Abstract
COVID-19 pandemic is affecting millions of people all across the globe. Along with other clinical features, anosmia and dysgeusia are important symptoms being seen. This study evaluates the prevalence of olfactory and gustatory dysfunction in patients with SARS CoV-2 infection in a tertiary care centre and the severity and duration of altered taste and smell sensation in COVID positive patients. A total number of 167 patients that had tested positive for COVID 19 KLES Dr. Prabhakar Kore hospital in the study period of 3 months were assessed for presence and severity of olfactory and gustatory sensations. The prevalence of alteration of sense in COVID 19 patients in our tertiary care centre was found to be 62.87% and alteration of taste was 58.68%. This study shows that smell and taste loss has a high prevalence in patients of COVID 19 and health care workers should keep high degree of suspicion for COVID 19 when patients present with these symptoms. The early identification may help to reduce the risk of spread.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID 19) is an ongoing viral pandemic that emerged from East Asia and quickly spread to the rest of the world. The most prevalent symptoms seen were of fever (98%), cough (76%), dyspnea (55%), and myalgia or fatigue (44%) [1]. Anosmia and dysgeusia were the unusual and only presentation in some cases.
Apart from degenerative diseases, the most common etiologies of olfaction loss are postviral upper respiratory infection (URI) (18–45% of the clinical population), nasal/sinus disease (7–56%), head trauma (8–20%), exposure to toxins/drugs (2–6%), and congenital anosmia (0–4%) [2].
Hypothesis could be that the alterations in smell are due to damage caused by the virus to the olfactory pathways. The reduction in the neuronal lifespan in the olfactory epithelium is most likely to be the consequence of a decrease in the support caused by the loss of mitral cells and the absence of dendrites of the surviving mitral and tufted cells from the glomerular layer. Accordingly, the virus may carry out its damage at the level of the olfactory bulb rather than the epithelium [3].
Zinc deficiency is well known to cause anosmia and taste dysfunction. Carbonic anhydrase (CA VI) is present in saliva and nasal mucus. Serum zinc is a key cofactor in all CA activity. Thus, treating these sensory deficient patients with exogenous zinc increases CA synthesis and restores taste and smell function [4].
Angiotensin-converting enzyme 2 (ACE2) has been identified as the cellular receptor for SARS-CoV-2. Presumably, these drugs inactivate the G protein-coupled proteins and sodium-ion channels present in the taste receptors. Another possibility is that the ability to perceive flavours in these patients is adversely affected by the concomitant presence of olfactory disturbances due to the intimate functional correlation between these 2 chemosensory systems [5].
A majority of patients who test positive for COVID 19 are having a distorted smell sensation upto 6 months post recovery from the illness. This alteration in perception of the correct smell sensation is described as parosmia. Parosmia is typically associated with reduced olfactory sensitivity. It can occur after viral infections of the upper respiratory tract or after skull-brain traumas.
Treatment strategies for Olfactory dysfunction secondary to sinonasal diseases aim to resolve the underlying conditions. Various medications and supplementation have been given for treatment of smell disorders like vitamin B12 supplementation, zinc supplementation etc. however their exact role has not yet been established. Olfactory training (OT) aims to enhance olfactory recovery based on the neuronal plasticity of the olfactory system [6]. OT is recommended as conscious sniffing of at least four different odors at least twice daily for several months and has emerged as a simple and side‐effect free treatment option for various causes of smell loss [7].
In July 2020 the 1st Indian study was published which concluded that prevalence of new onset anosmia in Indian population with COVID-19 is 14.8% [8]. The prevalence of anosmia in Indian/Asian population is much lesser than that reported in European population. The aim of our study is to investigate and characterize the occurrence of olfactory and gustatory disorders in patients with laboratory-confirmed COVID-19 infection using a large sample size and assessment of time period required for recovery of these symptoms.
In times of the corona virus disease 2019 (COVID-19) pandemic, the low prevalence of sensorineural viral anosmia in society as a whole has made clinical research challenging.
