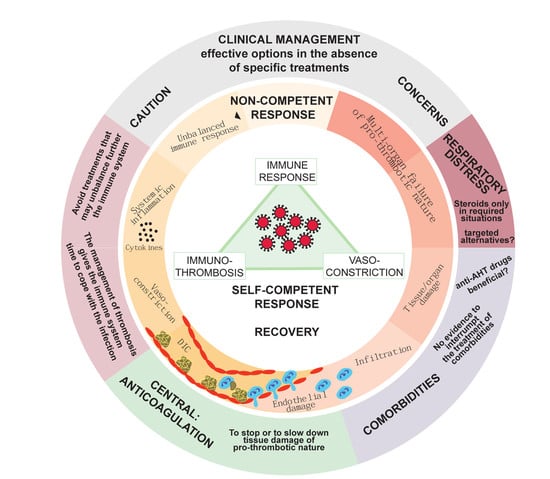
Clinical Management of Hypertension, Inflammation and Thrombosis in Hospitalized COVID-19 Patients: Impact on Survival and Concerns
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Data Sources
2.2. Variables
2.3. Study Design
- AHT: patients included were treated or not treated with ACE2-Is (enalapril or captopril), ARBs (valsartan) or combinations of both ACE2-Is and ARBs. Separate analyses were performed for each one of these subgroups, and they were grouped for all patients receiving ACE2-Is or ARBs;
- Inflammation (NSAIDs): patients included were treated or not treated with NSAIDs. Patients treated with immunosuppressing drugs or corticosteroids were excluded;
- Inflammation (corticosteroids): patients included were treated or not treated with corticosteroids. Patients treated with other immunosuppressing drugs (interferon beta-1b, ciclosporin, mycophenolic acid and azathioprine) or NSAIDs were excluded;
- Hemostasis: patients included were treated or not treated with low molecular weight heparin (LMWH). Patients treated with other anticoagulants (vitamin K antagonists and direct oral anticoagulants) or anti-platelet drugs (clopidogrel, acetylsalicylic acid, triflusal, prasugrel and ticagrelor) were excluded, as they were represented in low numbers and precluded a rigorous statistical analysis. Patients receiving different doses of LMWH during their hospitalization were included in the group of the highest administered dose.
2.4. Statistical Analysis
3. Results and Discussion
3.1. Arterial Hypertension
3.2. Inflammation: NSAIDs
3.3. Inflammation: Corticosteroids
3.4. Hemostasis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO World Health Organization. Coronavirus Disease (Covid-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 18 October 2020).
- Joly, B.S.; Siguret, V.; Veyradier, A. Understanding pathophysiology of hemostasis disorders in critically ill patients with COVID-19. Intensive Care Med. 2020, 46, 1603–1606. [Google Scholar] [CrossRef]
- Ni, W.; Yang, X.; Yang, D.; Bao, J.; Li, R.; Xiao, Y.; Hou, C.; Wang, H.; Liu, J.; Yang, D.; et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care 2020, 24, 422. [Google Scholar] [CrossRef] [PubMed]
- Debes, J.D. COVID-19 and the liver: The perils of non-peer-reviewed science in times of a pandemic. Gastroenterology 2020, 159, 1620. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, I.I.; Watts, A.; Thomas-Bachli, A.; Huber, C.; Kraemer, M.U.G.; Khan, K. Pneumonia of unknown aetiology in Wuhan, China: Potential for international spread via commercial air travel. J. Travel Med. 2020, 27, taaa008. [Google Scholar] [CrossRef] [PubMed]
- Bellocchio, L.; Bordea, I.R.; Ballini, A.; Lorusso, F.; Hazballa, D.; Isacco, C.G.; Malcangi, G.; Inchingolo, A.D.; DiPalma, G.; Inchingolo, F.; et al. Environmental Issues and Neurological Manifestations Associated with COVID-19 Pandemic: New Aspects of the Disease? Int. J. Environ. Res. Public Health 2020, 17, 8049. [Google Scholar] [CrossRef]
- Pillai, P.; Joseph, J.P.; Fadzillah, N.H.M.; Mahmod, M. COVID-19 and Major Organ Thromboembolism: Manifestations in Neurovascular and Cardiovascular Systems. J. Stroke Cerebrovasc. Dis. 2021, 30, 105427. [Google Scholar] [CrossRef] [PubMed]
