Abstract
The tests currently used for the identification of SARS-CoV-2 include specimens taken from the upper and lower respiratory tract. Although recommendations from the World Health Organization prioritise the usage of a nasopharyngeal swab (NS), nasopharyngeal aspirates (NPA) are thought to be superior in identifying SARS-CoV-2 in children. To our knowledge, however, no paediatric study has been published on the subject. The aim of this study is to evaluate the diagnostic performances of NS referred to NPA for SARS-CoV-2 in children. We calculated the sensitivity and specificity of the NS referred to the NPA of the whole sample and considered both age and collection period as covariates in different analyses. We collected 300 paired samples. The NS had a specificity of 97.7% and a sensitivity of 58.1%. We found similar results for the group of subjects ≥ 6 years old, while for subjects < 6 years old, the sensitivity was 66.7% and the specificity 97.8%. Considering period as a covariate, the sensitivity and specificity for patients hospitalised in March (31 patients, 52 records) were 70.0% and 97.6%, while for patients involved in the follow-up (16 patients, 57 records), they were 57.2% and 89.7%. The NS has a low sensitivity in detecting SARS-CoV-2 in children when referred to the NPA, whereas its specificity is high. Our results suggest that in children under 6 years of age, NSs should be preferred whenever possible. Though statistically not significant, the sensitivity of the NS rises when performed before the NPA.
Similar content being viewed by others
Introduction
In December 2019, the world witnessed the emergence of a novel coronavirus in Wuhan, China. Later named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the new coronavirus is responsible for a respiratory disease now known as the coronavirus disease (COVID-19). After spreading across the globe, the World Health Organization (WHO) declared COVID-19 an international health emergency [1]. In February 2020, the outbreak also involved Italy, which became one of the worst affected countries [2].
Cases reported in literature mainly concern adults and the mortality rate is higher in the elderly and in subjects with chronic underlying diseases [3].
Data regarding infected children are so far limited. In a study reviewing 44,672 laboratory-confirmed cases of COVID-19, Wu et al. reported that 1% of cases occurred in children from 10 to 19 years of age and another 1% in children of 9 years of age or younger, with no deaths reported in the latter group [4]. Overall, children younger than 18 years of age appear to be less vulnerable to the infection, to have milder symptoms, and a less severe disease course compared to adults [4,5,6,7]. A Chinese observational study reported that, of the 1391 children younger than 16 years of age tested for SARS-CoV-2, only 171 (8.1%) resulted positive. Among them, 15.8% were asymptomatic while the rest showed only mild symptoms [8]. These observations are similar to what was reported in a recent seroprevalence study which analysed data generated from the first lockdown in Lombardy. More specifically, the study showed a linear increase in the log odds for IgG positivity with age, ranging from 9.1% in 5-year-old children to 12.5% in 20-year-old individuals and ending at around 40% for people over 80 [9].
The tests currently used for the direct identification of SARS-CoV-2 include specimens taken from the upper (nasopharyngeal/oropharyngeal swab and nasopharyngeal aspirate) and the lower respiratory tract (bronchoalveolar lavage, tracheal aspirate, sputum) [10,11,12].
Upper respiratory specimens are easily obtainable, require less invasive manoeuvres than lower respiratory specimens, and their collection exposes healthcare workers to a lower risk of infection. Asymptomatic children and patients with mild symptoms are therefore usually tested with this type of sampling. The collection of lower respiratory specimens is instead reserved for symptomatic or severe cases due to the high discomfort caused, the special devices, and skilled operators required to obtain them [10].
Yang et al. demonstrated that SARS-CoV-2 isolation from the bronchoalveolar lavage fluid (BALF) had a 100% positive rate when collected from severe cases, while isolation from sputum resulted in the highest positive rate when collected from both severe and mild cases, followed by nasal swab [13, 14]. Regarding samples collected from the upper airways, higher viral loads were detected in the nose than in the throat; indeed, recommendations from WHO prioritise nasopharyngeal swab over oropharyngeal swab [10, 15].
Zou et al. demonstrated that the viral load in symptomatic children is similar to that of asymptomatic patients, which suggests a potential contagiousness of the latter [15]. Furthermore, they detected higher viral loads in specimens collected soon after the symptom’s onset which may indicate a higher risk of transmission in the early stages of infection [10, 15].
