Abstract
Purpose
The COVID-19 pandemic has affected healthcare systems worldwide. Data on the impact on otolaryngological clinics and private practices is sparse. This study aimed to present data on healthcare worker (HCW) screening, status of HCW, pre-interventional testing, the use of personal protective equipment (PPE) and the economic impact of the pandemic.
Methods
Otolaryngological private practices and hospital-based departments were surveyed nationwide using an online questionnaire. Participating facilities were recruited via the German Society for Oto-Rhino-Laryngology and the German Association for Otolaryngologists in Bavaria.
Results
365 private practices (2776 employees) and 65 hospitals (2333 employees) were included. Significantly more hospitals (68.7%) than practices (40.5%) performed pre-interventional testing in their outpatients (p < 0.00). Most inpatients were tested in practices and hospitals (100.0% and 95.0%; p = 0.08). HCW screening was performed in 73.7% of practices and in 77.3% of hospitals (p = 0.54). Significantly more HCW infections were reported in private practices (4.7%) than in hospital (3.6%; p = 0.03). The private or home environment was the most frequent source of infection among HCW in hospitals (44%) and practices (63%). The use of PPE increased over the course of the pandemic. The number of procedures and the revenue decreased in 2020.
Conclusion
The rate of pre-interventional testing among outpatients in otolaryngological practices is low and HCW infections were found to be more frequent in practices than in hospitals. In addition, a high rate of infections in otolaryngological HCW seems to stem from the private or home environment.
Similar content being viewed by others
Background
The first case of the novel coronavirus disease (COVID-19), caused by a beta coronavirus (SARS-CoV-2), was reported in Wuhan, China in December 2019 [1]. The World Health Organization (WHO) declared COVID-19 a global pandemic on 11 March 2020 [2]. The disease shows a death rate of 0.39 to 4%, in most cases caused by respiratory failure and thromboembolic events [3]. To date, a total of more than 2.7 million deaths related to the virus have been registered worldwide [4].
Healthcare workers (HCW) were shown to have an increased risk of infection by SARS-CoV-2 [5]. While guidelines recommend patient screening on SARS-CoV-2 prior to an elective therapeutic intervention [6], regular screening of HCW is not recommended, although it has been shown that 3% of asymptomatic HCW were positive when screened on SARS-CoV-2 [7]. To date, the main sites of infection among HCW are unknown. Additionally, most data on infection of HCW is from the clinical sector, while data from private practices is limited.
HCW who regularly perform aerosol-generating procedures (AGP), are at special risk of an infection with SARS-CoV-2 [8, 9]. In otolaryngology, AGPs are performed frequently. These are surgical procedures such as tracheostomy or CO2 laser ablation, but also diagnostic procedures such as nasopharyngoscopy and laryngoscopy which are performed on a regular daily basis [10,11,12,13]. Therefore, the use of personal protective equipment (PPE) consisting of a mask (FFP2/3), gloves, a gown and goggles is recommended when performing these procedures [14]. Furthermore, guidelines indicate that diagnostic AGPs should only be performed if potential findings may have an impact on patient management [10].
Against the background of a rising number of critically ill patients needing intensive care treatment, national policy demanded the postponement of all elective procedures in Germany in March 2020. In April 2020, the gradual resumption of elective procedures, depending on intensive care capacity, was recommended [15]. The health economic implications of these decisions have not been studied yet.
As a part of the collaborative project “Bundesweites Forschungsnetz Angewandte Surveillance und Testung” (B-FAST) of the Network of University Medicine (NUM), Augsburg University Hospital was commissioned to acquire data on the facial and aerosol-producing areas including otorhinolaryngology (ORL).
This study aims to present data from a nationwide survey of otolaryngological hospital-based departments and private practices regarding the Covid-19 pandemic. Particularly, the use of PPE, pre-interventional testing, healthcare worker screening, healthcare worker status and pandemic-related economic changes at the facilities were examined.
