Analysis of the mental health status of hospital staff during the COVID-19 pandemic
Abstract
BACKGROUND:
Medical work is a complex and interpersonally sensitive job; clinicians interact with patients, colleagues and society-at-large daily, and they are under pressure from a variety of sources. The doctor–patient relationship is of particular concern.
OBJECTIVE:
To investigate the current mental health status of hospital staff and related influencing factors during the coronavirus disease 2019 (COVID-19) pandemic.
METHODS:
The Symptom Checklist-90 (SCL-90) and Generalized Anxiety Disorder Scale-7 (GAD-7) were used to survey the current mental health status of hospital employees. The resulting qualitative data was described in the form of frequency and percentage (%), and the quantitative data were expressed as mean±standard deviation (
RESULTS:
A total of 1,074 employees of The Third Xiangya Hospital of Central South University participated in the mental health survey, of whom 77.47% were women. The SCL-90 score was 133.89±48.87, and the three highest scoring factors were depression, somatisation and obsessions, with factor scores of 19.10±8.14, 16.78±6.21 and 16.27±6.39, respectively. The GAD-7 score was 3.74±4.17 for women and 2.14±3.55 for men. The number of women with anxiety disorders was higher compared with men.
CONCLUSION:
The mental health status of hospital workers with different demographic characteristics varied greatly during the COVID-19 pandemic. Active attention needs to be paid to the mental health status of hospital staff.
1Introduction
The coronavirus disease 2019 (COVID-19) outbreak represents a serious public health threat worldwide. In addition to physical health, the potential impact of COVID-19 on mental health should also be given attention [1]. Previous studies have shown that, compared with physical injuries, major disasters have broader and longer-lasting psychological effects on people [2, 3]. This is especially true for healthcare workers, the main participants in this study.
The social impact of COVID-19 includes problems with family communication, increased smoking and domestic violence. The economic impact includes the inability to work in isolation, and the psychological impact includes stress, anxiety, loneliness, depression and burnout [4, 5]. This also increases the risk of psychological morbidity for healthcare workers (HCWs) responding to emergencies such as the unprecedented number of critically ill patients, the often-unpredictable disease course, high mortality rates and the lack of effective treatments or guidelines [6].
Studies from China, Italy, Turkey, Spain and Iran reported a higher prevalence of mental disease among healthcare workers compared with the overall public [7–9]. Existing research also showed that, compared with non-medical health workers, medical health workers have a higher prevalence of insomnia (38.4% vs 30.5%), anxiety (13.0 vs 8.5%), depression (12.2 vs 9.5%), somatisation (1.6 vs 0.4%) and obsessive-compulsive symptoms (5.3 vs 2.2%) [10]. The burden of the current epidemic on HCWs deserves close attention, as the individuals involved in the diagnosis, treatment, and care of COVID-19 patients are at high risk of experiencing psychological distress and other mental health symptoms. Therefore, psychological interventions for at-risk individuals with significant psychological distress are needed.
The World Health Organization (WHO) clearly states that health refers not only to the absence of physical disease but also to a good state of physical, mental, social and moral well-being. Psychology and physiology influence each other, promote each other and interact as cause and effect, and psychological health is a key determinant for overall health. Stable emotions and a healthy psychological state are especially important for medical staff, not only for their physical health but also to help them better complete the work of treating patients and saving lives.
Physicians’ psychological conditions are likely to have an impact on their occupational burnout. In addition, the high expectations of society, the mismatch between remuneration compared with stress and effort and the lack of social support may be important predictors of occupational burnout in doctors [11, 12]. A meta-analysis reported high rates of burnout among men living in Asian and North American countries who are working as medical and surgical residents [13, 14]. Another meta-analysis reported a high incidence of burnout among young paediatric nurses in the sub-Saharan African region of the world [15]. These factors also influence the psychological states, coping styles and stress behaviours of these individuals.
Exploring the psychological status of clinicians and understanding their coping methods is of great significance for promoting assistance and guidance that will help these practitioners reduce inappropriate or harmful stress behaviours. Medical work is a complex and interpersonally sensitive job; clinicians interact with patients, colleagues and society-at-large daily, and they are under pressure from a variety of sources. The doctor–patient relationship is of particular concern.
On 22 February 2019, the Institute of Psychology of the Chinese Academy of Sciences released the China Mental Health Development Report (2017–2018), in which healthcare workers were described as a population in need of attention. It stated that hospitals should focus on boosting the enthusiasm of medical staff through efforts including salary and treatment enhancements, improved development spaces and practice environments and better demonstrations of respect and care for the employees. It also noted the need for a strengthening of the sense of professional honour for medical staff through a variety of formats to create a good culture of respect for medical and health care throughout society. Therefore, a psychological survey was conducted in our hospital to understand the current state of mental health of its staff and to ascertain influencing factors during the COVID-19 pandemic.
2Participants and methods
2.1Research participants
In this cross-sectional survey, a total of 1074 employee responses were retrieved between 1 and 31 May 2020. The surveys included personal assessments of fear, anxiety and depression, as well as information on gender, age, working years, education, and the marital and fertility status of each respondent. Complete questionnaires finished within two days were recognised as eligible and included in the following analysis. All questionnaires were completed online by volunteer participants.
The inclusion criteria were determined to evaluate participating staff who consented to psychological intervention and who had been employed at the hospital for at least one year as of May 2020. Respondents who turned in incomplete questionnaires or had a history of psychological or cognitive disorders were excluded from the study.
