Hypercoagulable State Leading to Thrombotic Complications and Cerebral Artery Infarction in Patient with Severe Covid-19 Infection
Nujaimin Udin1, Abdul Karim Othman2,*, Nur Amirah Fazira Malzuki1, Siti Nurzulaikha Ab. Ghapar2, Nurul Nadzua Mohd Noor2
1Neurosurgical Unit, Department of Surgery, Hospital Sultanah Nur Zahirah, Ministry of Health, Malaysia
2Faculty of Medicine, University Sultan Zainal Abidin, Malaysia
Received Date: 06/10/2022; Published Date: 31/10/2022
*Corresponding author: Abdul Karim Othman, Faculty of Medicine, University Sultan Zainal Abidin, Malaysia
Abstract
We report a rare case of major deep vein thrombosis with Left Anterior Cerebral Artery (ACA) and Middle Cerebral Artery (MCA) infarction requiring emergency left decompressive craniectomy in a 40 year-old gentleman severe non-ICU COVID-19 infection with a no known risk factor for cerebrovascular disease or hypercoagulable state. The proposed mechanisms for hypercoagulable state among Covid-19 patients are through systemic inflammation and cytokine storm, postinfectious immune -mediated responses, and direct viral-induced endothelitis or endotheliopathy which potentially leading to angiopahic thrombosis. This complication is also associated with an increase rate of both arterial and venous thromboses in the pulmonary and systemic vasculature with the incidence rate of almost 2.8% to 3.8%. Therefore, we feel that it is crucial for all health personnel to have a high level of clinical suspicion and low threshold for diagnostic imaging for complications related to the hypercoagulable state among severe ICU and non-ICU COVID-19 patients.
Introduction
Covid-19 infection is a respiratory illness with a widespread systemic complication. Recent studies revealed a series of neurological manifestations are being recognized increasingly among patients with positive Covid-19 [1]. Among the neurological manifestations are encephalopathy, encephalitis, Gullain-Barre syndrome, and surprisingly acute cerebrovascular disease with the reporting incidence of 2-6% of patients hospitalised with Covid-19 [2]. These vascular complications are postulated to be associated with the pro-inflammatory hypercoagulable state with elevated C-reactive protein, D-dimer, and ferritin [3]. This complication is associated with an increase rate of both arterial and venous thromboses in the pulmonary and systemic vasculature with the incidence rate of almost 2.8% to 3.8%. The proposed mechanisms for hypercoagulable state among Covid-19 patients are through systemic inflammation and cytokine storm, postinfectious immune -mediated responses, and direct viral-induced endothelitis or endotheliopathy which potentially leading to angiopathic thrombosis [4,5].
Case Presentation
A 40-year-old healthy gentleman with no major risk factor of cerebrovascular disease such as hypertension, diabetes mellitus or smoking habit was immediately transferred to tertiary hospital for acute cerebral infarction from district hospital while being managed as category 4 Covid-19 infection. The patient has been admitted for 11 days in district hospital and throughout his admission in district hospital, there were no incidence of hypoxia and encephalopathy associated with hypoxia. This patient was staying in a Covid-19 infected area and he and his family was all positive for Covid-19 infection.
On day 11th of his admission in district hospital, he was found with sudden jerky movement over the left side of the body. Physical examination revealed a Glasgow Coma Scale (GCS) of E4V1M3 with bilaterally reactive pupils. The patient was immediately intubated and transferred to tertiary hospital for immediate CT brain imaging and for further care and intervention. CT scan imaging revealed a Left anterior cerebral artery (ACA) and middle cerebral artery (MCA) infarction with midline shift and underwent an emergency left decompressive craniectomy. 24 hours after emergency left decompressive craniectomy, repeated CT brain imaging revealed significant improvement of the midline shift with no further territory of infarction observed. However, a long segment of deep vein thrombosis was noted over the right lower limb extending from the right common iliac femoral vein to the popliteal vein. Upon completion of 48 hours of cerebral resuscitation, the patient was able to open his eyes, however the patient was not obeying command, withdrawal to pain and right hemiplegia with the motor power of 0/5.
Patient underwent physical rehabilitation with continuation treatment for deep vein thrombosis with synthetic anticoagulant; fondaparinux for 20 days and was later discharged with anticoagulant medication; rivaroxaban on day 24 after emergency decompressive craniectomy. One month after discharged from neurosurgical ward, the patient was seen again at neurosurgery clinic with a good GCS scoring, fully alert, able to follow command with right sided hemiplegia.
