Abstract
Aim
This study aims to examine the effect of COVID-19 on the anxiety levels of healthcare employees.
Methods
This descriptive study used the snowball sampling method to recruit participants. The study was conducted between 18 and 25 April 2020 with a total of 710 participants. The data were collected using a sociodemographic questionnaire and the State-Trait Anxiety Inventory. Ethics committee approval was obtained to conduct the study, and the data were analyzed using the SPSS 24.0 statistical package program using descriptive statistics, t tests and ANOVA.
Results
In the study, 46.8% of the participants were in the 26–35 age group, 60.7% were female, 19.9% worked at clinics with COVID-19 patients (service, intensive care and emergency clinics), and 17.6% had a chronic disease. The state and trait anxiety mean scores of the participants were 60.29 ± 6.13 and 44.18 ± 7.69, respectively. Statistically significant differences were found in the participants’ state and trait anxiety levels with respect to their age, gender, unit of work, marital status, status of having children and presence of a chronic disease (p < 0.05).
Conclusion
The state and trait anxiety levels of the healthcare workers in the study were found to be “severe” and “moderate,” respectively.
Similar content being viewed by others
Introduction
In December 2019, a new coronavirus infection (2019-nCoV) appeared as a cluster of mysterious pneumonia cases reported in Hubei, China. This disease, which quickly evolved into a pandemic, has been named COVID-19. It has rapidly spread from one person to another due to its transmission through respiratory droplets, causing the number of infected people to be higher than initially expected and revealing it to be a serious public health issue (Ho et al. 2020; World Health Organization 2020).
Globalization has accelerated the spread of the disease across continents, causing exponential growth in cases of infection throughout most of the world in a very short time. All these developments have brought about some changes and problems. Anxiety, panic and fear in societies have become evident in almost every area, including economic concerns for individuals, physical and mental problems caused by social isolation, interruption of educational activities, withdrawal from production and stress due to social distancing (Qiu et al. 2020; Duan and Zhu 2020). Health systems, which were caught unprepared for such a pandemic, have faced various problems, mainly including lack of sufficient protective materials, excessive workload, loss of workforce and staff shortage. This has caused an unprecedented state of psychological stress, fear, anxiety and depression for healthcare workers (Lu et al. 2020). In particular, healthcare workers at hospitals have always been at the forefront of coping with pandemics, facing serious risks to fulfill their duties. Healthcare workers who are in close contact with COVID-19 patients are vulnerable to COVID-19 infection, and they are likely to spread the virus to their colleagues and family members (Lu et al. 2020; Lin et al. 2007; Lehmann et al. 2015). The difficulties and stress they experience may trigger common mental disorders, including anxiety, insomnia, somatization, obsessive-compulsive symptoms and depressive disorders (Bao et al. 2020; Mo et al. 2020; Zhang et al. 2020; Lai et al. 2020; Xiao et al. 2020). Additionally, the balance between self-sacrifice, an essential component of healthcare professional duty, and personal fear for oneself and one’s family often causes conflict and maladjustment in healthcare workers (Lu et al. 2020). This conflict and maladjustment are combined with patient care stress, leading to increased mental distress (Xiang et al. 2020). In this context, it is important to protect the morale and mental health of healthcare workers, because this affects the successful delivery of healthcare services. Most healthcare workers in isolation units and hospitals do not receive any support for their own mental healthcare (Duan and Zhu 2020; Xiang et al. 2020). Hospitals should focus on providing both psychological support and timely psychological assistance for improving the coping strategies of their employees. It is very important for healthcare workers to strengthen their emotions and coping strategies to effectively deal with pandemics in order to prevent and control these kinds of adverse events (Huang et al. 2020). Increased efforts are needed to manage anxiety and stress in this group and help them prevent burnout, depression and post-traumatic stress disorder in the longer term (Bao et al. 2020; Cullen et al. 2020). Research data are needed to develop evidence-based strategies to reduce the adverse psychological impacts and psychiatric symptoms of the COVID-19 pandemic (Wang et al. 2020).