Methods
Based on expert discussion and a review on the current literature a self-report online questionnaire with 64 items was designed (Online Resource 1). In addition to collecting descriptive data, the questionnaire covered the SARS-CoV-2 infection rate among health care workers (HCW), use of personal protective equipment during the pandemic, pre-interventional diagnostics, and pandemic-related economic changes in facilities. Heads of the hospital-based departments were asked to state if their hospital was a primary, secondary or tertiary care department. Private practice owners were asked to mention the number of their pre-pandemic patient volume per quarter (less than 600; 600–1199; 1200–1799; 1800–2399; 2400 or more patients per quarter; Online Resource 2). Further, it was obtained if pre-interventional testing of patients was performed. If yes, it was asked if the predominantly used method of pre-interventional testing of patients was PCR or antigen testing and if the test was analyzed in an internal or external laboratory. This was separately obtained for inpatients (patients who stayed overnight) and outpatients (patients who did not stay overnight). Further it was asked how many hours prior to the intervention pre-interventional testing had been performed (Online Resource 3). Another question to be answered was if health care worker screening had been performed at least once. If yes, it should be indicated if the method used had been antibody, antigen, PCR testing or another method. Moreover, it was asked if at least one HCW within the facility had been infected with SARS-CoV-2. If yes, it was obtained, how many HCW had been infected with the virus. Two additional questions were, if the number of procedures and the revenue had increased by ≥ 50%, increased by < 50%, decreased by < 50%, decreased by ≥ 50% or was approximately unchanged in the years 2020 compared to the year 2019. Further, it was asked if the number of employees had increased, decreased or was approximately unchanged in the year 2020 compared to the year 2019. Another question was concerning the implied source of infection. For each infection within the facility, it was obtained where the infection had been acquired. The listed options were “private environment”, “during interventions”, “other patient contact”, “without patient contact”, and “unclear origin”. Eventually, the use of personal protective equipment, i.e., mouth and nose protection, FFP2 masks, gowns, goggles, and room ventilation was obtained for quarter one, two and three of the year 2020. Department heads in otolaryngological hospital-based departments and otolaryngological practice owners were addressed in a nationwide survey. The hospital-based departments as well as the private practice owners were recruited via the German Society for Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNO-KHC) and the German Professional Association for Otolaryngologists in Bavaria. The online questionnaire could be answered from December 16, 2020, to January 24, 2021. The questionnaire was created using Unipark®.
Statistical analysis of the subgroup data relating to otolaryngological facilities (as mentioned above) was performed using SPSS IBM® version 25.0. Categorical variables are presented as frequencies and percentages. Ordinal scaled variables are presented as frequencies and percentages. The relationship between nominal scaled variables was tested inferentially using chi-square independence tests. For inferential statistical analyses of ordinal scaled data, Mann–Whitney U test was used for independent groups and Friedmann’s test for related groups. The significance level was set at p < 0.05.
The study was conducted in accordance with the Declaration of Helsinki and the Good Clinical Practice (GCP) guidelines. A positive ethical evaluation of the study was obtained from the Ethics Committee of the Faculty of Medicine of the Technical University of Munich under accession number 713/20 S-SR.
Results
Sample
In total, 66 hospitals (2333 employees) and 395 private practices (2776 employees) were included (Table 1). The response rate was as high as 38.4% among hospital-based departments and 26.4% among private practices. Most hospitals (59.1%) were tertiary care hospitals. Most private practices (34.9%) had treated 1.200–1.799 patients per quarter.
Pre-interventional testing
40.5% of private practices reported to have performed pre-interventional SARS-CoV-2 testing for their outpatients, whereas 68.7% of hospitals stated to have performed pre-interventional testing in their outpatients until the end of 2020 (Table 2). The rate of pre-interventionally tested inpatients was markedly higher for private practices (95.0%) as well as for hospitals (100.0%). The most frequently used testing method was PCR testing for hospitals and private practices in their in- and outpatients, respectively.
Healthcare worker screening
Healthcare workers (HCW) were screened for SARS-CoV-2 at least once in 73.7% of the private practices until the end of 2020 (Table 3). The most frequently used testing method was antigen testing. In hospitals, HCW screening was performed in 77.3% with PCR being the most frequently used method. The frequency of HCW screening in private practices and hospitals did not differ significantly (p = 0.54).
Health care worker status
Overall, 4.1% of all HCW within the included facilities had a SARS-CoV-2 infection confirmed by a positive PCR-test (Table 4). There were significantly more infections among HCW in private practices than among those working in hospital-based departments (4.7% vs. 3.6%; p = 0.03).
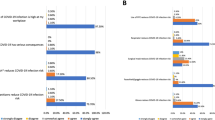
Source of infection
The implied source of infection among HCW identified by the heads of the facilities (head of the department in hospitals, owning physician in private practices) was predominantly the private or home environment followed by an unclear origin of infection for private practices and hospitals (Fig. 1). The rate of infections in the private environment was higher for private practices (63%) than for hospitals (44%) (p < 0.00). Only 14% of infections among HCW in private practices can be attributed to interventions or patient contact, whereas 32% of infections among HCW in hospitals can be attributed to interventions or patient contact (p < 0.00).