2.2Symptom Checklist-90
Symptom Checklist 90 (SCL-90) is a 90-item neuropsychological assessment tool which is frequently used both domestically and abroad [16]. This scale is the most frequently used screening scale for the examination of mental disorders and psychological disorders and has good reliability and validity [17, 18]. The SCL-90 covers items involving psychiatric symptomatology such as sensation, emotion, thinking, consciousness, behaviour and lifestyle habits. Nine dimensions from somatisation, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, terror, paranoia ideation and psychoticism are used to reflect the psychological symptoms and to achieve mental health assessment and screening of psychological problems, as well as to provide individuals with personalised mental health promotion management recommendations. Respondents are rated on a five-point Likert-type scale (score 0 [no significant physical symptoms] to 5 [extremely heavy]). In the present study, the Cronbach alpha coefficients for subscales were in the range of0.87–0.91.
2.3Generalized Anxiety Disorder Scale-7
The Generalized Anxiety Disorder Scale-7 (GAD-7) is used to identify patients with underlying generalised anxiety disorder and is commonly used to assess the severity of general anxiety symptoms due to its good operational properties [19, 20]. The GAD-7 uses a four-point Likert-type scale ranging from ‘0 = not at all’ to ‘3 = almost every day’ to indicate the presence of symptoms such as ‘feeling nervous, mild anxious, or severely anxious’ with a total score of 0–21. A score of 0–4 indicates normal anxiety, 5–9 indicates mild anxiety, 10–14 indicates moderate anxiety and 15–21 indicates severe anxiety. In the present study, the Cronbach alpha coefficientwas 0.93.
2.4Statistical analysis methods
The data were analysed via SPSS 26.0 software. Qualitative variables were described by frequency distribution (%), while quantitative variables were described by the mean±standard deviation (
3Results
3.1Basic characteristics of the research participants
A total of 1074 hospital employees participated in the mental health survey, of whom 832 (77.47%) were female and 242 (22.53%) were male. 48.42% of the surveyed employees were 31–40 years old; 441 were female and 79 were male. The educational level of the surveyed population was generally a completed bachelor’s degree (62.7%), with 69.1% of this group composed of (575) females and 40.5% (98) composed of males. 606 (72.8%) females were on nursing staff and 61 (25.2) males were doctors. The titles of the surveyed workers were generally intermediate level (56.1%), of which 504 were female and 99 were male; the largest number of people by administrative level were clerks (50.9%), of whom 416 were women and 131 were men (see Table 1). There was no statistical difference between males and females in age, marital status, education level, jobs, title or administrative level (p < 0.05).
Table 1
Table of basic characteristics of 1074 hospital workers n (%)
| Variables | Female (n = 832) | Male (n = 242) | Total (n = 1074) |
| Age | |||
| 20 years old and below | 1(0.1) | 0(0.0) | 1(0.1) |
| 21–30 years old | 218(26.2) | 47(19.4) | 265(24.7) |
| 31–40 years old | 441(53.0) | 79(32.6) | 520(48.4) |
| 41–50 years old | 162(19.5) | 65(26.9) | 227(21.1) |
| 51–60 years old | 9(1.1) | 50(20.7) | 59(5.5) |
| 61–70 years old | 1(0.1) | 1(0.4) | 2(0.2) |
| Marital status | |||
| Divorced | 22(2.6) | 6(2.5) | 28(2.6) |
| Widowed | 2(0.2) | 0(0.0) | 2(0.2) |
| Unmarried | 155(18.6) | 33(13.6) | 188(17.5) |
| Married | 653(78.5) | 203(83.9) | 856(79.7) |
| Education level | |||
| Elementary school and below | 3(0.4) | 0(0.0) | 3(0.3) |
| Junior High School | 1(0.1) | 8(3.3) | 9(0.8) |
| High School | 21(2.5) | 30(12.4) | 51(4.7) |
| University | 575(69.1) | 98(40.5) | 673(62.7) |
| Master | 180(21.6) | 52(21.5) | 232(21.6) |
| PhD | 52(6.3) | 54(22.3) | 106(9.9) |
| Jobs | |||
| Doctors | 59(7.1) | 61(25.2) | 120(11.2) |
| Medical technician | 75(9.0) | 58(24.0) | 133(12.4) |
| Nursing | 606(72.8) | 32(13.2) | 638(59.4) |
| Administration | 43(5.2) | 28(11.6) | 71(6.6) |
| Logistics | 16(1.9) | 38(15.7) | 54(5.0) |
| Other | 33(4.0) | 25(10.3) | 58(5.4) |
| Title | |||
| Primary | 221(26.6) | 61(25.2) | 282(26.3) |
| Intermediate | 504(60.6) | 99(40.9) | 603(56.1) |
| Associate | 33(4.0) | 30(12.4) | 63(5.9) |
| High | 3(0.4) | 8(3.3) | 11(1.0) |
| None | 71(8.4) | 44(18.2) | 115(10.7) |
| Administrative Level | |||
| Clerk | 416(50.0) | 131(54.1) | 547(50.9) |
| Deputy Chief | 9(1.1) | 16(6.6) | 25(2.3) |
| Section Chief | 11(1.3) | 13(5.4) | 24(2.2) |
| Deputy director | 0(0.0) | 1(0.4) | 1(0.1) |
| None | 396(47.6) | 81(33.5) | 477(44.4) |
3.2SCL-90 findings
The 1074 hospital workers returned SCL-90 scores in the range of 0–439 (133.89±48.87), and the top three highest scoring factors were depression, somatisation and obsessive-compulsive behaviour, with factor scores of 19.10±8.14, 16.78±6.21 and 16.27±6.39, respectively. Women scored significantly higher than men on most factors except paranoia (see Tables 2 and 3).