- Słomka, A.; Kowalewski, M.; Żekanowska, E. Coronavirus Disease 2019 (COVID–19): A Short Review on Hematological Manifestations. Pathogens 2020, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Bikdeli, B.; Madhavan, M.V.; Jimenez, D.; Chuich, T.; Dreyfus, I.; Driggin, E.; Der Nigoghossian, C.; Ageno, W.; Madjid, M.; Guo, Y.; et al. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020, 75, 2950–2973. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Misra, A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infection with reference to use of therapeutic and other drugs used in Co-morbid diseases (Hypertension, diabetes etc). Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 251–254. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Fagot Gandet, F.; et al. High risk of thrombosis in patients with severe sars-cov-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Llitjos, J.; Leclerc, M.; Chochois, C.; Monsallier, J.; Ramakers, M.; Auvray, M.; Merouani, K. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J. Thromb. Haemost. 2020, 18, 1743–1746. [Google Scholar] [CrossRef] [PubMed]
- Lodigiani, C.; Iapichino, G.; Carenzo, L.; Cecconi, M.; Ferrazzi, P.; Sebastian, T.; Kucher, N.; Studt, J.-D.; Sacco, C.; Bertuzzi, A.; et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan, S.; Yi, Q.; Fan, S.; Lv, J.; Zhang, X.; Guo, L.; Lang, C.; Xiao, Q.; Xiao, K.; Yi, Z.; et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID-19) infected patients. Br. J. Haematol. 2020, 189, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Fosbøl, E.L.; Butt, J.H.; Østergaard, L.; Andersson, C.; Selmer, C.; Kragholm, K.; Schou, M.; Phelps, M.; Gislason, G.H.; Gerds, T.A.; et al. Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality. JAMA 2020, 324, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Vikse, J.; Benoit, S.; Favaloro, E.J.; Lippi, G. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: A novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin. Chim. Acta 2020, 507, 167–173. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Kai, H.; Kai, M. Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors—lessons from available evidence and insights into COVID-19. Hypertens. Res. 2020, 43, 648–654. [Google Scholar] [CrossRef]
- Mancia, G.; Rea, F.; Ludergnani, M.; Apolone, G.; Corrao, G. Renin–Angiotensin–Aldosterone System Blockers and the Risk of Covid-19. N. Engl. J. Med. 2020, 382, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Rico-Mesa, J.S.; White, A.; Anderson, A.S. Outcomes in Patients with COVID-19 Infection Taking ACEI/ARB. Curr. Cardiol. Rep. 2020, 22, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shyh, G.I.; Nawarskas, J.J.; Cheng-Lai, A. Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Patients with Coronavirus Disease 2019: Friend or Foe? Cardiol. Rev. 2020, 28, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Varughese, G.I.; Lip, G.Y.H. Is hypertension a prothrombotic state? Curr. Hypertens. Rep. 2005, 7, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Galimberti, F.; McBride, J.; Cronin, M.; Li, Y.; Fox, J.; Abrouk, M.; Herbst, A.; Kirsner, R.S. Evidence-based best practice advice for patients treated with systemic immunosuppressants in relation to COVID-19. Clin. Dermatol. 2020, 38, 775–780. [Google Scholar] [CrossRef]