The COVID-19 pandemic causes acute stress in the whole community, but its effect on healthcare workers is not fully known. It is also important to know the well-being and emotional resilience of healthcare workers and understand and demonstrate these effects to maintain primary healthcare services during the COVID-19 pandemic. At this time, as the world is experiencing the severe effects of the COVID-19 pandemic, there is no Turkish study about the anxiety levels of healthcare workers, making this study the first piece of research on this topic. In this regard, this study aimed to examine the effect of COVID-19 on the anxiety levels of healthcare employees.
Research questions
-
1.
What is the level of anxiety in healthcare workers?
-
2.
Is there a relationship between healthcare workers’ sociodemographic characteristics, status of being affected by the COVID-19 pandemic and anxiety levels?
Methods
Objective and type
This descriptive study was conducted to examine the level of anxiety in healthcare workers caused by the COVID-19 pandemic.
Design and data collection
As the COVID-19 virus is transmitted from person to person, competent authorities recommend people to stay at home during the pandemic in order to minimize face-to-face interaction. Therefore, an electronic survey was created by the researchers to involve the participants in the study. Their responses were also received online. The study focused on healthcare workers in Turkey during the COVID-19 pandemic, and it used the snowball sampling method. The survey was shared on health-related social media platforms (such as WhatsApp, Instagram, Twitter), and the respondents were asked to share it with others. Before starting the survey, the participants were informed about the purpose and content of the study, emphasizing that participation was on a voluntary basis. The participants’ identity information was not recorded in the survey.
The sample size was calculated as 677 using the formula with an unknown universe. The snowball method, one of the probabilistic sampling types, was used. The sample consisted of healthcare workers from any healthcare institution/organization who agreed to participate in the study. The study was conducted between 18 and 25 April 2020 with a total of 710 participants who agreed to participate in the study.
Inclusion Criteria:
-
Currently working at any healthcare institution/organization,
-
Being willing to participate in the study.
The data were collected using a sociodemographic questionnaire prepared by the researchers, in line with the literature and the State-Trait Anxiety Inventory. It required around 5 minutes to fill out the data collection forms.
Sociodemographic questionnaire
In this section, a total of 15 questions were asked. A total of seven questions were asked about age, gender, occupation, unit of work, marital status, having children and having chronic disease. In addition, eight questions were asked about the fear of coronavirus, staying anywhere outside home during the pandemic, being tested for COVID-19, having a colleague or relative being tested for COVID-19, currently or previously providing care/treatment to a COVID-19 patient, being trained/educated on how to approach patients who tested positive for COVID-19, needing psychological support during the pandemic, and considering measures for healthcare workers as adequate.
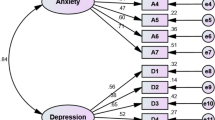
State-Trait Anxiety Inventory (STAI)
It was developed by Spielberger et al. (1970) to determine people’s state (Kvaal et al. 2005) and trait anxiety levels and adapted to Turkish by Öner and LeCompte (1985). The inventory consists of two separate scales. The State Anxiety Inventory is a self-assessment scale consisting of short and clear expressions to measure how the individual feels at a particular time and under certain conditions. It consists of questions that can be answered as “(1) not at all,” (2) “somewhat,” (3) “moderately so” and (4) “very much” to evaluate the anxiety levels of individuals included in a study. The Trait Anxiety Inventory mainly evaluates feelings of apprehension, tension, irritability and anxiety. It measures how an individual feels independent of their current state and conditions. The STAI is composed of two separate scales with a total of 40 items, whereby the State Anxiety Inventory consists of 20 items to evaluate how individuals feel “now,” whereas the Trait Anxiety Inventory consists of 20 items to evaluate how individuals feel “in general.” The State Anxiety Inventory rates one’s emotions or behaviors according to their severity, and the Trait Anxiety Inventory rates them according to their frequency, using a 4-point Likert-type scale. Each STAI item is given a weighted score of 1 to 4. Scores for both scales range from a minimum of 20 to a maximum of 80, where a higher score indicates a greater level of anxiety. STAI scores are interpreted as follows: 0–19, normal or no anxiety; 20–39, mild to moderate anxiety; 40–59, moderate to severe anxiety; 60–79, severe anxiety; and 80 and above, panic and crisis (Çakır and Özbayır 2018). The Cronbach’s alpha coefficients for the State and Trait Anxiety Inventories were calculated as 0.793 and 0.869, respectively.