Table 2
SCL-90 scores and ranking of each factor for 1074 hospital workers
| Factor name | Factor score | Rank |
| Somatization | 16.78±6.21 | 2 |
| Hostility | 8.47±3.46 | 7 |
| Obsessive–compulsive | 16.27±6.39 | 3 |
| Terror | 8.32±3.15 | 8 |
| Interpersonal relationships | 12.41±4.95 | 6 |
| Paranoia | 7.78±3.10 | 9 |
| Depression | 19.10±8.14 | 1 |
| Psychotic | 12.62±4.68 | 5 |
| Anxiety | 13.60±5.38 | 4 |
| Anxiety disorders | 3.38±4.10 | 10 |
Table 3
Gender difference in factor scores
| Factor name | Factor score | t | p | |
| Female (n = 832) | Male (n = 242) | |||
| Somatization | 17.26±6.51 | 15.11±4.63 | –4.79 | <0.001 |
| Hostility | 8.73±3.63 | 7.60±2.65 | –4.51 | <0.001 |
| Obsessive–compulsive | 16.82±6.55 | 14.35±5.40 | –5.37 | <0.001 |
| Terror | 8.47±3.37 | 7.83±2.15 | –2.76 | 0.006 |
| Interpersonal relationships | 12.66±5.15 | 11.57±4.11 | –3.02 | 0.003 |
| Paranoia | 7.86±3.20 | 7.49±2.75 | –1.66 | 0.098 |
| Depression | 19.50±8.40 | 17.71±7.00 | –3.03 | 0.002 |
| Psychotic | 12.79±4.85 | 12.06±4.01 | –2.12 | 0.034 |
| Anxiety | 13.94±5.63 | 12.45±4.22 | –3.82 | <0.001 |
| Anxiety disorders | 3.74±4.17 | 2.14±3.55 | –5.90 | <0.001 |
A small proportion of the 1074 respondents had extremely severe symptom manifestations on all factors. In terms of different genders, the proportion of males with no significant symptoms at any factors levels was higher than that of females, and those with extremely severe symptoms were all females (see Table 4).
Table 4
Table of results of severity of each factor of SCL-90 in 1074 hospital workers n(%)
| Variables | Female (n = 832) | Male (n = 242) | Total (n = 1074) |
| Somatization | |||
| No significant physical symptoms | 598(71.9) | 197(81.4) | 795(74.0) |
| Mild | 191(23.0) | 43(17.8) | 234(21.8) |
| Moderate | 35(4.2) | 2(0.8) | 37(3.4) |
| Severe | 7(0.8) | 0(0.0) | 7(0.7) |
| Extremely heavy | 1(0.1) | 0(0.0) | 1(0.1) |
| Hostilization | |||
| No obvious hostile symptoms | 614(73.8) | 203(83.9) | 817(76.1) |
| Mild | 164(19.7) | 34(14.0) | 198(18.4) |
| Moderate | 39(4.7) | 5(2.1) | 44(4.1) |
| Severe | 13(1.6) | 0(0.0) | 13(1.2) |
| Extremely heavy | 2(0.2) | 0(0.0) | 2(0.2) |
| Obsessive-compulsive | |||
| No obvious obsessive-compulsive symptoms | 450(54.1) | 174(71.9) | 624(58.1) |
| Mild | 299(35.9) | 54(22.3) | 353(32.9) |
| Moderate | 66(7.9) | 12(5.0) | 78(7.3) |
| Severe | 14(1.7) | 2(0.8) | 16(1.5) |
| Extremely heavy | 3(0.4) | 0(0.0) | 3(0.3) |
| Terror | |||
| No obvious terror symptoms | 721(86.7) | 222(91.7) | 943(87.8) |
| Mild | 87(10.5) | 18(7.4) | 105(9.8) |
| Moderate | 16(1.9) | 2(0.8) | 18(1.7) |
| Severe | 4(0.5) | 0(0.0) | 4(0.4) |
| Extremely heavy | 4(0.5) | 0(0.0) | 4(0.4) |
| Interpersonal relationships | |||
| No significant interpersonal sensitivity symptoms | 600(72.1) | 193(79.8) | 793(73.8) |
| Mild | 188(22.6) | 41(16.9) | 229(21.3) |
| Moderate | 33(4.0) | 6(2.5) | 39(3.6) |
| Severe | 9(1.1) | 2(0.8) | 11(1.0) |
| Extremely heavy | 2(0.2) | 0(0.0) | 2(0.2) |
| Paranoia | |||
| No obvious symptoms of paranoia | 682(82.0) | 203(83.9) | 885(82.4) |
| Mild | 113(13.6) | 33(13.6) | 146(13.6) |
| Moderate | 29(3.5) | 5(2.1) | 34(3.2) |
| Severe | 8(1.0) | 1(0.4) | 9(08) |