- Ye, Q.; Wang, B.; Mao, J. The pathogenesis and treatment of the ’cytokine storm’ in COVID-19. J. Infect. 2020, 80, 607–613. [Google Scholar] [CrossRef]
- Jamilloux, Y.; Henry, T.; Belot, A.; Viel, S.; Fauter, M.; El Jammal, T.; Walzer, T.; François, B.; Sève, P. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun. Rev. 2020, 19, 102567. [Google Scholar] [CrossRef] [PubMed]
- Russell, B.; Moss, C.; Rigg, A.; Van Hemelrijck, M. COVID-19 and treatment with NSAIDs and corticosteroids: Should we be limiting their use in the clinical setting? Ecancermedicalscience 2020, 14, 1023. [Google Scholar] [CrossRef] [Green Version]
- Jamerson, B.D.; Haryadi, T.H. The use of ibuprofen to treat fever in COVID-19: A possible indirect association with worse outcome? Med. Hypotheses 2020, 144, 109880. [Google Scholar] [CrossRef] [PubMed]
- Martins-Filho, P.R.; Nascimento-Júnior, E.M.D.; Santos, V.S. No current evidence supporting risk of using Ibuprofen in patients with COVID-19. Int. J. Clin. Pract. 2020, 74, e13576. [Google Scholar] [CrossRef]
- Sodhi, M.; Etminan, M. Safety of Ibuprofen in Patients with COVID-19. Chest 2020, 158, 55–56. [Google Scholar] [CrossRef] [PubMed]
- Zolk, O.; Hafner, S.; Schmidt, C.Q.; on behalf of the German Society for Experimental and Clinical Pharmacology and Toxicology. COVID-19 pandemic and therapy with ibuprofen or renin-angiotensin system blockers: No need for interruptions or changes in ongoing chronic treatments. Naunyn Schmiedebergs Arch. Pharmacol. 2020, 393, 1131–1135. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in hospitalized patients with COVID-19. N. Engl. J. Med. 2020, 384, 693–704. [Google Scholar]
- McGee, S.; Hirschmann, J. Use of corticosteroids in treating infectious diseases. Arch. Intern. Med. 2008, 168, 1034–1046. [Google Scholar] [CrossRef]
- Yang, J.-W.; Fan, L.-C.; Miao, X.-Y.; Mao, B.; Li, M.-H.; Lu, H.-W.; Liang, S.; Xu, J.-F. Corticosteroids for the treatment of human infection with influenza virus: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2015, 21, 956–963. [Google Scholar] [CrossRef] [Green Version]
- Saghazadeh, A.; Rezaei, N. Towards treatment planning of COVID-19: Rationale and hypothesis for the use of multiple immunosuppressive agents: Anti-antibodies, immunoglobulins, and corticosteroids. Int. Immunopharmacol. 2020, 84, 106560. [Google Scholar] [CrossRef] [PubMed]
- Kakodkar, P.; Kaka, N.; Baig, M.N. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus Cureus 2020, 12, e7560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, R.; Wang, L.; Kuo, H.-C.D.; Shannar, A.; Peter, R.; Chou, P.J.; Li, S.; Hudlikar, R.; Liu, X.; Liu, Z.; et al. An update on current therapeutic drugs treating COVID-19. Curr. Pharmacol. Rep. 2020, 1–15, Online ahead of print. Available online: https://www.ncbi.nlm.nih.gov/pubmed/32395418 (accessed on 18 October 2020). [CrossRef] [PubMed]
- R Core Team. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2020. Available online: https://R-project.org/ (accessed on 10 February 2021).