Although a positive test is highly indicative of infection, a negative test does not rule it out [16]. Several factors may contribute to false-negative results including the sampling technique, the transportation process, the potentially limited RNA found in the samples, and the molecular structure making up the coronavirus (e.g. genetic mutations such as D614G acquired by SARS-CoV-2 that naturally selected dominant lineages helping the virus to spread faster and acquire higher levels of virulence) [17, 18]. Testing of specimens from multiple sites may help reduce false-negative results [13].
To date, there are no paediatric studies on the identification of SARS-CoV-2 through nasopharyngeal aspirate (NPA). Various studies on major respiratory viruses have shown that in the paediatric population the sensitivity of nasal swabs (NS) is comparable to that of NPAs. There have been some reports, however, that highlight a lower sensitivity of the former compared to the latter for the detection of common viruses such as the Respiratory Syncytial Virus and the Rhinovirus [19,20,21]. It is generally agreed that the NS is recommended in outpatient settings because of its rapid and less traumatic collection and because it usually does not require any training and additional devices. On the other hand, for hospitalised patients, who could receive unnecessary antibiotic therapy or be subject to additional diagnostic procedures, the NPA is the test of choice due to its higher sensitivity [22, 23]. For this reason, we considered the NPA as our reference test.
Our study was aimed at evaluating if the NS could be used instead of the NPA in children. To do this, we calculated the concordance and the diagnostic performance of the NS compared the NPA’s in accordance with age and order in which the tests were administered.
Methods
Patients and samples
From March 13th to May 22nd, all children who attended the emergency room and needed to be hospitalised and those who were transferred to our paediatric unit from other wards/hospitals underwent both NS and NPA, acquiring specimens from both nostrils. The tests were performed, sequentially, on admission and after 24 h by well-trained nurses or doctors. The nasopharyngeal swabs were collected following the procedure published in the New England Journal of Medicine [24], first from one nostril and then from the other, using the Copan-503CS01 nasopharyngeal flocked swab. The nasopharyngeal aspirates were collected from both nostrils using a standard protocol and the Medicoplast mucus extractor 440-ch08. In the laboratory, two assays were performed for the detection of SARS-CoV-2. The AllplexTM 2019-nCoV Assay was used with the Seegene NIMBUS & STARlet instrument, an in vitro diagnostic medical device designed for the qualitative detection of the novel Coronavirus (2019-nCoV) by real-time reverse transcription-polymerase chain reaction (RT-PCR). Starting from 300 μl of both NS and NPA samples, nucleic acid extraction was performed using the STARMag 96 X 4 Universal Cartridge kit and 10 μl of RP-V Internal Control (IC) which was added to each specimen before RNA extraction. The second assay, GeneFinder COVID-19 Plus RealAmp Kit adapted to the ELITe InGenius®(ELITechGroup) instrument, is a qualitative one-step RT-PCR that used 200 μl of both samples for automatic and integrated extraction. In this case, the IC was endogenous (RNase p).
For samples analysed with the GeneFinder COVID-19 Plus RealAmp Kit, we considered positive Ct values ≤ 45 and negative Ct > 45, while for the Allplex™ 2019-nCoV Assay, positive findings were considered when Ct values were ≤ 40 and negative when Ct values were > 40. A weak positivity was defined for Ct values of 40–45 or 37–40, depending on the method.
There was not a defined order for obtaining the specimens. More specifically, we performed first the NS and then the NPA in March 2020, whereas we collected first the NPA and then the NS during the follow-up. A total of 134 patients were included in the study. Thirteen among the latter and two outpatient children were followed by collecting paired specimens until both came out negative 24 h apart. Thus, 300 paired specimens (NS/NPA) were collected from 136 patients (134 hospitalised and 2 outpatients) and were tested for SARS-CoV-2.
Statistical analyses
All the statistical analyses were performed with R (v. 3.6.2) [25]. In order to estimate the incidence of the positive cases on hospitalised patients, we calculated the proportion of the positive cases (patients who had a positive result of NS or a positive result of NPA) in hospitalised patients and its 95% confidence interval using the binomial distribution [26].
Analyses on diagnostic tests results (NS and NPA) concerned the concordance between the results of the two tests. Furthermore, we calculated the mismatch for positive and negative values and the sensitivity and specificity of NS (considering NPA as reference). In order to evaluate whether sensitivity, specificity, and mismatch of the NS were influenced by the patients’ age, we considered age as a covariate (coded as 0 from 0 to 5 years old and as 1 for more than 5 years old).
Since the order of collecting specimens was different between patients hospitalised in March, and patient of the follow-up, for the purpose of detecting any change in sensitivity, specificity, and mismatches according to the order of execution of the tests, we considered the period as covariate (codified as 0 for the March period and as 1 for the follow-up).