Ethical considerations
Ethical approval was obtained for conducting the study (2020/22). The purpose of the study was included in the digitally prepared survey form, emphasizing the voluntary basis for participation in the study. This study was planned and conducted in accordance with the principles of the Declaration of Helsinki.
Data evaluation
The data were analyzed using IBM SPSS Statistics version 24.0 statistical software for Windows; the categorical variables are presented as frequencies and percentages, and the continuous variables are expressed as means ± standard deviations. Kolmogorov–Smirnov and Shapiro–Wilk tests were used to check the normality of the distribution of the data. Independent-samples t test and one-way analysis of variance (ANOVA) were used for the statistical analyses. The Bonferroni correction from post hoc tests was used to determine from which group the difference originated. The Cronbach’s alpha value was calculated for internal consistency. A p value less than 0.05 was considered statistically significant.
Results
The mean age and the mean work experience of the participants were 33.90 ± 8.56 and 10.74 ± 8.30 years, respectively. Among the participants, 46.8% were aged 26–35 years, 60.7% were female, 45.8% were nurses, 19.9% worked at coronavirus clinics (service, intensive care, emergency clinics), 63.7% were married, 58.0% had children and 17.6% had a chronic disease. Additionally, 82.1% of the participants were afraid of the COVID-19 pandemic, 24.2% had stayed outside their house due to the pandemic, 0.1% had tested positive for COVID-19, 12.0% had colleagues or relatives who had tested positive for COVID-19, 30.8% cared for COVID-19 patients, 52.8% received training on how to approach COVID-19 patients, 54.4% needed psychological support in this process, and 74.6% considered measures taken at their institutions/organizations to be inadequate (Table 1).
In these days of the severe COVID-19 pandemic, healthcare workers reported that they were most affected by the fear of transmitting the virus to others (78.9%), fear of becoming infected with the virus (55.5%), future anxiety (46.3%), sadness (45.9%), fear of being addicted to cleaning (33.0%) and fear of death (21.0%) (Chart 1).
The state and trait anxiety mean scores of the participants were 60.29 ± 6.13 and 44.18 ± 7.69, respectively (Table 2). Accordingly, 50.8% of the healthcare workers in the study had “severe” state anxiety, and 71.9% had “moderate” trait anxiety.
A statistically significant difference was determined in the healthcare workers’ state and trait anxiety levels with respect to their age, gender, unit of work, marital status, having children and presence of a chronic disease (p < 0.05). A statistically significant difference was determined in the healthcare workers’ state and trait anxiety levels with respect to their status of having fear due to the COVID-19 pandemic, being tested for COVID-19, being trained on how to approach patients who tested positive for COVID-19, needing psychological support in this process and considering measures for healthcare workers as adequate (p < 0.05) (Table 3).
In the advanced analysis, significant differences were found in the “State Anxiety” levels between age groups 19–25 years and 26–35 years (p = 0.026); between age groups 19–25 years and ≥ 46 years (p = 0.033); between working in coronavirus clinics and non-medical units (p = 0.028); between polyclinics and emergency room workers (p = 0.016) and polyclinics and ASM staff (p = 0.011); between working in polyclinics and non-medical units (p = 0.001); between those who had a positive COVID-19 test and those who did not test for COVID-19 (p = 0.037); and between those with a colleague or relative who received a positive COVID-19 test and those without.
Again in the advanced analysis, significant differences were found in the “Trait Anxiety” levels between age groups 19–25 years and ≥ 46 years (p = 0.023); between doctors and nurses (p = 0.001); between physicians and other healthcare professionals (p = 0.011); between working in surgery and in internal medicine clinics (p = 0.003); and between those who had a positive COVID-19 test and those who did not (p = 0.041) (Table 3).
Discussion
The COVID-19 pandemic has affected all continents, nations, races and individuals regardless of their socioeconomic levels, turning into one of the central health crises of a generation. Since COVID-19 is a highly contagious disease, there is a dramatically increased risk of transmission of the virus to healthcare workers (Lu et al. 2020). Although the rate of virus transmission to healthcare workers is unknown across the world, we assume that the figures are extremely high. Healthcare workers, who are at the forefront of the fight against the pandemic, care for each COVID-19 patient. Given that the pandemic can last for weeks or months, healthcare workers are more likely to encounter adverse conditions such as long-term exposure to the virus, increased workload, ethical dilemmas, lack of protective equipment, lack of effective medicines, poor social and medical support, loss of confidence, loss of social relationships and abnormalities in their daily routines (Lu et al. 2020; Qiu et al. 2020). All of these conditions increase anxiety. Therefore, this study was conducted to examine the level of anxiety caused by the COVID-19 pandemic in healthcare workers.