| Depression | |||
| No significant depressive symptoms | 547(65.7) | 174(71.9) | 721(67.1) |
| Mild | 222(26.7) | 55(22.7) | 277(25.8) |
| Moderate | 43(5.2) | 10(4.1) | 53(4.9) |
| Severe | 16(1.9) | 3(1.2) | 19(1.8) |
| Extremely heavy | 4(0.5) | 0(0.0) | 4(0.4) |
| Psychotic | |||
| No obvious psychotic symptoms | 696(83.7) | 210(86.8) | 906(84.4) |
| Mild | 105(12.6) | 26(10.7) | 131(12.2) |
| Moderate | 25(3.0) | 6(2.5) | 31(2.9) |
| Severe | 4(0.5) | 0(0.0) | 4(0.4) |
| Extremely heavy | 2(0.2) | 0(0.0) | 2(0.2) |
| Anxiety | |||
| No significant anxiety symptoms | 641(77.0) | 208(86.0) | 849(79.1) |
| Mild | 142(17.1) | 29(12.0) | 171(15.9) |
| Moderate | 40(4.8) | 5(2.1) | 45(4.2) |
| Severe | 8(1.0) | 0(0.0) | 8(0.7) |
| Extremely heavy | 1(0.1) | 0(0.0) | 1(0.1) |
| Anxiety disorders | |||
| Anxiety without clinical significance | 550(66.1) | 199(82.2) | 749(69.7) |
| Mild | 213(25.6) | 30(12.4) | 243(22.6) |
| Moderate | 46(5.5) | 9(3.7) | 55(5.1) |
| Severe | 23(2.8) | 4(1.7) | 27(2.5) |
Results from T-tests and one-way ANOVA indicated significant group differences in the demographic variables of gender (t = –3.90, p < 0.001), education level (F = 4.85, p < 0.001) and jobs (F = 6.67, p < 0.001). Regression analysis showed that gender, education level and jobs had a significant effect on SCL-90 total scores (βgender = 0.071, p = 0.026; βeducation level = –0.098, p = 0.004; βjobs = –0.149, p < 0.001) (see Tables 5 and 6).
Table 5
Demographic differences in SCL-90 total scores
| Variables | M±SD | t/F | p |
| Total | 115.35±41.92 | ||
| Gender | –3.90 | <0.001 | |
| Female | 118.03±43.70 | ||
| Male | 106.16±33.64 | ||
| Age | 2.05 | 0.069 | |
| Below 20 years old | 122 | ||
| 21–30 years old | 111.49±37.20 | ||
| 31–40 years old | 119.45±44.50 | ||
| 41–50 years old | 112.42±42.32 | ||
| 51–60 years old | 108.00±34.52 | ||
| Above 60 years old | 108.50±34.65 | ||
| Marital status | 0.38 | 0.766 | |
| Divorced | 122.21±50.19 | ||
| Widowed | 101 | ||
| Unmarried | 116.52±42.01 | ||
| Married | 114.88±41.65 | ||
| Education level | 4.85 | <0.001 | |
| Elementary school and below | 137.67±5.69 | ||
| Junior high school | 96.22±19.45 | ||
| High school | 97.22±24.54 | ||
| University | 118.79±44.71 | ||
| Master | 114.79±39.57 | ||
| PhD | 104.30±31.71 | ||
| Jobs | 6.67 | <0.001 | |
| Doctors | 110.51±41.91 | ||
| Medical technician | 121.01±45.70 | ||
| Nursing | 108.33±33.77 | ||
| Administration | 109.27±33.13 | ||
| Logistics | 100.42±25.06 | ||
| Other | 100.60±22.46 | ||
| Title | 1.84 | 0.102 | |
| Primary | 114.41±41.47 | ||
| Intermediate | 118.08±43.67 | ||
| Associate | 108.85±30.56 | ||
| High | 107.17±35.84 | ||
| Administrative level | 0.59 | 0.669 | |
| Clerk | 109±28.64 | ||
| Deputy chief | 110.92±28.64 | ||
| Section chief | 114.22±44.41 | ||
| Deputy director | |||
| None | 117.21±40.01 |
Table 6
Regression analysis results of SCL-90 total scores
| Outcome variable | β | t | p | |
| SCI-90 total score | Constant | 10.89 | <0.001 | |
| Gender | 0.071 | 2.23 | 0.026 | |
| Education level | –0.098 | –2.86 | 0.004 | |
| Jobs | –0.149 | –4.23 | <0.001 |
Note: R2 = 0.031, adjusted R2 = 0.028; β, Standardized Coefficients Beta.