Concerning the performance of the NS (considering NPA as reference test), descriptive summary measures were also calculated: likelihood ratio positive (LR+) and negative (LR−). Likelihood ratios compare the probability that a patient with positive NPA at the date of the test has a particular NS test result as compared to someone with NPA negative. LR+ is the ratio between the probability of a true positive result on the probability of false positive result. LR− is the ratio between the probability of a false negative result on the probability of a true negative result [27].
Tests with very high LR+ and very low LR− have greater discriminating ability: in particular, tests with LRs > 10 or < 0.1 are very useful in establishing or excluding a diagnosis [28].
The analyses were performed by generalised estimating equation models (GEE) with family binomial to take account of the correlation among diagnostic tests on the same patients [29]. To estimate the percentage of concordance, the model response was coded as 1 if the results of the two diagnostic tests agreed and as 0 otherwise. To estimate the sensibility and the mismatch for positive values, only the records with a positive result of the NPA were used, while to estimate specificity and negative mismatch, only the records with a negative result of the NPA were used. In both cases, the model response was the result of the NS (coded as 0 if it was negative and as 1 if it was positive) [30].
The influence of age and test period was estimated using the Wald test on the respective model coefficients with a 5% significance level (two-tailed test).
Due to the absence of a reliable prevalence value for COVID-19 in children, we could not calculate the positive and negative predictive values (VPP, VPN).
Results
For this study’s purposes, we considered positive to SARS-CoV-2 every patient whose NPA or NS or NPA/NS resulted positive or weak positive.
Out of the 134 patients hospitalised, 18 children tested positive (prevalence 13.4%, 95% CI: 8.2–20.4%). Among the latter, 13 of them and 2 outpatient children were followed by collecting paired specimens until both resulted negative 24 h apart.
We collected 600 samples in total (equal to 300 paired): 43 positive NPA, 31 positive NS, 257 negative NPA, and 269 negative NS.
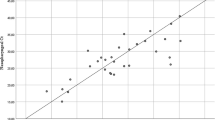
Of the 300 paired specimens evaluated: 276 were concordant; 24 were discordant, so the naïve concordance was 92.0% (95% CI: 88.3–94.6%).
The mismatch negative NS and positive NPA was greater than the mismatch positive NS and negative NPA (about 42% and about 2% respectively), see Table 1.
The NS’s specificity was greater than its sensitivity, suggesting the NS test was more suitable to rule-in positive NPA patients than in ruling-out negative NPA patients (sensitivity was about 58% and specificity was about 98%). The LR+ was 25.3 and LR− was 0.43, which means that a patient with a positive result from an NPA is 25.3 times more likely to have a positive result from an NS than someone with a negative result from an NPA and that a patient with a positive NPA is 0.43 times as likely to have a negative NS than someone with a negative NPA (or that a patient with a negative NPA is about 2 times more likely to have a negative NS than someone with a positive NPA). Considering the high value of the LR+ (greater than 10), the NS is expected to be useful in establishing the positivity of SARS-CoV-2; however, the NS is probably not very useful in excluding the infection, as shown by the higher than 0.1 LR-.
Considering age as a covariate, its effect on the above-mentioned measures was not statistically significant for all models at the 5% significance level. More specifically, considering the mismatch between positive NPAs and negative NSs, we obtained a Z value (Wald statistic) of 0.493 (p = 0.483), for the mismatch between negative NPAs and positive NSs, we obtained a Z value of 0.03 (p = 0.87) while considering sensitivity and specificity, we found Z values of 0.49 (p = 0.48) and 0.03 (p = 0.87), respectively.
Concerning sensitivity, specificity, LR+ (21.9), and LR− (0.46), results regarding subjects ≥ 6 years old were similar to those for “all records” (Table 1).
The mismatch between negative NSs and positive NPAs was smaller for subjects < 6 years old (about 33%) than for all subjects and subjects ≥ 6 years old, while the mismatch between positive NSs and negative NPAs was similar (about 2%) among the three groups (Table 1).
The specificity of the NS for this age group was greater than its sensitivity, suggesting the test was more suitable to detect positive NPA patients than negative NPA patients (the test had a sensitivity of about 67% and a specificity of about 98%). In addition, the sensitivity was greater than the sensitivity calculated for all subjects and for subjects ≥ 6 years old (Table 1). The LR+ was 30.3 and LR− was 0.34.