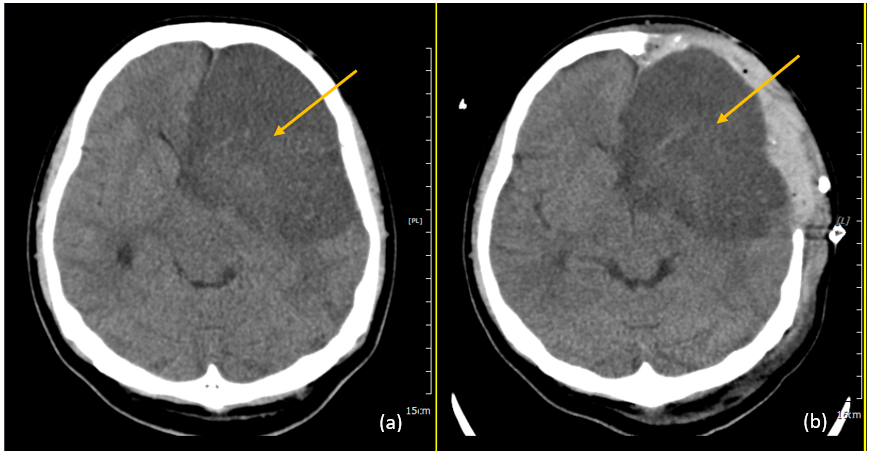
Figure 1: Arrow showing CT brain plain axial view (a)pre-operative imaging, (b)post-operative imaging.
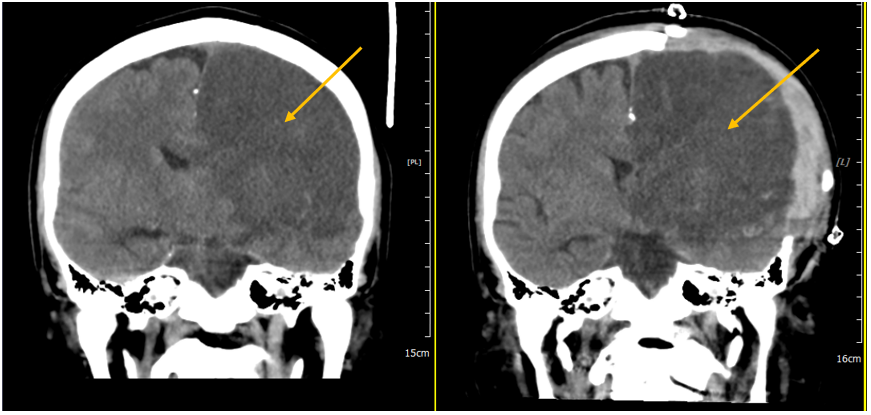
Figure 2: Arrow showing CT brain plain axial view (a)pre-operative imaging, (b)post-operative imaging.
Discussion
The presence of hypercoagulable state and evidence for the development of thrombotic complications in patient with COVID-19 is getting significant. Our case report illustrated a case of non-ICU critically ill COVID-19 patient presented with acute cerebral artery infarction associated with the findings of long segment deep vein thrombosis over the right lower limb extending from the right common femoral vein to the popliteal vein. Regardless of the potential pathogenesis of hypercoagulable state, the combination of critically ill COVID-19 infection with hypercoagulable state are the concerning aspect of the disease because of its high mortality and poor outcomes. Therefore, in managing our case, we feel that it is very crucial for all health personnel to have a high level of clinical suspicion and low threshold for diagnostic imaging for complications related to the hypercoagulable state of the patients.
Our research concerning to our case revealed an emerging discovery about COVID-19 with the mounting evidence linking the COVID-19 infection with acute ischemic stroke [6]. A retrospective study of 214 patients with COVID-19 infection from Wuhan, China, showed that 5.7% of the patients with severe infection suffered an acute cerebrovascular event [7]. In fact, there was a 7.5-fold increase in the odds of stroke with COVID-19 compared to patients with influenza6. Even more worrisome are the increasing number of reports of acute ischemic stroke in patients with COVID-19 infection who were younger than 50 years old [8,9]. COVID-19 associated neurologic symptom pathogenesis has been intensively studied worldwide and thromboembolic events are common in COVID-19 infected patients, particularly large vessel occlusion strokes [10] as occurred in our patient. Interestingly, as with our patient, Kihira et al [11] reported COVID-19 patients were 2.4 times more risk of large vessel strokes compares with patients without COVID-19 infection. Surprisingly, this association was not reported for small vessel strokes. They also reported that almost 62% of the strokes involving M1-M2. This represents a risk factor to developing malignant cerebral oedema.