Methodology
A cross sectional study among all Covid positive patients admitted in our tertiary care hospital was done for a study period of 3 months from July 2020 to September 2020. A total of 167 patients were included. All patients more than 18 years of age who tested positive for SARS-CoV-2-RNA by polymerase chain reaction by nasopharyngeal and throat swabs/ patients with CORAD scoring more than equal to 4 were included in the study. Patients with olfactory or gustatory dysfunctions before the epidemic, history of allergic rhinitis or chronic rhinosinusitis, any obstructive nasal pathology or any nasal surgeries were excluded.
Procedure
All selected patients were given the treatment for covid 19 as per the guidelines. Informed written consent was obtained from each patient. Each patient was given a standardised questionnaire [9] of 22 questions regarding olfactory and gustatory dysfunction faced by them. The questionnaire was carried out by telephonic assessment using google forms. The progress of symptoms and resolution was noted upto 3 months.
The categorical data was expressed in terms of rates, ratios and percentages. The association between the outcome, clinical and demographic characteristics was tested using Chi-square test and Fisher’s exact test. For all the tests the value of p less than 5% (0.05) was considered significant.
Result
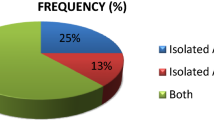
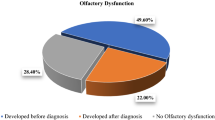
Out of 167 patients in our study [10], 105 patients had altered sense of smell (62.87%) and 98 had altered sense of taste (58.68%) after diagnosis of the disease as shown in Fig. 1. The majority of patients in our study were less than 29 years of age (61/167) attributing to 36.53%. This was followed by age group of 30–49 years (34.73%), then 50–60 years (24.55%) and only 4.19% patients were above the age of 60 years. The mean age of patients was 39 years. Our analysis shows a male preponderance in patients with COVID 19 with male to female ratio as 1.2:1. As seen in Fig. 2 only 44/167 i.e. 26.7% patients had smell and taste alteration as the first symptom. Table 1 shows us that there was a 50% decrease in the sense of smell during the disease among all the patients when compared before the disease. After 14 days there was a 74% improvement in the sense of smell when compared to smell during the disease period. There was a 45.26% decrease in the sense of taste during the disease among all the patients when compared before the disease as seen in Table 2. After 14 days there was a 63.21% improvement in the sense of taste when compared to taste during the disease period.
Majority of patients recovered their sense of smell and taste within 14 days post diagnosis. 39.64% completely recovered by 14 days, 36.94% recovered within 30 days and only 23.42% had persistent symptoms after 30 days of diagnosis. Around 21.3% patients had a distorted smell sensation even upto 3 months post recovery.
Discussion
Up until COVID 19, patients with sensorineural viral anosmia and dysgeusia were seldom seen in general otolaryngology practice with approximately one to two new-onset patients each year. Zou and colleagues found that the virus binds to ACE receptors in nasal epithelium and causes degeneration of the nasal mucosa and subsequent inflammation and damage to the neural receptors responsible for olfaction. Another hypothesis, currently the most widely accepted, suggests the direct changes to the central nervous system by the virus [9]. Therefore The American Academy of Otolaryngology—Head and Neck Surgery and the British Association of Otorhinolaryngology are now recommending these symptoms be added to the list of primary screening symptoms for COVID-19 [1].
Our study was conducted in a tertiary care centre among all covid positive patients including health care workers. We evaluated the sense of smell and taste before, during and 14 days after the diagnosis and noted a high prevalence of loss of sense and taste among COVID 19 patients as 62.87% and 58.68% respectively. Also there was a significant reduction in smell (50.76%) and taste (45.26%) perception during the disease which improved significantly for majority of patients (39.64%). We observed that with increasing age the incidence of these symptoms reduced and the mean age seen was of 39 years. Along with smell and taste we also evaluated other symptoms of fever, malaise, headache, sore throat and difficulty in breathing and a significant number of patients had smell and taste alteration as the 1st symptom (26.35%). The previously done studies in India have evaluated the prevalence of olfactory and taste dysfunction in a very small group of patients and have not followed up the patients for recovery of their taste and smell dysfunction. In our study we followed up the patients for a period of 3 months post infection to evaluate the recovery and improvement in symptoms.