3.3GAD-7 findings
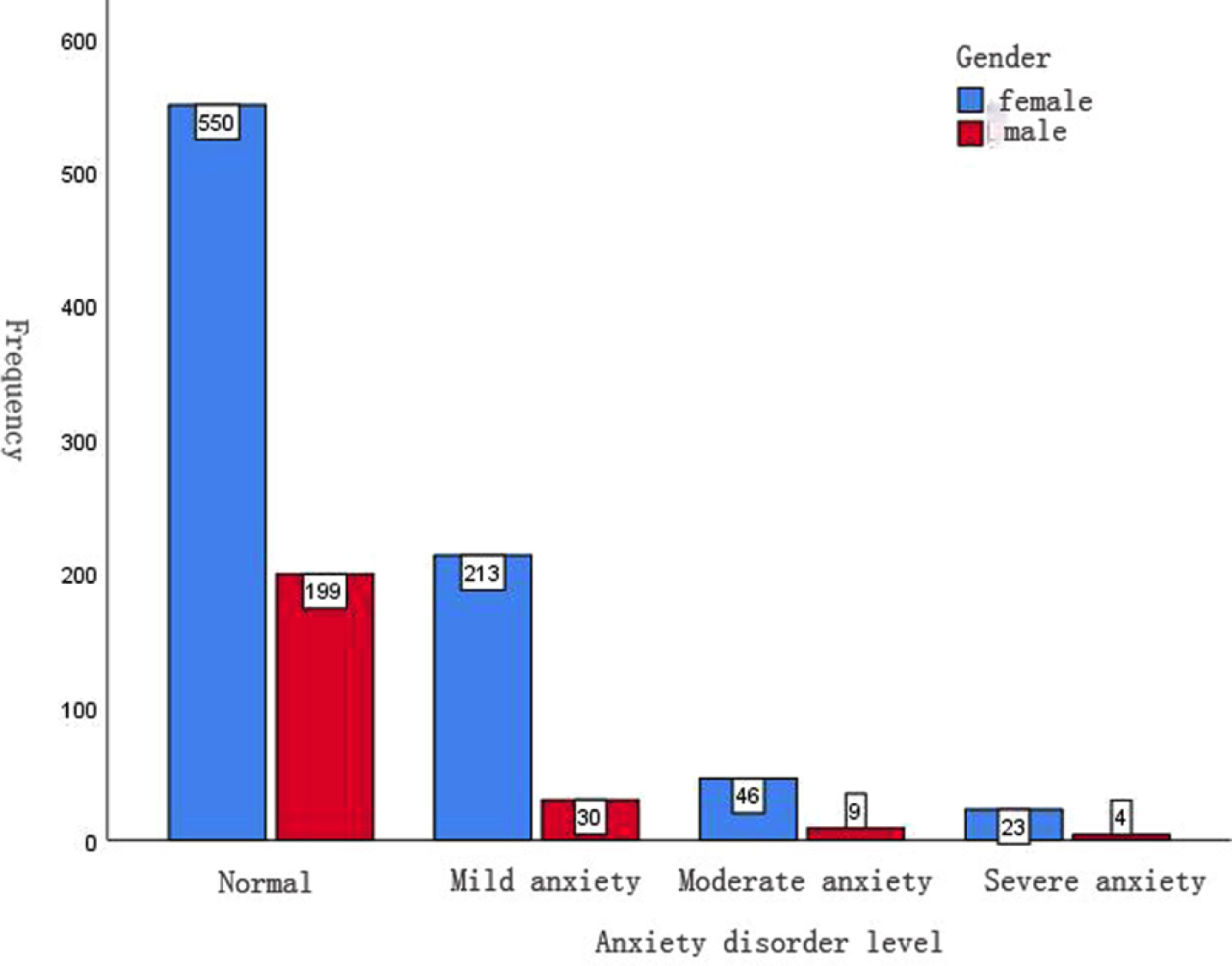
The GAD-7 score of 1074 hospital workers was 3.38±4.10, and in terms of gender, the GAD-7 score of women was 3.74±4.17 and the GAD-7 score of men was 2.14±3.55. The GAD-7 scores of women were significantly higher than those of men (see Table 7). The number of women with anxiety disorders was higher than that of men, and the number of women with mild disorders was the highest, with a total of 213. There were 46 with moderate disorders and 23 with severe disorders (see Fig. 1).
Table 7
Table of GAD-7 scores of 1074 hospital workers
| Variables | M±SD | t/F | p |
| Total | 3.38±4.10 | ||
| Gender | –5.41 | <0.001 | |
| Female | 3.74±4.17 | ||
| Male | 2.14±3.55 | ||
| Age | 3.22 | 0.007 | |
| 21–30 years old | 3.34±3.73 | ||
| 31–40 years old | 3.78±4.25 | ||
| 41–50 years old | 2.89±4.17 | ||
| 51–60 years old | 2.08±3.65 | ||
| Marital status | 0.43 | 0.733 | |
| Divorced | 2.96±4.65 | ||
| Widowed | 1.00±1.41 | ||
| Unmarried | 3.62±4.25 | ||
| Married | 3.35±4.05 | ||
| Education level | 5.36 | <0.001 | |
| Elementary school and below | 9.33±4.16 | ||
| Junior high school | 1.00±1.73 | ||
| High school | 1.61±3.24 | ||
| University | 3.63±4.25 | ||
| Master | 3.47±3.80 | ||
| PhD | 2.51±3.81 | ||
| Jobs | 6.52 | <0.001 | |
| Doctors | 2.92±435 | ||
| Medical technician | 2.66±3.21 | ||
| Nursing | 3.92±4.28 | ||
| Administration | 2.83±4.14 | ||
| Logistics | 1.61±2.48 | ||
| Other | 2.36±3.42 | ||
| Title | 1.89 | 0.094 | |
| Primary | 3.38±3.93 | ||
| Intermediate | 3.60±4.17 | ||
| Associate | 2.67±3.84 | ||
| High | 2.76±4.09 | ||
| Administrative level | 1.29 | 0.272 | |
| Clerk | 3.31±4.25 | ||
| Deputy chief | 3.04±3.12 | ||
| Section chief | 1.88±3.04 | ||
| Deputy director | |||
| None | 3.56±3.99 |
Fig. 1
Histogram of the GAD-7 anxiety disorder scale for 1074 hospital workers.
Results from T-tests and one-way ANOVA indicated significant group differences in demographic variables of gender (t = –5.41, p < 0.001), age (F = 3.22, p = 0.007), education level (F = 5.36, p < 0.001) and jobs (F = 6.52, p < 0.001). Regression analysis showed that gender and jobs had a significant effect on GAD-7 scores (βgender = 0.128, p < 0.001; βjobs = –0.107, p = 0.003) (see Table 8).
