompromised patient. Radiol Case Rep. 2010;5:361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 68. | Yuan Y, Tao XF, Shi YX, Liu SY, Chen JQ. Initial HRCT findings of novel influenza A (H1N1) infection. Influenza Other Respir Viruses. 2012;6:e114-e119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 69. | Choi MJ, Lee YS, Lee JY, Lee KS. Novel influenza A (H1N1) virus infection in children: chest radiographic and CT evaluation. Korean J Radiol. 2010;11:656-664. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 70. | Valette X, du Cheyron D, Goursaud S. Mediastinal lymphadenopathy in patients with severe COVID-19. Lancet Infect Dis. 2020;20:1230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 71. | Plesner LL, Dyrberg E, Hansen IV, Abild A, Andersen MB. [Diagnostic imaging findings in COVID-19]. Ugeskr Laeger. 2020;182. [PubMed] [Cited in This Article: ] |
| 72. | Elicker BM, Schwartz BS, Liu C, Chen EC, Miller SA, Chiu CY, Webb WR. Thoracic CT findings of novel influenza A (H1N1) infection in immunocompromised patients. Emerg Radiol. 2010;17:299-307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 73. | Dong D, Tang Z, Wang S, Hui H, Gong L, Lu Y, Xue Z, Liao H, Chen F, Yang F, Jin R, Wang K, Liu Z, Wei J, Mu W, Zhang H, Jiang J, Tian J, Li H. The role of imaging in the detection and management of COVID-19: a review. IEEE Rev Biomed Eng. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 150] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 74. | López Vega JM, Parra Gordo ML, Diez Tascón A, Ossaba Vélez S. Pneumomediastinum and spontaneous pneumothorax as an extrapulmonary complication of COVID-19 disease. Emerg Radiol. 2020;27:727-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 75. | Ucpinar BA, Sahin C, Yanc U. Spontaneous pneumothorax and subcutaneous emphysema in COVID-19 patient: Case report. J Infect Public Health. 2020;13:887-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 76. | Bor C, Demirağ K, Uyar M, Cankayalı I, Moral AR. Recurrent Spontaneous Pneumothorax during the Recovery Phase of ARDS Due to H1N1 Infection. Balkan Med J. 2013;30:123-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 77. | Chaturvedi A, Kumar A. Spontaneous Pneumothorax in H1N1 Infection. J Assoc Physicians India. 2017;65:97-98. [PubMed] [Cited in This Article: ] |