- Rossi, L.; Malagoli, A.; Biagi, A.; Zanni, A.; Sticozzi, C.; Comastri, G.; Pannone, L.; Gandolfi, S.; Vergara, P.; Villani, G.Q. Renin-angiotensin system inhibitors and mortality in patients with COVID-19. Infection 2020, 1–8, Online ahead of print. Available online: https://www.ncbi.nlm.nih.gov/pubmed/33222020 (accessed on 18 December 2020). [CrossRef]
- Tetlow, S.; Segiet-Swiecicka, A.; O’Sullivan, R.; O’Halloran, S.; Kalb, K.; Brathwaite-Shirley, C.; Alger, L.; Ankuli, A.; Baig, M.S.; Catmur, F.; et al. ACE inhibitors, angiotensin receptor blockers and endothelial injury in COVID-19. J. Intern. Med. 2020. Online ahead of print. Available online: https://www.ncbi.nlm.nih.gov/pubmed/33210357 (accessed on 18 December 2020). [CrossRef] [PubMed]
- Zhang, Y.; Coats, A.J.S.; Zheng, Z.; Adamo, M.; Ambrosio, G.; Anker, S.D.; Butler, J.; Xu, D.; Mao, J.; Khan, M.S.; et al. Management of heart failure patients with COVID-19: A joint position paper of the chinese heart failure association & national heart failure committee and the heart failure association of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22, 941–956. [Google Scholar] [PubMed]
- Chandan, J.S.; Zemedikun, D.T.; Thayakaran, R.; Byne, N.; Dhalla, S.; Acosta-Mena, D.; Gokhale, K.M.; Thomas, T.; Sainsbury, C.; Subramanian, A.; et al. Non-steroidal anti-inflammatory drugs and susceptibility to COVID-19. Arthritis Rheumatol. 2020. Online ahead of print. Available online: https://www.ncbi.nlm.nih.gov/pubmed/33185016 (accessed on 18 December 2020). [CrossRef]
- Kelleni, M.T. Early use of non-steroidal anti-inflammatory drugs in COVID-19 might reverse pathogenesis, prevent complications and improve clinical outcomes. Biomed. Pharmacother. 2021, 133, 110982. [Google Scholar] [CrossRef]
- Lund, L.C.; Kristensen, K.B.; Reilev, M.; Christensen, S.; Thomsen, R.W.; Christiansen, C.F.; Støvring, H.; Johansen, N.B.; Brun, N.C.; Hallas, J.; et al. Adverse outcomes and mortality in users of non-steroidal anti-inflammatory drugs who tested positive for SARS-CoV-2: A Danish nationwide cohort study. PLoS Med. 2020, 17, e1003308. [Google Scholar] [CrossRef]
- Ahmed, M.H.; Hassan, A. Dexamethasone for the treatment of coronavirus disease (COVID-19): A review. SN Compr. Clin. Med. 2020, 1–10, Online ahead of print. Available online: https://www.ncbi.nlm.nih.gov/pubmed/33163859 (accessed on 18 October 2020). [CrossRef]
- Matthay, M.A.; Thompson, B.T. Dexamethasone in hospitalised patients with COVID-19: Addressing uncertainties. Lancet Respir. Med. 2020, 8, 1170–1172. [Google Scholar] [CrossRef]
- Liberman, A.C.; Budziñski, M.L.; Sokn, C.; Gobbini, R.P.; Steininger, A.; Arzt, E. Regulatory and mechanistic actions of glucocorticoids on T and inflammatory cells. Front. Endocrinol. 2018, 9, 235. [Google Scholar] [CrossRef]
- Ronchetti, S.; Migliorati, G.; Bruscoli, S.; Riccardi, C. Defining the role of glucocorticoids in inflammation. Clin. Sci. 2018, 132, 1529–1543. [Google Scholar] [CrossRef] [PubMed]
- Kow, C.S.; Hasan, S.S. Use of low-molecular-weight heparin in COVID-19 patients. J. Vasc. Surg. Venous Lymphat. Disord. 2020, 8, 900–901. [Google Scholar] [CrossRef]