Anxiety is defined as “an unpleasant emotional state or condition perceived by individuals as ‘threatening’ or ‘dangerous’ to their basic values and existence,” and it is handled from two perspectives as state and trait anxiety. State anxiety may be defined as a transitory emotional state characterized by subjective feelings of apprehension and nervousness associated with activation (arousal) of the autonomic nervous system at a particular time. Therefore, state anxiety, which is accepted as temporary and short-term, comes into question while dealing with dangerous or threatening situations under a certain condition. In contrast, trait anxiety refers to a relatively stable individual difference and permanent personality trait in both anxiety tendency reflected as anxiety states manifested over time and probability of future anxiety (Spielberger 1972; Chew et al. 2020). This study found that state anxiety increased as the age of the healthcare workers increased, where those aged above 46 years had higher trait anxiety levels than the other age groups. There was a statistically significant difference in the participants’ state and trait anxiety levels with respect to their age (Table 3). Qiu et al. (2020) reported that individuals over 60 years of age had higher levels of psychiatric problems such as anxiety and depression during pandemics. One study concluded that young people had lower anxiety levels than the elderly (Huang et al. 2020). These results, which suggest that mental symptoms such as anxiety or depression are lower in young individuals than the elderly, may be associated with the fact that mortality increases as age increases.
The present study found a statistically significant relationship between gender and state-trait anxiety in healthcare workers, where women had significantly higher state and trait anxiety levels (Table 3). Studies conducted with healthcare workers during the pandemic have reported that women had higher anxiety levels (Chew et al. 2020; Huang et al. 2020), emotional issues such as stress and depression (Wang et al. 2020), and decreased social functionality (Qiu et al. 2020). The results of the current study were consistent with those in the literature.
This study revealed no statistically significant relationship between occupation and state anxiety, but it determined a statistically significant relationship between occupation and trait anxiety in healthcare workers (Table 3). Although there was no statistically significant relationship between occupation and state anxiety, all healthcare workers had “severe” state anxiety levels (Table 2). One study conducted in the general population during the pandemic reported that healthcare workers had higher levels of anxiety than those working in other sectors (Huang et al. 2020). Lai et al. (2020) reported that healthcare workers in direct contact with patients (especially nurses) and those working in cities with a high number of cases had higher anxiety levels. The current study found no statistically significant relationship between occupation and state anxiety, but it determined that nurses had higher state anxiety levels than the other healthcare workers (Table 3). Karasu and Çopur (2020) interviewed intensive care nurses and reported that they had high anxiety levels due to the pandemic. Healthcare workers who personally deal with patients are considered to be working at “ground zero,” where medical interventions such as care, treatment, intubation and aspiration are carried out in close contact with patients, increasing the risk of virus transmission. All occupational groups included in this study worked at healthcare institutions with a high probability of virus transmission, making them a high-risk group in this regard. This may be why healthcare workers in this study had high anxiety levels.
The study found a statistically significant relationship between the healthcare workers’ unit of work and their state-trait anxiety levels. The healthcare workers working at clinics with COVID-19 patients (service, intensive care and emergency clinics) had significantly higher state anxiety levels than those working at other clinics (Table 3). One study found that healthcare workers dealing with the diagnosis, treatment and care of COVID-19 patients had higher levels of symptoms of anxiety and depression (Lai et al. 2020). Another study found significantly higher fear, depression and anxiety levels in healthcare workers who worked at chest/respiratory, emergency, infectious disease and intensive care units and in close contact with infected patients (Lu et al. 2020). As suggested by both this study and other studies in the literature, as the intensity of contact with COVID-19 patients at a healthcare unit increases, the anxiety of those working at this unit increases, where those who work at units where contact is most frequent have the highest levels of anxiety.
