Diabetes and COVID-19: Case study
Fadi F. Fawares*, Rabia Haddad and Bayan Fawares
Department of Nursing, Nurse Educator at King Hussein Cancer Center, Jordan
Department of Nursing, King Abdullah University Hospital/Jordan University of science and technology, Jordan
Department of Nursing, Registered Nurse, Gynecology and Paediatrics Hospital, Ministry of health, Jordan
Received Date: 29/05/2021; Published Date: 16/06/2021
*Corresponding author: Fadi F Fawaris, Department of Nursing, Clinical Nurse Educator at King Hussein Cancer Center, Amman, Jordan. Tel: 00962780373897; E-Mail: Fadi862005@yahoo.com,
ORCID ID: https://orcid.org/0000- 0001-8461-3733
Abstract
Respiratory distress is commonly seen with COVID-19. But in many cases, the virus affects a person’s overall well-being and aggravates other systemic diseases. One such observation of grave concern is a rapid increase in the number of mucormycosis cases in patients recovering from COVID-19. This manuscript discusses a few hypotheses that may explain the pathogenesis of mucormycosis in post COVID-19 phase.
Keywords: COVID-19; Invasive fungal infections; Mucormycosis; Mucormycetes; Mycoses; SARS-CoV-2
Introduction
Coronavirus disease-2019 (COVID-19) is an emerging human disease caused by the novel coronavirus (SARS-CoV-2), which was reported first in December 2019. Due to the rapid spread worldwide, the World Health Organization (WHO) affirmed the COVID-19 a public health emergency in January 2020 (Shah and Farrow, 2020) [1]. By the end of September 2020, over 32.7 million COVID-19 cases and 991 000 deaths have been informed to WHO COVID-19 (World Health Organization (WHO), 2020) [2].
In Jordan, the infected individuals with COVID-19 were isolated and treated in specialized units. By the end of January, 2021 the Jordanian Ministry of Health announced 326,855 confirmed cases; and 4,316 deaths (Ministry of Health, 2020). The Jordanian government-imposed home confinement instructions, lockdown, and movement restrictions followed by a partial lockdown until further notice. The studies emphasized the importance of religious/spiritual involvements in order to deliver a vital and whole care for all (fawares et al., 2020) [3].
Diabetes was found to be 8.2 percent in 1590 patients from China with COVID-19. Nevertheless, the incidence of diabetes was elevated to 34.6% in patients who complained from sever COVID-19 symptoms (Guan et al., 2020) [4]. Newly, study of COVID-19 patients, showed that the frequency of diabetes and obesity was greater in those who admitted than in those not admitted to the hospital (347 percent vs 97% for diabetes and 395 percent vs 308 percent for obesity, correspondingly).
DKA is life-threatening diabetic crises that should be avoided. Any infectious disease, like COVID-19, may cause these complications. In this report, I discuss case of vital COVID-19 that was handled in the ministry of health setting and complicated by DKA (Suwanwongse et al., 2021) [5].
Case Presentation
A 46-year-old male patient came to the ER complaining from fever for 11 days with general weakness, myalgia, hyposmia, and one incidence of vomiting.
Furthermore, the patient complained of polydipsia, polyuria, and nocturia for 6 days with generalized weakness, and dyspnea for 5 days. With history of Hypertension and Diabetes mellitus controlled without medications. He was controlling his blood glucose levels with dietary and exercises.
The patient was dehydrated on the initial evaluation, and the physical assessment was as the following:
- HR:118 beats per minute,
- Blood pressure :136/92 mmHg,
- temperature of 37.8 °C,
- respiratory rate of 25 breaths per minute,
- And oxygen saturation of 90 percent in room air.
Blood samples were taken and displayed the following:
- Plasma blood glucose of 1543 mg/dl, serum creatinine 3.2 mg/dl, serum potassium 5.5 mEq/L HbA1c 14.0%, mg/dl, serum sodium 149 mEq/L, blood urea 132 and urine analysis showed positive result of ketones. The arterial blood gas sample (ABG) shown compensated metabolic acidosis. Chest x-ray showed bilateral airspace consolidations, more prominent in the bilateral middle and lower lungs, concerning for multifocal infection. He was admitted and treated in the ICU as a part of COVID-19 treatment guideline. COVID-19 tested positive on the same day of admission.