Table 8
Regression analysis results of GAD-7 scores
| Outcome variable | β | t | p | |
| SCI-90 total score | Constant | 2.65 | 0.008 | |
| Gender | 0.128 | 3.94 | <0.001 | |
| Age | –0.009 | –0.264 | 0.791 | |
| Education level | –0.058 | –1.71 | 0.088 | |
| Jobs | –0.107 | –2.94 | 0.003 |
Note: R2 = 0.035, adjusted R2 = 0.032.
4Discussion and conclusion
4.1Main findings
In this study, we found that women had higher scores on the SCL-90 and the GAD-7 than men, and the number of women with anxiety disorders was higher than men in all cases, which may be due to the large difference in the gender structure of our staff. Factors such as job and education have a greater impact on the mental health of HCWs. Work stress and the doctor–patient relationship may make these individuals more vulnerable to mental health problems than others.
4.2Analysis of the influencing factors on the mental health of hospital workers
4.2.1The mental health status of male and female workers differed greatly
Results of the SCL-90 scale scores showed that women scored higher than men on all factor levels except paranoia, the proportion of men without significant symptoms was higher than women on all factor levels, and those with very severe symptoms were all women.
The mean score on the GAD-7 scale was 3.38±4.10, with women scoring higher than men. The number of women with anxiety disorders was higher than men in all cases. This is due to the large difference in the gender structure of our staff.
Prior studies have found that mental health problems are more severe in women. Foreign studies have found that female medical staff generally suffer from subjective physical discomfort and lower moods [21]. In addition, other studies have found that depressive symptoms occur more often in women than in men [22], the prevalence of depression among female physicians is about 1.5 times higher than that of men and the prevalence of severe depression is about eight times higher [23]. The results of domestic studies indicate that the mental health quality of female medical personnel is lower than that of men [24–26].
4.2.2Jobs have a greater impact on mental health
Regression analysis showed that jobs had a significant effect on SCL-90 total scores and GAD-7 scores. Among all the types of occupations of HCWs, medical technicians had the highest SCL-90 total scores, and nurses had the highest GAD-7 scores. Doctors ranked second in both SCL-90 total scores and GAD-7 scores.
The medical personnel mentioned above are all front-line workers in the hospital. Factors such as work stressors and doctor–patient relationships may make them more vulnerable to mental health problems than others [27], so more attention should be paid to these people.
4.2.3Education has a greater impact on mental health
Regression analysis showed education level had a significant effect on SCL-90 total scores; those whose highest level of schooling was elementary school and below had the highest SCL-90 total scores.
The results of this study showed that marital status was not a factor influencing the mental health of hospital workers. However, the findings of Wang et al. showed that the mental health of unmarried personnel was lower [28]. Unmarried healthcare workers are more likely to have mental health problems as they experience the dual pressure of career and family. Their careers are in a period of vigorous development. At the same time, they are taking on the obligations of household chores and supporting the elderly alone [29].
4.2.4The mental health of healthcare workers during the COVID-19 pandemic
Given that the COVID-19 pandemic continues in 2022, it is necessary to consider its impact on the mental health of healthcare workers. COVID-19 has had a significant impact on the mental health of everyone from the public to healthcare workers in several countries and regions [30–34]. Post-traumatic stress disorder was reported to be the most common mental health disorder reported by healthcare workers during the COVID-19 pandemic, followed by anxiety, depression and distress [35]. Participants perceived high risk of infection with COVID-19, and they also perceived an inadequate workplace response to the pandemic [28]. The above factors were partially reflected in the participants of this study.
4.3Recommendations
4.3.1Establish a mental health promotion management programme
Based on the results of the mental health assessment of hospital staff, researchers can develop mental health promotion solutions for healthcare workers, carry out mental health management, improve the mental health of healthcare workers and effectively prevent psychosomatic diseases. A good mental status and psychological quality of life are the basic foundations for better work. Through mental health promotion, HCWs can pay more attention to their mental health, remain mindful of their mental status and adjust negative emotions, thus purposefully improving their work and life situation to conduct busy jobs with a more positive and optimistic mental outlook. In addition, a regular psychological examination can also timely identify the state of healthcare workers at the edge of a psychological crisis, which will be helpful for early intervention with psychological assistance and timely and effective intervention to curb the occurrence of malignant adverse events.
4.3.2Establish a personalised adaptive psychological intervention system
Xuan et al. proposed an integrated approach including improved risk communication, safety training and psychological support programmes for all hospital staff [28]. After HCWs completed the psychological physical examination through the self-help mental health service platform, the software system (uniform information management platform for hospital) developed an individualised psychological training programme for them, based on the results of psychological assessment. Firstly, a self-help adaptive intervention platform will intervene with the psychological problems of HCWs. This platform will promote universal mental health knowledge, and provide assistance with emotional management, stress management and interpersonal communication through psychological animation, electronic magazines, music therapy and psychological training.
4.3.3Develop an annual digital mental health promotion training course and internet cognitive behaviour therapy
Cognitive behaviour therapy (CBT) has the highest amount of evidence demonstrating its effectiveness. A digital version, Internet CBT (iCBT), can deliver such care while preventing the spread of infection during the pandemic [36]. It has been reported that iCBT can treat psychiatric symptoms such as insomnia [37]. The digital training programme provides step-by-step psychological training for healthcare workers to help them improve their mental health, enhance their ability to cope with crises, prevent psychological problems and develop positive psychological qualities. The digital training courses are conducted through remote training methods, allowing healthcare professionals to freely choose their training time without interfering with their daily work and life, with online self-help as the main mode.