Personal protective equipment
In terms of personal protective equipment (PPE), a quarterly comparison in both practices and hospitals shows a decrease in the use of conventional surgical masks (55% Q2 vs. 45% Q4, p < 0.00) in practices and (67% in Q2 vs. 47% in Q4, p = 0.01) in hospitals, with a simultaneous significant increase in the proportion of FFP2 masks used in both facility types (49% Q2 vs. 71% Q4, p < 0.00 in private practices; 26% in Q2 vs. 71% in Q4, p < 0.00) (Fig. 2). Interestingly, practices reported using FFP2 masks significantly more often for procedures in Q3 compared to hospitals (61% vs. 46%, p = 0.01), with this difference levelling out toward the end of the year (71% vs. 71%, p = 1.00). Also evident was an increase in room ventilation between procedures in both practices (36% Q2 vs. 61% Q4, p < 0.00) and hospitals (14% in Q2 vs. 35% in Q4, p < 0.00). In addition, the use of protective eyewear increased over the course of the pandemic. Towards the end of 2020, private practices reported a significantly more frequent room ventilation between procedures compared to hospitals (61% vs. 35%, p < 0.00).
Procedures, revenue and employee development
The number of procedures changed in both practices and hospitals compared to the year before the pandemic. 67.8% (n = 268) of private practices and 78.5% (n = 51) of hospitals reported a decrease in procedures. The number of performed procedures did not change in 27.3% (n = 108) of private practices and 20.0% (n = 13) of hospitals.
The trend in economic revenue was similar. 74.5% (n = 292) of practices and 63.5% (n = 40) of hospitals experienced a decrease of less than 50%. 1.4% (n = 4) of practices and even 17.5% (n = 11) of hospitals reported a decrease in revenue of more than 50% compared to the year before the pandemic. Revenue did not change for 19.9% (n = 78) of practices and 17.5% (n = 11) of hospitals.
18.0% (n = 71) of the surveyed private practices experienced a decrease in the number of employees compared to hospitals with 13.8% (n = 9; p = 0.42). In contrast, only 6.4% (n = 18) of practices experienced an increase in the number of employees and no hospital increased its number of employees. However, most private practices (76.1%, n = 300) and hospitals (86.2%, n = 56) showed stable numbers of employees compared to the year before the pandemic (Table 5).
Discussion
This nationwide study shows data on pre-interventional testing of patients, HCW screening, HCW status, use of personal protective equipment, as well as the economic impact during the course of the SARS-CoV-2 pandemic in a high number of otolaryngological hospital-based departments and private practices in Germany.
A total of 66 otolaryngological hospital-based departments and 395 private practices were included in this survey. In Germany, 168 otolaryngological hospitals exist while the number of otolaryngological practices is unknown [16, 17]. For this reason, the number of included facilities can be considered to be a representative sample of otolaryngological care in Germany. Additionally, by collecting the first two digits of the postal code, it was possible to determine an even distribution of facilities across Germany.
The German interdisciplinary guidelines published in June 2020 recommend pre-interventional PCR testing for SARS-CoV-2 prior to all elective procedures [6], especially because of the high sensitivity and specificity of correctly performed swabs [18]. The present survey shows that these guidelines were widely implemented in inpatients, as 95.0% of the private practices and 100.0% of the hospitals reported performing pre-interventional testing in those patients. On the other hand, only 40.5% of private practices and 68.7% of hospitals, respectively, performed pre-interventional testing in their outpatients. The high rate of untested patients may be one reason for high infection rates among HCW [5]. Furthermore, the difference between outpatient testing among private practices and hospitals showed statistical significance (40.5% vs. 68.7%; p = 0.01), which may be due to a higher economic pressure in the private practice sector compared to the average hospital. In terms of the method of pre-interventional testing, 16.6% of private practices and 14.8% of hospitals performed antigen testing among their inpatients and 21.7% of private practices and 38.7% of hospitals performed antigen testing in their outpatients, respectively. Since antigen tests have a lower sensitivity than PCR tests, especially in asymptomatic patients [19], these results emphasize the necessity for close adherence to the above-mentioned guidelines.
To date, there is no general recommendation of HCW screening for SARS-CoV-2, although a rate of 3% of asymptomatic infections among HCW has been shown [6, 7]. Nevertheless, 73.7% of private practices and 77.3% of hospitals in the present cohort reported to have performed HCW screening at least once. While most private practices used antigen tests (55%), the primary method in hospitals was PCR testing (71%; p < 0.00). This may be explained by a higher availability of laboratories performing PCR tests in hospitals. As asymptomatic HCW may be responsible for a certain number of infections among hospitalized patients, regularly performed HCW screening might avoid nosocomial SARS-CoV-2 infections in the future.