Based on the current treatment protocol, initial antibiotic regimen started, oxygen supplementation through nasal cannula 3L/M, and DKA treatment plan was started generally with careful administration of fluids, potassium correction and insulin.
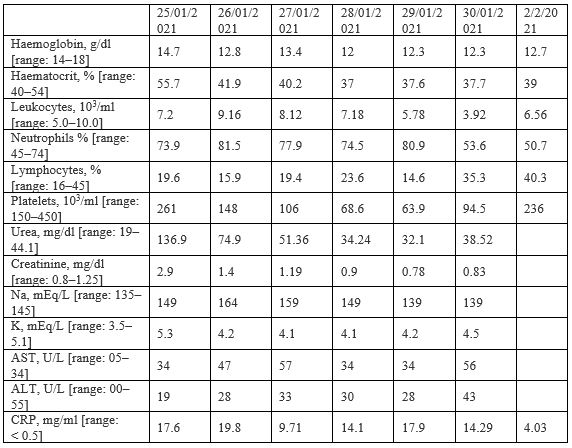
The patient’s DKA and Acute Kidney Injury (AKI) enhanced progressively which was obvious by the stabilisation of renal function and serum sodium levels. He also developing thrombocytopenia throughout the sequence of management which improved over seven days. The patient also displayed enhancement in his breathing pattern as his oxygen saturation raised to 96% at room air. Repeated chest x-ray shown obvious improvement of the lung consolidations. After seven days from the admission day, the patient was transferred out of ICU to the general ward in stable condition.
Discussion
I have presented case of diabetic emergencies caused by COVID-19, in which a patient was hospitalized with DKA accompanied by pneumonia and recovered suitably. To the best of my knowledge, this is the first time a case report of COVID-19 with DKA has been discussed.
The COVID-19 has been linked to increased severity with increasing age and male sex (Caramelo et al., 2020) [6]. According to study was conducted in China, the overall case-fatality rate was 2.3 percent, but it rose to 14.8 percent in people aged 80 and above. Diabetes prevalence rises with age, hence diabetic COVID-19 patients are older on average than non-diabetic COVID-19 patients. Another review of COVID-19 patients with and without diabetes found that survivors were younger than non-survivors, and that being above the age of 70 was an independent risk factor for in-hospital mortality [7-10].
References
- Shah, S. G. S., & Farrow, A. A commentary on “World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19)”. International journal of surgery (London, England), 2020; 76: 128.
- World Health Organization. Timeline: WHO’s COVID-19 response. World Health Organization. 2020.
- Fawares F, Ibdah R, Ammar K, Alkhoulli L, Khader H, Muhareb H, et al. Spiritual Beliefs of Jordanian Adult Patients Receiving Palliative Care. Journal of religion and health, 2020; 1-13.
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. European Respiratory Journal, 2020; 55(5).
- Suwanwongse K, Shabarek N. Newly diagnosed diabetes mellitus, DKA, and COVID‐19: Causality or coincidence? A report of three cases. Journal of medical virology, 2021; 93(2): 1150-1153.
- Caramelo F, Ferreira N, Oliveiros B. Estimation of risk factors for COVID-19 mortality-preliminary results. MedRxiv. 2020.
- Gupta R, Misra A. Clinical considerations in patients with diabetes during times of COVID19: An update on lifestyle factors and antihyperglycemic drugs with focus on India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 2020; 14(6), 1777-1781.
- WHO. Timeline: WHO’s COVID-19 response. World Health Organization. (2021a).
- Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. Bmj, 2020; 369.
- Soliman A, Nair AP, Al Masalamani MS, De Sanctis V, Khattab MAA, Alsaud AE, et al. Prevalence, clinical manifestations, and biochemical data of type 2 diabetes mellitus versus nondiabetic symptomatic patients with COVID-19: A comparative study. Acta Bio Medica: Atenei Parmensis, 2020; 91(3): e2020010.