This study determined that the married healthcare workers and those with children had significantly higher state-trait anxiety levels than those who were single (Table 3). Chew et al. (2020) conducted a study with healthcare workers during the pandemic, and they reported that the married healthcare workers experienced more physical symptoms of anxiety than single workers. This may be because those who are married are stressed by not seeing their spouses and children and have a high risk of carrying/transmitting the virus to their loved ones when they see and spend time with them. Mo et al. (2020) also stated that nurses have high work stress in pandemics, which is mostly associated with the status of having children. The causes of anxiety in healthcare workers include uncertainties at the workplace such as exposure to COVID-19, fear of transmitting the infection to their families and concerns about who would meet their personal and family needs if they were infected. Additionally, it should be noted that those with school-age children were also worried about who would take care of their children while schools were closed in this process (Shanafelt et al. 2020).
In this study, the healthcare workers with chronic diseases had significantly higher state-trait anxiety levels than those without any chronic disease (Table 3). One study reported that the anxiety, stress and depression levels of healthcare workers with low/poor perceived health increased during the pandemic (Huang et al. 2020). On the other hand, another study found that the anxiety, depression and obsessive-compulsive problems of healthcare workers were independent of their status of having a chronic disease. That study also reported that non-medical healthcare workers with chronic diseases had a high risk of experiencing anxiety, depression and obsessive-compulsive problems during the pandemic (Zhang et al. 2020). This was a noteworthy result.
This study found that both the state and trait anxiety levels were significantly higher in the healthcare workers who were afraid of the COVID-19 pandemic (Table 3). This may be because COVID-19 is a new disease and spread across the world quickly, with the global number of COVID-19-positive cases and deaths increasing with each passing day. There is still a lack of an effective drug or vaccine for COVID infection, and the number of COVID-19-positive cases and deaths is also increasing among healthcare workers. Therefore, it is important to take necessary precautions in this regard.
This study revealed significantly higher state anxiety levels in the healthcare workers who stayed anywhere outside their home due to the COVID-19 pandemic (Table 3). Accommodation of healthcare workers anyplace other than their homes is considered to increase their anxiety levels, as they disrupt their routine, stay in an unfamiliar environment, do not receive social support and become isolated (are unable to see their loved ones including spouse, children, parents), which increases their longing for their loved ones. The study also found that the healthcare workers who tested positive for COVID-19 and those who had a colleague or relative who tested positive for COVID-19 had higher state anxiety levels (Table 3). Fear of testing positive for COVID-19, having a colleague or relative testing positive for COVID-19, becoming infected with the virus or death due to virus infection, transmitting the virus to others, and staying apart or losing their loved ones might have caused anxiety in the healthcare workers.
In this study, the healthcare workers who received training on how to approach COVID-19 patients and those who cared for COVID-19 patients had significantly higher state anxiety levels (Table 3). Huang et al. (2020) reported that people who did not know about COVID-19 had lower anxiety levels. This result suggested that people with information about virus transmission pathways, disease course and outcomes better understand the magnitude of disease risk, and thus, they have higher anxiety levels. As the level of knowledge and experience about the disease increases, feelings of curiosity and anxiety about the course, spread and further progress of the disease may increase.
This study found that the healthcare workers who needed psychological support during the pandemic had significantly higher state and trait anxiety levels (Table 3). Tan et al. (2020) concluded that providing psychological support and counseling services to healthcare workers and developing support systems among their colleagues would reduce the psychological impact of the pandemic. Employees may need emotional and psychological support, especially due to the psychological impact of the COVID-19 pandemic. Providing social support for healthcare workers improves their self-efficacy, decreasing their anxiety, stress and depression levels (Xiao et al. 2020).
The current study also determined that the healthcare workers who considered measures taken at healthcare institutions/organizations as inadequate had significantly higher state and trait anxiety levels than those who did not (Table 3). Lack of access to appropriate personal protective equipment and inability to obtain current information have been found to increase anxiety (Shanafelt et al. 2020). Wang et al. (2020) reported that healthcare workers had low levels of stress, anxiety and depression when they were able to apply special measures (e.g. hand hygiene, wearing a mask). Adequate measures allow employees to protect themselves. Failure to take measures or inadequate measures increases the stress levels in employees by making them feel insecure.