In a retrospective study conducted by Lv et al. (Wuhan, China) in September 2020, out of 196 patients 8.2% and 4.6% of patients reported olfactory and taste disorders, respectively [11]. In a systematic review and meta-analysis of Smell and Taste Dysfunction in Patients With COVID-19 Akosua Adom Agyeman et al. found that about 41% and 38% of diagnostic-confirmed patients with COVID- 19 infection presented with olfactory or gustatory dysfunctions respectively. The studies involved a total of 8438 patients. In a study by Prasun et al. in India the prevalence of new onset anosmia in Indian population with COVID-19 was seen 14.8% [8]. These results indicate that the prevalence and prognosis of olfactory or gustatory impairment in COVID-19 patients vary globally, reflecting the complexity of this disease.
In India very few studies have given the prevalence of anosmia and dysgeusia among patients. Understanding the prevalence of these symptoms in our country can alert the otolaryngologists and help in early detection and management of covid 19.
Conclusion
Our current study strongly confirms the high prevalence of olfactory and gustatory disorders in COVID-19 infection. Smell and taste loss should be used as indicators of potential contagion and otolaryngologists should keep high degree of suspicion for COVID 19 when patients present with these symptoms. The early identification may help to reduce the risk of spread especially by pauci symptomatic cases [9].
Data Availability
Data transparency.
References
Machado C, Gutierrez J (2020) Anosmia and ageusia as initial or unique symptoms after SARS-COV-2 virus infection. Preprints 20(20)
Dai Q, Pang Z, Yu H et al (2016) Recovery of olfactory function in postviral olfactory dysfunction patients after acupuncture treatment. Evid-Based Complement Altern Med:1–6
Vaira LA, Italy Alessandro Giuseppe Fois et al (2020) Potential pathogenesis of ageusia and anosmia in COVID‐19 patients. Int Forum Allergy Rhinol
Komai M, Goto T, Suzuki H et al (2000) Zinc deficiency and taste dysfunction, contribution of carbonic anhydrase, a zinc-metalloenzyme, to normal taste sensation. BioFactors 12(1–4):65–70
Gheblawi M, Wang K, Viveiros A et al (2020) Angiotensin converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system. Circ Res 126(10):1456–1474
Liu DT, Sabha M, Damm M, Philpott C et al (2021) Parosmia is associated with relevant olfactory recovery after olfactory training. Laryngoscope 131(3):618–623
Hummel T, Rissom K, Reden J et al (2009) Effects of olfactory training in patients with olfactory loss. Laryngoscope 119(3):496–499
Mishra P, Gowda V, Dixit S (2020) Prevalence of new onset anosmia in COVID-19 patients: is the trend different between European and Indian population? Indian J Otolaryngol Head Neck Surg 72(4):484–487
Butowt R, von Bartheld CS et al (2020) Anosmia in COVID-19: underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist. https://doi.org/10.1177/1073858420956905
Dell’Era V, Farri F, Garzaro G et al (2020) Smell and taste disorders during COVID‐19 outbreak: a cross‐sectional study on 355 patients. Head Neck:1–6
Lv H, Zhang W, Zhu Z et al (2020) Prevalence and recovery time of olfactory and gustatory dysfunctions of hospitalized patients with COVID-19 in Wuhan, China. Int J Infect Dis 100:507–512
Acknowledgements
I would like to thank my teachers and post graduate colleagues and clerical staff from the department of otorhinolaryngology and Head and Neck Surgery for their invaluable help and time.
Funding
None.
Author information
Authors and Affiliations
Contributions
Present.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical Approval
Obtained institutional ethical clearance.
Consent to Participate
Obtained.
Consent for Publication
Obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hajare, P.S., Harugop, A.S., Goswami, L. et al. Prevalence of Olfactory and Gustatory Dysfunction in Coronavirus Disease (COVID-19): A Cross Sectional Study in Our Tertiary Care Hospital. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 3012–3015 (2022). https://doi.org/10.1007/s12070-021-02702-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02702-w