5Limitations and future directions
This was an observational study, and the lack of a randomised sampling method may have resulted in a small sample size. Furthermore, as the study did not utilise a standardised clinical interview for diagnosis, it is not known whether a disease was actually present. At the same time, the lack of a control group limits the generalisability of the results. Future research will still need to design and evaluate the effectiveness of psychological and therapeutic interventions.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of The Third Xiangya Hospital of Central South University (Approval number: 2021-S462). Written informed consent was obtained from all participants.
Conflict of interest
None of the authors have any personal, financial, commercial, or academic conflicts of interest to report.
Acknowledgments
The authors are grateful for the contributions of the panel of the Third Xiangya Hospital, Central South University, and all participants for data collection support. They furthermore thank the project team members for all work and energy on important insights about the project.
Funding
The study was supported by the Key Research and Development Program of Hunan Province (2020SK2090) and the Natural Science Foundation of Hunan Province (2019JJ40409).
References
[1] | Luo M , Guo LX , Yu MZ , Jiang WY , Wang HY . The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res. (2020) ;291: :113190. doi: 10.1016/j.psychres.2020.113190. |
[2] | Murat M , Köse S , Savaşer S . Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) ;30: (2):533–43. doi: 10.1111/inm.12818. |
[3] | Kayabınar E , Kayabınar B , Önal B , Zengin HY , Köse N . The musculoskeletal problems and psychosocial status of teachers giving online education during the COVID-19 pandemic and preventive telerehabilitation for musculoskeletal problems. Work. (2021) ;68: (1):33–43. doi: 10.3233/WOR-203357. |
[4] | Clay JM , Parker MO . Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? The Lancet Public Health. (2020) ;5: (5):e259. doi: 10.1016/S2468-2667(20)30088-8. |
[5] | Yang Q , Huo J , Li J , Jiang YS . Research on the influence of the COVID-19 epidemic on work stress of returning workers in China: A study based on empirical analyses of industrial enterprises. Work. (2020) ;67: (1):67–79. doi: 10.3233/WOR-203253. |
[6] | Wang C , Horby PW , Hayden FG , Gao GF . A novel coronavirus outbreak of global health concern. Lancet. (2020) ;395: :470–3. doi: 10.1016/S0140-6736(20)30185-9. |
[7] | Lai JB , Ma SM , Wang Y , Cai ZX , Hu JB , Wei N , et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) ;3(3). doi: 10.1001/jamanetworkopen.2020.3976. |
[8] | González-Sanguino C , Ausín B , Castellanos M , Saiz J , López-Gómez A , Ugidos C , et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) . doi: 10.1016/j.bbi.2020.05.040.S0889-1591(20)30812-6. |
[9] | Nachimuthu S , Vijayalakshmi R , Sudha M , Viswanathan V . Coping with diabetes during the COVID – 19 lockdown in India: Results of an online pilot survey. Diabetes Metab Syndr. (2020) ;14: (4):579–82. doi: 10.1016/j.dsx.2020.04.053. |
[10] | Zhang WR , Wang K , Yin L , Zhao WF , Xue Q , Peng M , et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) ;89: (4):242–50. doi: 10.1159/000507639. |
[11] | Kang BA , Kwon S , You M , Lee H . Perceived sources of occupational burn-out and embitterment among front-line health workers for COVID-19 control in Gyeonggi province, South Korea: A qualitative study. Occup Environ Med. (2022) ;79: (4):245–52. doi: 10.1136/oemed-2021-107635. |
[12] | Panagioti M , Geraghty K , Johnson J . How to prevent burnout in cardiologists? A review of the current evidence, gaps, and future directions. Trends Cardiovasc Med. (2018) ;28: (1):1–7. doi: 10.1016/j.tcm.2017.06.018. |
[13] | Low ZX , Yeo KA , Sharma VK , Leung GK , McIntyre RS , Guerrero A , et al. Prevalence of burnout in medical and surgical residents: A meta-analysis. Int J Environ Res Public Health. (2019) ;16: (9):1479. doi: 10.3390/ijerph16091479. |
[14] | Özgün Ü . During COVID-19, which is more effective in work accident prevention behavior of healthcare professionals: Safety awareness or fatalism perception? Work. (2020) ;67: (4):783–90. doi: 10.3233/WOR-203327. |
[15] | Woo T , Ho R , Tang A , Tam W . Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J Psychiatr Res. (2020) ;123: :9–20. doi: 10.1016/j.jpsychires.2019;12.015. |
[16] | Jugovac S , O’Kearney R , Hawes DJ , Pasalich DS . Attachment- and emotion-focused parenting interventions for child and adolescent externalizing and internalizing behaviors: A meta-analysis. Clin Child Fam Psychol Rev. (2022) ;10. doi: 10.1007/s10567-022-00401-8. |
[17] | Ignatyev Y , Fritsch R , Priebe S , Mundt AP . Psychometric properties of the symptom check-list-90-R in prison inmates. Psychiatry Res. (2016) ;239: :226–31. doi: 10.1016/j.psychres.2016.03.007. |