- Barnes, G.D.; Burnett, A.; Allen, A.; Blumenstein, M.; Clark, N.P.; Cuker, A.; Dager, W.E.; Deitelzweig, S.B.; Ellsworth, S.; Garcia, D.; et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: Interim clinical guidance from the anticoagulation forum. J. Thromb. Thrombolysis 2020, 50, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Connors, J.M.; Levy, J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020, 135, 2033–2040. [Google Scholar] [CrossRef]
- Obi, A.T.; Barnes, G.D.; Wakefield, T.W.; Brown, S.; Eliason, J.L.; Arndt, E.; Henke, P.K. Practical diagnosis and treatment of suspected venous thromboembolism during COVID-19 pandemic. J. Vasc. Surg. Venous Lymphat. Disord. 2020, 8, 526–534. [Google Scholar] [CrossRef]
- Tang, N.; Bai, H.; Xiong, D.; Sun, Z. Specific coagulation markers may provide more therapeutic targets in COVID-19 patients receiving prophylactic anticoagulant. J. Thromb. Haemost. 2020, 18, 2428–2430. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, D.; Van Gerwen, M.; Alsen, M.; Thibaud, S.; Kessler, A.J.; Venugopal, S.; Makki, I.; Qin, Q.; Dharmapuri, S.; Jun, T.; et al. Impact of anticoagulation prior to COVID-19 infection: A propensity score–matched cohort study. Blood 2020, 136, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Kelleni, M.T. ACEIs, ARBs, ibuprofen originally linked to COVID-19: The other side of the mirror. Inflammopharmacology 2020, 28, 1477–1480. [Google Scholar] [CrossRef] [PubMed]
- LaForge, M.; Elbim, C.; Frère, C.; Hémadi, M.; Massaad, C.; Nuss, P.; Benoliel, J.-J.; Becker, C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat. Rev. Immunol. 2020, 20, 515–516. [Google Scholar] [CrossRef]
- Sahebnasagh, A.; Saghafi, F.; Safdari, M.; Khataminia, M.; Sadremomtaz, A.; Talaei, Z.; Ghaleno, H.R.; Bagheri, M.; Habtemariam, S.; Avan, R. Neutrophil elastase inhibitor (sivelestat) may be a promising therapeutic option for management of acute lung injury/acute respiratory distress syndrome or disseminated intravascular coagulation in COVID-19. J. Clin. Pharm. Ther. 2020, 45, 1515–1519. [Google Scholar] [CrossRef]
- Maes, B.; Bosteels, C.; De Leeuw, E.; Declercq, J.; Van Damme, K.; Delporte, A.; Demeyere, B.; Vermeersch, S.; Vuylsteke, M.; Willaert, J.; et al. Treatment of severely ill COVID-19 patients with anti-interleukin drugs (COV-AID): A structured summary of a study protocol for a randomised controlled trial. Trials 2020, 21, 468. [Google Scholar] [CrossRef] [PubMed]
- Ayerbe, L.; Risco, C.; Ayis, S. The association between treatment with heparin and survival in patients with COVID-19. J. Thromb. Thrombolysis 2020, 50, 298–301. [Google Scholar] [CrossRef]
- Patell, R.; Chiasakul, T.; Bauer, E.; Zwicker, J.I. Pharmacologic Thromboprophylaxis and Thrombosis in Hospitalized Patients with COVID-19: A Pooled Analysis. Thromb. Haemost. 2021, 121, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Cuker, A.; Tseng, E.K.; Nieuwlaat, R.; Angchaisuksiri, P.; Blair, C.; Dane, K.; Davila, J.; DeSancho, M.T.; Diuguid, D.; Griffin, D.O.; et al. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19. Blood Adv. 2021, 5, 872–888. [Google Scholar] [CrossRef]