Most infections in HCW were stated to be attributed to the private or home environment with significantly more infections attributed to the private environment among HCW in private practices (63%) than among HCW in hospitals (44%, p < 0.00). These findings correlate with results from a Turkish study, which revealed that work breaks spent together and non-compliance with physical and social distance rules among HCW were found to be statistically significant risk factors of SARS-CoV-2 infection [20]. Additionally, PPE is not used in the private environment which may also contribute to an increased risk of transmission in the private environment.
The rate of SARS-CoV-2 infections among HCW was as high as 4.1% in the present study compared to an infection rate of 2.5% among the general population on the 21st January 2021 in Germany [21, 22]. This is in line with recent data showing a higher risk of infection among HCW compared to the general population [5, 23]. One reason for the higher rate of infections among HCW may be additional exposure at the workplace although a high rate of infections among HCW in otolaryngological private practices and hospitals was attributed to the private environment (as discussed above). Additionally, the rate of HCW screening for a SARS-CoV-2 infection was high (77.3% in hospitals, 73.7% in private practices), which possibly contributes to a higher rate of HCW infections compared to the general population as potentially more asymptomatic infections were detected. Further, there were significantly more infections among HCW in private practices than among those working in hospital-based departments (4.7% vs. 3.6%; p = 0.03). This may partly be explained by a significantly lower percentage of pre-interventional testing among outpatients in private practices (40.5%) than in hospital-based departments (68.7%) leading to a higher risk of HCW infection in otolaryngological private practices than in hospitals.
AGP such as tracheostomy, CO2 ablation, nasopharyngoscopy and laryngoscopy are regularly performed in otolaryngology. In February 2020, the European Center for Disease Prevention and Control recommended the use of FFP2/FFP3 masks, goggles and gowns for AGP [24]. Additionally, room ventilation is widely recommended for the reduction of the risk of transmission, as transmission rates for respiratory tract infections have been shown to be increased in indoor spaces with poor ventilation [25]. The present study shows that both private practices and hospitals showed a decreased use of surgical masks and a simultaneously increased use of FFP2 masks over the course of the pandemic leading to a reported use of FFP2 masks in 71% of private practices and hospitals in Q4. It must be emphasized that 29% of all facilities reported not using FFP2 masks in Q4, potentially leading to an increased risk of infection. Moreover, the use of gowns, protective eyewear, and room ventilation increased from Q2 to Q4 in both private practices and hospitals, although rates of use were still fairly low by the end of 2020. For further transmission risk reduction, this rate should be increased.
To the best of our knowledge, this is the first study evaluating the economic impact of the COVID-19 pandemic on otolaryngological private practices and hospitals in Europe. The reported number of procedures decreased by less than 50% in 56.7% of the private practices and in 63.1% of the hospitals when comparing the years 2019 and 2020. A decrease of more than 49% of procedures was only reported in 11.1% of the private practices and in 15.4% of the hospitals, respectively (p = 0.41). In contrast, a study that included 10 otolaryngological private practices in Massachusetts showed a mean decrease of 90% of endoscopic sinus surgeries, 89% of tonsillectomies and/or adenoidectomies, 93% of septoplasties, 85% of cerumen removals, and 77% of flexible and rigid endoscopies when comparing procedures in weeks 11–16 of 2019 to 2020 data [26]. In our study, the number of employees remained unchanged in 76.1% of the private practices and 86.2% of the hospitals, while 18.0% of the private practices and 13.8% of the hospitals reported a decrease in the number of employees when comparing 2019 and 2020. In contrast, the study from Massachusetts showed that 90% of the private practices had reduced working hours and 80% of practices furloughed their employees [26]. These results suggest that the economic impact on otolaryngological private practices and hospital-based departments in Germany seems to be relatively mild compared to those in the USA. This may in part be due to a lower grade of privatization in healthcare when comparing the German to the American healthcare system. Though, an employment decrease of 18.0% in otolaryngological private practices and 13.8% in otolaryngological hospital-based departments within one year will possibly lead to a noticeable increase of unemployment with subsequent socioeconomic consequences among HCW. It is to be hoped that the rate of unemployment will rapidly decrease as soon as the pandemic comes to an end and the volume of patients increases. Finally, 74.5% of private practices and 63.5% of hospitals experienced a decrease in revenue of 50% or less when comparing 2019 and 2020. A significantly higher percentage of hospitals (17.5%) than private practices (2.6%, p < 0.00) reported a decrease in economic revenue of more than 49%. This finding may in part be explained by the fact that many otolaryngological hospitals were forced to assign their employees to infection wards with subsequently lower surgery capacities while this was not the case for private practices. A decreased revenue will not only lead to further growth of unemployment among HCW but also affect practice owners and companies providing hospital services themselves.