As described above, we considered patients hospitalised in March (31 patients and 52 records) and patients involved in follow-up (16 patients and 57 records).
Regarding hospitalised children in March, we retrieved 52 paired specimens: 10 positive NPAs, 8 positive NSs, 42 negative NPAs, 44 negative NSs. Of the 52 paired specimens evaluated, 48 were concordant and 4 were discordant; thus, the naïve concordance was 92.3% (95% CI: 81.7–97.0%). The results for these records showed that the smallest mismatch was between negative NSs and positive NPAs (30%). The mismatch between positive NSs and negative NPAs was similar to the previously presented results (about 2%). While we found a similar specificity to that of our other results, the sensitivity was higher (70%), see Table 1. The LR+ was 29.2 and the LR− was 0.31.
Concerning the follow-up samples, there were 57 paired specimens: 28 positive NPAs, 19 positive NSs, 29 negative NPAs, and 38 negative NSs. Of the 57 paired specimens evaluated, 42 were concordant and 15 were discordant; thus, the naïve concordance was 73.7% (95% CI: 61.8–82.9%). In this case, the mismatch between negative NSs and positive NPAs was similar to the analyses on all subjects and on subjects ≥ 6 years old (about 43%); the mismatch, however, between positive NSs and negative NPAs was greater than all previous results (about 10%). Here, the specificity was greater than the sensitivity (about 90% for the specificity and about 57% for the sensitivity), although the former was also the lowest among all previous analyses (Table 1). The LR+ was 5.6 and LR− was 0.48.
The impact of period on the above-mentioned measures was not statistically significant at a 5% significance level for all models. Especially for the mismatch between positive NPAs and negative NSs, we obtained a Z value (Wald statistic) of 0.520 (p = 0.471) and for the mismatch between negative NPAs and positive NSs, we had a Z value of 1.8 (p = 0.180). The Z values for sensitivity and specificity were respectively of 0.52 (p = 0.47) and 1.8 (p = 0.180).
Discussion
According to our results, the NS has a low sensitivity in the detection of SARS-CoV-2 in children. At the same time, the NS has both a high specificity and a high LR+, which means that a positive NS has a good reliability in detecting who has a positive NPA.
Despite the influence of age and collection period resulted not statistically significant, the difference between the results of the two age groups and of the two collection periods could suggest a potential impact of the two factors, which should be evaluated in larger case series.
Regarding the order with which the tests were obtained, the sensitivity and specificity in hospitalised children in March were higher than those of follow-up patients. This may imply that executing an NS before an NPA may result in a greater probability of identifying SARS-CoV-2. This may be explained by the fact that the NPA, through the thin catheter of the mucus extractor, is able to collect a larger amount of secretions from the lower parts of the upper respiratory tract and number of deeper cells compared to the NS [31, 32], which may lead to reduced or inadequate samples to identify the virus when the NS is used after the NPA. Our results were not statistically significant probably due to the small and non-uniform sample examined, so further studies, involving a larger sample, are necessary to strengthen this evidence.
Concerning age, the sensitivity of the NS was highest in the group of children younger than 6 years. This means that a negative NS has a good reliability in detecting the patient who has a negative NPA. Moreover, patients younger than 6 years have the highest LR+, while the specificity is similar to that found in the other analysed groups. The NS, therefore, is suitable to identify children younger than 6 years with a positive NPA. According to these results, performing NSs in this age group is better for identifying a SARS-CoV-2 infection. Although our results point towards a better identification of the SARS-CoV-2 infection using the NS in children under 6 years, in our experience, [21, 32], performing an NPA in young children is simpler than performing an NS: the aspiration of mucus from the nasopharynx using the small catheter resulted less unpleasant compared to brushing against the nasopharyngeal wall using the NS. At the same time, the NPA requires a catheter, an aspiration trap, a vacuum source, and specialised training, which are only available in a hospital setting. On the other hand, for the NS, no additional training or devices are needed.
Our study has some limitations. Firstly, the different order with which the specimens were obtained, which implies that the data are not uniform. Secondly, the small sample. Another limitation is the lack of data regarding signs and symptoms of patients who underwent NPA and NS and the resulting inability to describe a correlation between the isolation of SARS-CoV-2 and clinical features. Finally, to our knowledge, an analysis on the relationship between the viral load and the infectivity has not yet been reported. It has been, however, demonstrated that the identification of the virus on a specimen does not necessarily correlate with infectivity and there are indeed multiple reports which attest a prolonged viral shedding after symptoms resolution in COVID-19 [33]. In our department, among children whose tests were positive, three continued to be positive to either NS or NPA or both for the following 9 weeks. These findings are in line with several other studies that demonstrated the prolonged viral shedding of children [34, 35].
