The red half-moon nail sign in a COVID-19 patient
Esranur Ünal, Seray Külcü Çakmak , Ahu Yorulmaz
, Ahu Yorulmaz
University of Health Sciences, Department of Dermatology, Ankara City Hospital, Ankara, Turkey
Corresponding author: Seray Külcü Çakmak, MD
How to cite this article: Ünal E, Çakmak SK, Yorulmaz A. The red half-moon nail sign in a COVID-19 patient. Our Dermatol Online. 2022;13(2):223-224.
Submission: 25.10.2021; Acceptance: 05.01.2021
DOI: 10.7241/ourd.20222.29
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a global pandemic. Several cutaneous manifestations associated with COVID-19 have been reported, including chilblains or chilblain-like lesions, erythematous rash, viral exanthem, urticaria, livedo reticularis, acral ischemia, palpable purpura, and erythema multiforme. These were thought to be useful in the early diagnosis and triage of COVID-19 patients and their risk stratification [1]. However, there are limited reports on the nail manifestations of COVID-19, including several cases of Beau lines, leukonychia, orange discoloration, and onychomadesis [2]. An exceptionally rarely reported manifestation of COVID-19 is the red half-moon-nail sign [3,4].
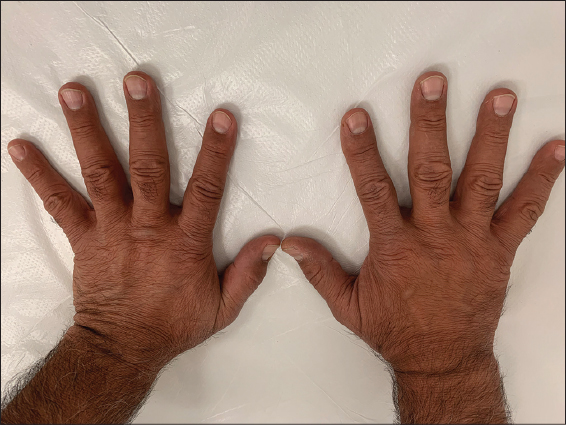
A 46-year-old male presented to our outpatient clinic with transversal red bands surrounding the distal margin of the nail’s lunula on all of the fingernails, which the patient noticed a week previously (Fig. 1). One month before, with symptoms of fever, shortness of breath, and coughing present for three days, he had been given the diagnosis of COVID-19 following a positive nasopharyngeal swab polymerase chain reaction test. Computed tomography of the lungs revealed generalized ground-glass opacities and paraseptal emphysema in the upper lobes, and the patient was hospitalized for one week and treated with favipiravir for five days and was on oxygen therapy. He was discharged from the hospital one week later with partial remission of the respiratory symptoms. He also had hypertension, atherosclerotic heart disease, and Behçet’s disease, and had been using metoprolol, amlodipine, edoxaban, irbesartan, hydrochlorothiazide, and colchicine. After two weeks of follow-up, the bands remained present and became wider (Fig. 2).
The red-half-moon sign was first described by Neri et al. as half-moon-shaped transversal red bands after SARS-CoV-2 infection. The patient was a sixty-year-old female and the bands appeared two weeks after the onset of symptoms of COVID-19. The patient was hospitalized and received oxygen therapy and several other treatments, including hydroxychloroquine and lopinavir/ritonavir. As in our patient, the bands remained present and became wider after one month of follow-up [3].
Mendez-Flores et al. reported a case of the red half-moon nail sign in a 37-year-old female with COVID-19. The patient noticed the changes two days after the COVID-19 symptoms appeared, and these lasted for one week before gradually returning to normal. The patient was managed at home and required no oxygen therapy [4].
The pathogenesis of the red half-moon sign is unknown. Neri et al. proposed that localized microvascular injury secondary to an inflammatory immune response and procoagulant state may play a role. It is thought that, because of the location, the distal subungual arcade’s capillary network may be affected in these cases [2,3].
We also agree that the red half-moon sign could be associated with microvascular injury or a procoagulant state connected to an inflammatory immune response. Recently, Natalello et al. reported nailfold capillaroscopy abnormalities in COVID-19 patients, including microvascular alterations in the nailfold capillary bed ranging from microthrombosis to altered capillary structures, according to the COVID-19 phase supporting this theory [5]. We also think that the persistence of the bands might be related to the severity of the disease, as both our and Neri et al.’s patients were hospitalized and had a more severe disease course than Mendez-Florez et al.’s patient.
We think that, similarly to skin findings, nail findings may be a clue in the diagnosis and prognosis of COVID-19 as well as the pathogenesis of the disease, and clinicians should search for nail findings in COVID-19 patients.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Mirza FN, Malik AA, Omer SB, Sethi A. Dermatologic manifestations of COVID-19:a comprehensive systematic review. Int J Dermatol. 2021;60:418-50.
2. Ocampo-Garza SS, Ocampo-Candiani J, Camela E, Vastarella M, Fabbrocini G, Scalvenzi M, et al. Nail changes as manifestation of systemic disease in COVID-19 infection. J Eur Acad Dermatol Venereol. 2021;35:e474-5.
3. Neri I, Guglielmo A, Virdi A, Gaspari V, Starace M, Piraccini BM. The red half-moon nail sign:A novel manifestation of coronavirus infection. J Eur Acad Dermatol Venereol. 2020;34:e663-5.
4. Méndez-Flores S, Zaladonis A, Valdes-Rodriguez R. COVID-19 and nail manifestation:Be on the lookout for the red half-moon nail sign. Int J Dermatol. 2020;59:1414.
5. Natalello G, De Luca G, Gigante L, Campochiaro C, De Lorenzis E, Verardi L, et al. Nailfold capillaroscopy findings in patients with coronavirus disease 2019:Broadening the spectrum of COVID-19 microvascular involvement. Microvasc Res. 2021;133:104071.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-8536-5946 http://orcid.org/0000-0001-8536-5946 http://orcid.org/0000-0003-4687-0522 http://orcid.org/0000-0003-4687-0522 |




Comments are closed.