[18] | Albert U , Bonavigo T , Moro O , De Caro EF , Palmisano S , Pascolo-Fabrici E , et al. SCL-90 empirical factors predict post-surgery weight loss in bariatric patients over longer time periods. Eat Weight Disord. (2022) ;27: (7):2845–55. doi: 10.1007/s40519-022-01424-4. |
[19] | Bisby MA , Karin E , Scott AJ , Dudeney J , Fisher A , Gandy M , et al. Examining the psychometric properties of brief screening measures of depression and anxiety in chronic pain: The Patient Health Questionnaire 2-item and Generalized Anxiety Disorder 2-item. Pain Pract.. (2022) ;22: (4):478–86. doi:10.1111/papr.13107. |
[20] | Fusar-Poli P , Salazar de Pablo G , Correll CU , Meyer-Lindenberg A , Millan MJ , Borgwardt S , et al. Prevention of psychosis: Advances in detection, prognosis, and intervention. JAMA Psychiatry. (2020) ;77: (7):755–65. doi: 10.1001/jamapsychiatry.2019.4779. |
[21] | Aasland OG , Olff M , Falkum E , Schweder T , Ursin H . Health complaints and job stress in Norwegian physicians: The use of an overlapping questionnaire design. Soc Sci Med. (1997) ;45: (11):1615–29. doi: 10.1016/s0277-9536(97)00093-2. |
[22] | Høstmælingen A , Ulvenes P , Nissen-Lie HA , Eielsen M , Wampold BE . Trajectories of change in chronic depression: Differences in self-criticism and somatic symptoms between users of antidepressants and nonmedicated patients. J Couns Psychol. (2022) ;69: (1):85–99. doi: 10.1037/cou0000572. |
[23] | Comfort AB , Krezanoski PJ , Rao L , El Ayadi A , Tsai AC , Goodman S , et al. Mental health among outpatient reproductive health care providers during the US COVID-19 epidemic. Reprod Health. (2021) ;18: (1):49. doi: 10.1186/s12978-021-01102-1. |
[24] | Gupta S , Basera D , Purwar S , Poddar L , Rozatkar AR , Kumar M , et al. Comparing the psychological problems among the health care workers across two waves of SARS-CoV-2 (COVID-19) pandemic: An observational study from India. Disaster Med Public Health Prep. (2022) :1-9. doi: 10.1017/dm2022.192. |
[25] | Gu M , Gu Y , Mei YM , Lu JH , Yu RB . Survey on mental health status of medical practitioners in comprehensive hospitals of Jiangsu. Chinese Journal of Public Health. (2008) (08):921–22. |
[26] | Zheng RJ , Zhou YH , Fu Y , Xiang QF , Cheng FY , Chen HQ , et al. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: A cross-sectional study. Int J Nurs Stud. (2021) ;114: :103809. doi: 10.1016/j.ijnurstu.2020.103809. |
[27] | Song XY , Fu WN , Liu XR , Luo ZQ , Wang RX , Zhou N , et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. (2020) ;88: :60–5. doi: 10.1016/j.bbi.2020.06.002. |
[28] | Leng M , Wei LL , Shi XH , Cao GR , Wei YL , Xu H , et al. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs Crit Care. (2021) ;26: (2):94–101. doi: 10.1111/nicc.12528. |
[29] | Sun XX , Xie F , Chen BJ , Shi PX , Shen ST , Chen ZH , et al. Negative emotions in Chinese frontline medical staff during the early stage of the COVID-19 epidemic: Status, trend, and influential pathways based on a national investigation. Front Psychiatry. (2021) ;12: :567446. doi: 10.3389/fpsyt.2021.567446. |
[30] | Le XTH , Nguyen QT , Onyango B , Nguyen QN , Pham QT , Ta NTK , et al. Perception toward exposure risk of COVID-19 among health workers in vietnam: Status and correlated factors. Front Public Health. (2021) ;9: :589317. doi: 10.3389/fpubh.2021.589317. |
[31] | Ho RC , Tran BX , McIntyre RS . The impact of COVID-19 pandemic on global mental health: From the general public to healthcare workers. Ann Acad Med Singap. (2021) ;50: (3):198–9. doi: 10.47102/annals-acadmedsg.202189. |
[32] | Chew NWS , Ngiam JN , Tan BYQ , Tham SM , Tan CYS , Jing M , et al. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. BJPsych Open. (2020) ;6: (6):e116. doi: 10.1192/bjo.2020.98. |
[33] | Tan BYQ , Chew NWS , Lee GKH , Jing MX , Goh YH , Yeo LLL , et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. (2020) ;M20-1083. doi:10.7326/M20-1083. |
[34] | Chew NWS , Cheong C , Kong G , Phua K , Ngiam JN , Tan BYQ , et al. An Asia-Pacific study on healthcare worker’s perception and willingness to receive COVID-19 vaccination. Int J Infect Dis. (2021) :S1201-9712(21)00287-3. doi: 10.1016/j.ijid.2021.03.069. |
[35] | Saragih ID , Tonapa SI , Saragih IS , Advani S , Batubara SK , Suarilah I , et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int J Nurs Stud. (2021) ;121: :104002. doi: 10.1016/j.ijnurstu.2021.104002. |
[36] | Ho CS , Chee CY , Ho RC . Mental health strategies to combat the psychological impact of coronavirus disease (COVID-19) beyond paranoia and panic. Ann Acad Med Singap. (2020) ;49: (3):155–60. |
[37] | Soh HL , Ho RC , Ho CS , Tam WW . Efficacy of digital cognitive behavioural therapy for insomnia: A meta-analysis of randomised controlled trials. Sleep Med. (2020) ;75: :315–25. doi: 10.1016/j.slee2020.08.020. |