In this study, more than half of the healthcare workers had “severe” state anxiety and “moderate” trait anxiety (Table 2). Chew et al. (2020) also reported that healthcare workers experienced moderate to severe anxiety during the pandemic. In 2003, severe acute respiratory syndrome (SARS) caused similar problems in healthcare workers, including high emotional distress, fear of transmission (Phua et al. 2005; Nickell et al. 2004; Maunder et al. 2004), stigma (Maunder et al. 2004; Bai et al. 2004) and worry about family (Nickell et al. 2004; Wong et al. 2005; Maunder 2004). Additionally, this study concluded that the healthcare workers experienced serious concerns such as virus transmission, virus infection, future anxiety and fear of death. The anxiety in healthcare workers may be explained by their concern that the pandemic will be continuous, and there is uncertainty about when it will end. Apart from the pandemic process, healthcare workers have to work under more severe conditions than many employees. Irregular working hours, prolonged hours at work, heavy workload, stress, risk of getting infectious diseases, facing stressed people and being exposed to verbal or physical assault are the main problems that many healthcare workers encounter while doing their job and which are considered to increase their trait anxiety. Healthcare workers should be supported to provide patients with quality and functional healthcare services and ensure their continuity in this pandemic period. It should be noted that healthcare workers try to flatten the pandemic curve, but the curve of their mental health problems caused by the pandemic should also be flattened after the pandemic.
Conclusion
The individuals most affected by this pandemic are those working at healthcare institutions/organizations. All those involved in management, physicians, nurses, support staff and other employees at these institutions have faced a situation that they had not known or experienced before but were suddenly forced to manage. The results of the study showed that the state and trait anxiety levels of the healthcare workers who were included in the study were “severe” and “moderate,” respectively, where those who needed psychological support and those who considered the measures taken at their healthcare institutions to be inadequate had higher state and trait anxiety levels.
For the quality and continuity of healthcare services, it is necessary to determine the physical and psychological experiences of healthcare workers in this pandemic period, take necessary precautions in this regard and implement relevant improvement efforts. Revealing their experiences during this period and conducting evidence-based research will help to guide similar situations in the future. It should be noted that after the pandemic has ended, the marks it leaves on society, especially on healthcare workers, are important, and understanding these marks in advance may aid in gradually reducing and finally eliminating their persistency.
Limitations
This study had some limitations. It was conducted in only one country. A device which supports the program was needed to complete the digital survey. Additionally, internet access and ability to complete the survey were required. Those without this skill were excluded from the study. Furthermore, the participation of healthcare workers in the study was limited due to the intensity of their activities across the country to combat the spread of COVID-19 infection.
References
Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P (2004) Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 55:1055–1057. https://doi.org/10.1176/appi.ps.55.9.1055
Bao Y, Sun Y, Meng S, Shi J, Lu L (2020) 2019-nCoV epidemic: address mental health care to empower society. Lancet 395(10224):e37–e38. https://doi.org/10.1016/S0140-6736(20)30309-3
Çakır SK, Özbayır T (2018) Assessment of patient anxiety levels before and after stoma surgery. Turk J Colorectal Dis 28:159–163. https://doi.org/10.4274/tjcd.15046.
Chew N, Lee G, Tan B, Jing M, Goh Y, Ngiam N et al (2020) A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. https://doi.org/10.1016/j.bbi.2020.04.049
Cullen W, Gulati G, Kelly BD (2020) Mental health in the Covid-19 pandemic. QJM 113(5):311–312. https://doi.org/10.1093/qjmed/hcaa110.
Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet 7(4):300–302. https://doi.org/10.1016/S2215-0366(20)30073-0.
Ho CS, Chee CY, Ho RC (2020) Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap 49(3):155–160
Huang L, Xu F, Liu H (2020) Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. MedRxiv. https://doi.org/10.1101/2020.03.05.20031898
Karasu F, Çopur EÖ (2020) COVID-19 Vakaları artarken salgının ön safındaki bir yoğun bakım hemşiresi: “cephede duran kahramanlar”. Yoğun Bakım Hemşireliği Dergisi 24(1):11–14
Kvaal K, Ulstein I, Nordhus IH, Engedal K (2005) The Spielberger State-Trait Anxiety Inventory (STAI): the state scale in detecting mental disorders in geriatric patients. Int J Geriatr Psychiatry 20(7):629–634. https://doi.org/10.1002/gps.1330.