Conclusions
The NS has a low sensitivity in detecting SARS-CoV-2 in children when referred to NPA, both in the overall analysis and in that according to age. Its specificity on the other hand is high. This means that a positive NS can be reliable, but that a negative NS cannot rule out the presence of SARS-CoV-2 since the proportion of false negatives is substantial.
Though statistically not significant, we found that when the NS is performed before the NPA, its sensitivity rises, which may be due to the fact that NSs performed before NPAs are richer in secretion, cells, and therefore viruses.
Although statistical significance was not reached, our results suggest that the use of the NS for the detection of SARS-CoV-2 should be preferred whenever possible in children younger than 6 years, thanks to its high LR+.
As far as we know, this is the first study dealing with diagnostic performance of NS referred to NPA for detecting SARS-CoV-2 in children. Further analyses are mandatory to transfer these findings to our clinical practice.
Data availability
All data were collected in a computerised database, and all biological samples were anonymised before their inclusion in the collection.
References
World Health Organization. Coronavirus disease 2019 (COVID-19). Situation Report 51. Published March 11, 2020. Accessed July 27, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
Epicentro. Istituto Superiore della sanità. Dati della Sorveglianza integrata COVID-19 in Italia. Published February 27, 2020. Accessed July 27, 2020. https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard
Wang L, Wang Y, Ye D, Liu Q (2020) Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int J Antimicrob Agents 55:105948
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323:1239–1242
Ludvigsson JF (2020) Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr 109:1088–1095
Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S (2020) Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med 382:1370–1371
Brodin P (2020) Why is COVID-19 so mild in children? Acta Paediatr 109:1082–1083
Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, Zhang W, Wang Y, Bao S, Li Y, Wu C, Liu H, Liu D, Shao J, Peng X, Yang Y, Liu Z, Xiang Y, Zhang F, Silva RM, Pinkerton KE, Shen K, Xiao H, Xu S, Wong GWK, Chinese Pediatric Novel Coronavirus Study Team (2020) SARS-CoV-2 infection in children. N Engl J Med 382:1663–1665
Pagani G, Conti F, Giacomelli A, Bernacchia D, Rondanin R, Prina A, Scolari V, Gandolfi CE, Castaldi S, Marano G, Ottomano C, Boracchi P, Biganzoli EM, Galli M (2020) Seroprevalence of SARS-CoV-2 IgG significantly varies with age: results from a mass population screening (SARS-2-SCREEN-CdA). MedRxiv. https://doi.org/10.1101/2020.06.24.20138875
Mawaddah A, Gendeh HS, Lum SG, Marina MB (2020) Upper respiratory tract sampling in COVID-19. Malays J Pathol 42:23–35
Loeffelholz MJ, Tang YW (2020) Laboratory diagnosis of emerging human coronavirus infections - the state of the art. Emerg Microbes Infect 9:747–756
Hanson KE, Caliendo AM, Arias CA, Englund JA, Lee MJ, Loeb M, Patel R, El Alayli A, Kalot MA, Falck-Ytter Y, Lavergne V, Morgan RL, Murad MH, Sultan S, Bhimraj A, Mustafa RA (2020) Infectious Diseases Society of America Guidelines on the diagnosis of COVID-19. Clin Infect Dis ciaa760
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W (2020) Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 323:1843–1844
Yang Y, Yang M, Shen C (2020) Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. MedRxiv. https://doi.org/10.1101/2020.02.11.20021493
Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J (2020) SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 382:1177–1179
Zitek T (2020) The appropriate use of testing for COVID-19. West J Emerg Med 21:470–472
Winichakoon P, Chaiwarith R, Liwsrisakun C, Salee P, Goonna A, Limsukon A, Kaewpoowat Q (2020) Negative nasopharyngeal and oropharyngeal swabs do not rule out COVID-19. J Clin Microbiol 58:e00297–e00220
Callaway E (2020) The coronavirus is mutating - does it matter? Nature 585(7824):174–177