Our case demonstrated a rare neurological complication related to COVID-19 infection because of his young age with no comorbidity related to the risk of hypercoagulable state or cerebrovascular event. Li et al [12] in a single-centre study reported that 5% of COVID-19 hospitalized patients suffered an acute ischemic stroke and that a higher incidence was seen in older patients with stroke risk factors. There is a strong association between stroke and major risk factors in COVID-19 patients, mainly age. Rothstein et al [13] reviewed a large series of patients with COVID-19 and acute cerebrovascular events, reporting that 95% of patients had a previous history of hypertension, 60% had a history of diabetes mellitus, and newly positive antiphospholipid antibodies were found in 75% of patients.
The mean age of patients with malignant middle cerebral artery stroke ranges from 43.5 to 63.5 years [14]. The mortality rate among the general population who underwent decompressive craniectomy for malignant middle cerebral artery stroke, despite receiving the best treatment, ranges from 20 to 55% in recent series [15]. The benefit of decompressive craniectomy after malignant MCA infarction in reducing the outcome of death, without increasing the risk if severe disability, and while also increasing independence, has been demonstrated in patients under 60 years of age [13]. With the immediate decompressive craniectomy done on his Left anterior cerebral artery (ACA) and middle cerebral artery (MCA) infarction, the patient was seen again at neurosurgery clinic with a good GCS scoring, fully alert, able to follow command with right sided hemiplegia.
Conclusion
COVID-19 patients have been shown to suffer a hypercoagulable state, increasing the risk of acute ischemic strokes, probably because of some procoagulant and inflammatory pathways that being activated. Therefore, we feel that it is very crucial for all health personnel to have a high level of clinical suspicion and low threshold for diagnostic imaging for complications related to the hypercoagulable state of the patients. The role of early screening for hypercoagulable state and immediate prophylactic anticoagulant may probably have the ability to reduce the risk of those events.
Acknowledgements
The authors would also like to acknowledge all the multidisciplinary members of neurosurgery, anaesthesia and clinicians in district hospital for their dedications and support in managing this case.
Compliance with Ethics Guidelines
Nujaimin Udin, Abdul Karim Othman, Nur Amirah Fazira Malzuki, Siti Nurzulaikha Ab. Ghapar and Nurul Nadzua Mohd Noor, declare that they have no conflict of interest. Patient anonymity was preserved, and this article does not contain any studies with animal subjects performed by any of the authors.
Funding: No funding sources.
Ethical approval: Not required.
References
- Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol,2020; 77:1366–1372.
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al.Neurologic Manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China.JAMA Neurol, 2020; 77: 683–690. doi: 10.1001/jamaneurol.2020.1127.
- Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol,2020; 19: 767-783.
- Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet,2020; 395: 1417-1418.
- Paniz-Mondolfi A, Bryce C, Grimes Z, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol,2020; 92: 699-702.
- Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E. Risk of Ischemic stroke in patients with Coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol, 2020; 77: 1-7.
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q. Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China. JAMA Neurol, 2020; 77: 683-690.
- Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med, 2020; 382: e60.
- Pisano TJ, Hakkinen I, Rybinnik I. Large vessel occlusion secondary to COVID-19 hypercoagulability in a young patient: A case report and literature review. J Stroke Cerebrovasc Dis, 2020; 29: 105307.
- Khan M, Ibrahim R, Siddiqi S, Kerolos Y, Al-Kaylani MM, AlRukn SA, et al. COVID-19 and acute ischemic stroke—a case series from Dubai, UAE. Int J Stroke, 2020; 15: 699–700. doi: 10.1177/17474930209 38285
- Kihira S, Schefflein J, Mahmoudi K, Rigney B, Delman NB, Mocco J, et al. Association of coronavirus disease (COVID-19) with large vessel occlusion strokes: a case-control study. AJR Am J Roentgenol, 2020; 29: 1– 6. doi: 10.2214/AJR.20.23847.
- Li Y, Li M, Wang M, Zhou Y, Chang J, Xian Y, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol, 2020; 5: 279–284. doi: 10.1136/svn-2020-000431.
- Rothstein A, Oldridge O, Schwennesen H, Do D, Cucchiara BL. Acute cerebrovascular events in hospitalized COVID-19 patients. Stroke, 2020; 51: e219–22. doi: 10.1161/STROKEAHA.120.030995.
- Wei H, Jia FM, Yin HX, Guo ZL. Decompressive hemicraniectomy versus medical treatment of malignant middle cerebral artery infarction: a systematic review and meta-analysis. Biosci Rep, 2020; 40: BSR20191448. doi: 10.1042/BSR20191448.
- Das S, Mitchell P, Ross N, Whitfield PC. Decompressive hemicraniectomy in the treatment of malignant middle cerebral artery infarction: a meta- analysis. World Neurosurg, 2019; 123: 8–16. doi: 10.1016/j.wneu.2018. 11.176.