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N et al (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3(3):e203976. https://doi.org/10.1001/jamanetworkopen
Lehmann M, Bruenahl CA, Löwe B, Addo MM, Schmiedel S, Lohse AW, Schramm C (2015) Ebola and psychological stress of health care professionals. Emerg Infect Dis 21:913–914. https://doi.org/10.3201/eid2105.141988.
Lin CY, Peng YC, Wu YH, Chang J, Chan CH, Yang DY (2007) The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J 24:12–17. https://doi.org/10.1136/emj.2006.035089.
Lu W, Wang H, Lin Y, Li L (2020) Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res 288:112936. https://doi.org/10.1016/j.psychres.2020.112936
Maunder R (2004) The experience of the 2003 SARS outbreak as a traumatic stress among frontline health care workers in Toronto: lessons learned. Philos Trans R Soc Lond Ser B Biol Sci 359(1447):1117–1125. https://doi.org/10.1098/rstb.2004.1483
Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D, Balderson K et al (2004) Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med 66:938–942. https://doi.org/10.1097/01.psy.0000145673.84698.18
Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, Qin M, Huang H (2020) Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. J Nurs Manag. https://doi.org/10.1111/jonm.13014
Nickell LA, Crighton EJ, Tracy CS, Al Enazy H, Bolaji Y, Hanjrah S et al (2004) Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ 170:793–798. https://doi.org/10.1503/cmaj.1031077.
Öner N, LeCompte WA (1985) Durumluk-Trait Anxiety envanteri el kitabı. Boğaziçi Üniversitesi Yayınları.
Phua DH, Tang HK, Tham KY (2005) Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad Emerg Med 12(4):322–328. https://doi.org/10.1197/j.aem.2004.11.015.
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry 33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213
Shanafelt T, Ripp J, Trockel M (2020) Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. https://doi.org/10.1001/jama.2020.5893
Spielberger CD (1972) Anxiety as an emotional state. In: Spielberger CD (ed) Anxiety: Current Trends in Theory and Research, vol 1, pp 23–49. https://doi.org/10.1016/B978-0-12-657401-2.50009-5
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the state-trait anxiety inventory. Consulting Psychologists Press, Palo Alto
Tan B, Chew N, Lee G, Jing M, Goh Y, Yeo L et al (2020) Psychological impact of the COVID-19 pandemic on health Care Workers in Singapore. Ann Intern Med M20–M1083. https://doi.org/10.7326/M20-1083
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17(5):1729. https://doi.org/10.3390/ijerph17051729.
Wong TW, Yau JK, Chan CL, Kwong RS, Ho SM, Lau CC et al (2005) The psychological impact of severe acute respiratory syndrome outbreak on health care workers in emergency departments and how they cope. Eur J Emerg Med 12:13–18. https://doi.org/10.1097/00063110-200502000-00005.
World Health Organization Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. Jan 11, 2020. https://www.who.int/internalpublications-detail/clinicalmanagement-of-severe-acute-respiratoryinfection-when-novel-coronavirus-(ncov)-infection-is-suspected Accessed 30 Jan 2020
Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH (2020) Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7(3):228–229. https://doi.org/10.1016/S2215-0366(20)30046-8
Xiao H, Zhang Y, Kong D, Li S, Yang N (2020) The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 26:e923549. https://doi.org/10.12659/MSM.923549.
Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M et al (2020) Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 9:1–9. https://doi.org/10.1159/000507639.
Acknowledgements
We would like to thank all those who contributed to this study.
Author information
Authors and Affiliations
Contributions
Fatma Karasu: Study conception/design, drafting of manuscript, critical revisions for important intellectual content; supervision, statistical expertise, administrative/technical/material support.
Ebru Öztürk Çopur: Study conception/design, drafting of manuscript, critical revisions for important intellectual content; supervision, administrative/technical/material support.
Duygu Ayar: Study conception/design, drafting of manuscript, critical revisions for important intellectual content; supervision, administrative/technical/material support.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest among the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karasu, F., Öztürk Çopur, E. & Ayar, D. The impact of COVID-19 on healthcare workers’ anxiety levels. J Public Health (Berl.) 30, 1399–1409 (2022). https://doi.org/10.1007/s10389-020-01466-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-020-01466-x