Sung RY, Chan PK, Choi KC, Yeung AC, Li AM, Tang JW, Ip M, Tsen T, Nelson EA (2008) Comparative study of nasopharyngeal aspirate and nasal swab specimens for diagnosis of acute viral respiratory infection. J Clin Microbiol 46(9):3073–3076
Meerhoff TJ, Houben ML, Coenjaerts FE, Kimpen JL, Hofland RW, Schellevis F, Bont LJ (2010) Detection of multiple respiratory pathogens during primary respiratory infection: nasal swab versus nasopharyngeal aspirate using real-time polymerase chain reaction. Eur J Clin Microbiol Infect Dis 29:365–371
Faden H (2010) Comparison of midturbinate flocked-swab specimens with nasopharyngeal aspirates for detection of respiratory viruses in children by the direct fluorescent antibody technique. J Clin Microbiol 48:3742–3743
Macfarlane P, Denham J, Assous J, Hughes C (2005) RSV testing in bronchiolitis: which nasal sampling method is best? Arch Dis Child 90:634–635
Lambert SB, Whiley DM, O’Neill NT, Andrews EC, Canavan FM, Bletchly C, Siebert DJ, Sloots TP, Nissen MD (2008) Comparing nose-throat swabs and nasopharyngeal aspirates collected from children with symptoms for respiratory virus identification using real-time polymerase chain reaction. Pediatrics 122:e615–e620
Marty FM, Chen K, Verrill KA (2020) How to obtain a nasopharyngeal swab specimen. N Engl J Med 382:e76
R Development Core Team, R (2011) R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. https://www.r-project.org/
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26:404–413
Ranganathan P, Aggarwal R (2018) Understanding the properties of diagnositc tests-part 2: likelihood ratios. Perspect Clin Res 9:99–102
Deeks JJ, Altman DG (2004) Diagnostic tests 4: likelihood ratios. BMJ 329:168–169
Liang KY, Zeger SL (1984) Longitudinal data analysis using generalized linear models. Biometrika 73:13–22
Leisenring W, Sullivan Pepe M, Longton G (1997) A marginal regression modelling framework for evaluating medical diagnostic tests. Stat Med:1263–1281
Chan KH, Peiris JSM, Lim W, Nicholls JM, Chiu SS (2008) Comparison of nasopharyngeal flocked swabs and aspirates for rapid diagnosis of respiratory viruses in children. J Clin Virol 42:65–69
Abu-Diab A, Azzeh M, Ghneim R, Ghneim R, Zoughbi M, Turkuman S, Rishmawi N, Issa AE, Siriani I, Dauodi R, Kattan R, Hindiyeh M (2008) Comparison between pernasal flocked swabs and nasopharyngeal aspirates for detection of common respiratory viruses in samples from children. J Clin Microbiol 46:2414–2417
Widders A, Broom A, Broom J (2020) SARS-CoV-2: the viral shedding vs infectivity dilemma. Infect Dis Health S2468-0451(20):30028–30026
Liu P, Cai J, Jia R, Xia S, Wang X, Cao L, Zeng M, Xu J (2020) Dynamic surveillance of SARS-CoV-2 shedding and neutralizing antibody in children with COVID-19. Emerg Microbes Infect 9:1254–1258
Lu Y, Li Y, Deng W, Liu M, He Y, Huang L, Lv M, Li J, Du H (2020) Symptomatic infection is associated with prolonged duration of viral shedding in mild coronavirus disease 2019: a retrospective study of 110 children in Wuhan. Pediatr Infect Dis J 39:e95–e99
Acknowledgements
On behalf of Testing Pediatric Covid-19 (TPC-19):
Andrea Gori, MD1,2, Carlo Agostoni, MD1,2, Raffaella Pinzani, MD2, Ferruccio Ceriotti, MD2.
1University of Milan, Milan, Italy
2Foundation IRCCS Ca′ Granda, Ospedale Maggiore Policlinico, Milan, Italy
Author information
Authors and Affiliations
Consortia
Contributions
Prof Marchisio, Castaldi, and Biganzoli conceptualised and designed the study, reviewed, and revised the manuscript. Drs Di Pietro and Capecchi collected data, wrote, and reviewed the manuscript. Drs Biganzoli, Luconi, Marano, and Boracchi analysed the statistical data.
Drs Lunghi and Ceriotti analysed the specimens. Prof Gori and Agostoni, Drs Bertolozzi, Bosis, Pinzani, and Cantoni reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
No informed consent was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Pietro, G.M., Capecchi, E., Luconi, E. et al. Diagnosis of SARS-CoV-2 in children: accuracy of nasopharyngeal swab compared to nasopharyngeal aspirate. Eur J Clin Microbiol Infect Dis 40, 1155–1160 (2021). https://doi.org/10.1007/s10096-020-04131-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-04131-z