- Patell, R.; Bogue, T.; Koshy, A.; Bindal, P.; Merrill, M.; Aird, W.C.; Bauer, K.A.; Zwicker, J.I. Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood 2020, 136, 1342–1346. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.N.; Whyte, M.B.; Georgiou, L.; Giron, G.; Czuprynska, J.; Rea, C.; Vadher, B.; Patel, R.K.; Gee, E.; Arya, R. Postdischarge venous thromboembolism following hospital admission with COVID-19. Blood 2020, 136, 1347–1350. [Google Scholar] [CrossRef] [PubMed]
- Mycroft-West, C.J.; Su, D.; Pagani, I.; Rudd, T.R.; Elli, S.; Gandhi, N.S.; Guimond, S.E.; Miller, G.J.; Meneghetti, M.C.Z.; Nader, H.B.; et al. Heparin Inhibits Cellular Invasion by SARS-CoV-2: Structural Dependence of the Interaction of the Spike S1 Receptor-Binding Domain with Heparin. Thromb. Haemost. 2020, 120, 1700–1715. [Google Scholar] [PubMed]
- Tree, J.A.; Turnbull, J.E.; Buttigieg, K.R.; Elmore, M.J.; Coombes, N.; Hogwood, J.; Mycroft-West, C.J.; Lima, M.A.; Skidmore, M.A.; Karlsson, R.; et al. Unfractionated heparin inhibits live wild type SARS-CoV-2 cell infectivity at therapeutically relevant concentrations. Br. J. Pharmacol. 2021, 178, 626–635. [Google Scholar] [CrossRef] [PubMed]




| Severe Respiratory Distress (N) | Non-Treated with Corticosteroids 394 (50%) | Treated with Corticosteroids 399 (50%) | Total 793 (100%) |
| Age | |||
| (Mean ± SD) | 67.0 ± 16.1 | 69.8 ± 14.8 | 68.4 ± 15.5 |
| Sex | |||
| Female | 170 (43%) | 138 (35%) | 308 (39%) |
| Male | 224 (57%) | 261 (65%) | 485 (61%) |
| Status | |||
| Discharge | 334 (85%) | 288 (72%) | 622 (78%) |
| Exitus | 60 (15%) | 111 (28%) | 171 (22%) |
| Hospitalization | |||
| Non-ICU | 374 (95%) | 349 (87%) | 723 (91%) |
| ICU | 20 (5%) | 50 (13%) | 70 (9%) |
| No Registered Respiratory Distress (N) | Non-Treated with Corticosteroids 696 (56%) | Treated with Corticosteroids 546 (44%) | Total 1242 (100%) |
| Age | |||
| (Mean ± SD) | 64.2 ± 17.4 | 68.9 ± 14.7 | 66.3 ± 16.4 |
| Sex | |||
| Female | 293 (42%) | 212 (39%) | 505 (41%) |
| Male | 403 (58%) | 334 (61%) | 737 (59%) |
| Status | |||
| Discharge | 643 (92%) | 437 (80%) | 1080 (87%) |
| Exitus | 53 (8%) | 109 (20%) | 162 (13%) |
| Hospitalization | |||
| Non-ICU | 679 (98%) | 494 (90%) | 1173 (94%) |
| ICU | 17 (2%) | 52 (10%) | 69 (6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Botía, P.; Bernardo, Á.; Acebes-Huerta, A.; Caro, A.; Leoz, B.; Martínez-Carballeira, D.; Palomo-Antequera, C.; Soto, I.; Gutiérrez, L. Clinical Management of Hypertension, Inflammation and Thrombosis in Hospitalized COVID-19 Patients: Impact on Survival and Concerns. J. Clin. Med. 2021, 10, 1073. https://doi.org/10.3390/jcm10051073
Martínez-Botía P, Bernardo Á, Acebes-Huerta A, Caro A, Leoz B, Martínez-Carballeira D, Palomo-Antequera C, Soto I, Gutiérrez L. Clinical Management of Hypertension, Inflammation and Thrombosis in Hospitalized COVID-19 Patients: Impact on Survival and Concerns. Journal of Clinical Medicine. 2021; 10(5):1073. https://doi.org/10.3390/jcm10051073
Chicago/Turabian StyleMartínez-Botía, Patricia, Ángel Bernardo, Andrea Acebes-Huerta, Alberto Caro, Blanca Leoz, Daniel Martínez-Carballeira, Carmen Palomo-Antequera, Inmaculada Soto, and Laura Gutiérrez. 2021. "Clinical Management of Hypertension, Inflammation and Thrombosis in Hospitalized COVID-19 Patients: Impact on Survival and Concerns" Journal of Clinical Medicine 10, no. 5: 1073. https://doi.org/10.3390/jcm10051073