This study has several limitations. First, due to the study design with recruitment of participants via the German Society for Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNO-KHC), a selection bias cannot be ruled out. In addition, the questionnaire was addressed to the head of the department concerned or the practice owner, who answered the questions for the respective institution according to their own level of knowledge. Further, the reported HCW status was not confirmed by seroprevalence in this study. Finally, testing strategies differed between hospitals and private practices, which must be kept in mind when comparing patterns of SARS-CoV-2 employee positivity between the two settings.
Conclusion
The present study included a high number of otolaryngological departments as well as private practices in Germany and demonstrates important data on pre-interventional testing, the use of PPE, HCW screening, HCW status and the economic impact of the COVID-19 pandemic. The data shows that the frequency of pre-interventional testing in outpatients has room for improvement. Furthermore, the rate of HCW infections was significantly higher in private practices than in hospital-based departments. In addition, an important source of infection among HCW seems to be the private or home environment. Finally, the economic impact of the pandemic on otolaryngological private practices and hospitals is evident, however, the number of employees in a high rate of facilities remained unchanged through the pandemic.
References
Meng L, Hua F, Bian Z (2020) Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res 99(5):481–487
Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Biomed 91(1):157–160
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the chinese center for disease control and prevention. JAMA 323(13):1239–1242
Johns Hopkins University CVRC (2021) https://coronavirus.jhu.edu/data/mortality. Accessed 27 Mar 2021
Kambhampati AK, O’Halloran AC, Whitaker M, Magill SS, Chea N, Chai SJ et al (2020) COVID-19–associated hospitalizations among health care personnel—COVID-NET, 13 states, march 1–may 31, 2020. Morb Mortal Wkly Rep 69(43):1576
Meyer HJ, Deitmer T, Schmidt-Rixen T, Roissant R, Janssens U, Chaberny I, Liebert U, Wienke A (2020) Interdisziplinär abgestimmte Empfehlungen zum Personal- und Patientenschutz bei Durchführung planbarer Eingriffe zur Zeit der SARS-CoV-2-Pandemi. AWMF-S1-Leitline
Rivett L, Sridhar S, Sparkes D, Routledge M, Jones NK, Forrest S et al (2020) Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife 9:e58728
Ran L, Chen X, Wang Y, Wu W, Zhang L, Tan X (2020) Risk factors of healthcare workers with coronavirus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis 71(16):2218–2221
Sowerby LJ, Stephenson K, Dickie A, Lella FAD, Jefferson N, North H et al (2020) International registry of otolaryngologist-head and neck surgeons with COVID-19. Int Forum Allergy Rhinol 10(11):1201–1208
Rameau A, Young VN, Amin MR, Sulica L (2020) Flexible laryngoscopy and COVID-19. Otolaryngol Head Neck Surg 162(6):813–815
Chiesa-Estomba CM, Lechien JR, Calvo-Henriquez C, Fakhry N, Karkos PD, Peer S et al (2020) Systematic review of international guidelines for tracheostomy in COVID-19 patients. Oral Oncol 108:104844
Thamboo A, Lea J, Sommer DD, Sowerby L, Abdalkhani A, Diamond C et al (2020) Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology–head and neck surgery during the COVID-19 pandemic. J Otolaryngol Head Neck Surg 49:1–14
McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS et al (2020) Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med 8(7):717–725
Herzog M, Beule A, Lüers J-C, Guntinas-Lichius O, Grafmans D, Deitmer T. Das erste Jahr der Pandemie mit SARS-CoV-2–Auswirkungen auf die Hals-Nasen-Ohren-Heilkunde. Hno. 2021:1–8
Bundesministerium für Gesundheit (2020) http://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html. Accessed 27 Mar 2021
Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde Kopf- und Hals-Chirurgie eV, Bonn. DGHNO-Übersicht: Universitäts-HNO-Kliniken. https://www.hno.org/anschriften/klinik_unihtml. Accessed 02 Apr 2021
Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie eV, Bonn. DGHNO-Übersicht: Kliniken / Zentren mit HNO-Hauptabteilung. http://www.hno.org/anschriften/klinikenhtml. Accessed 02 Apr 2021
Wolfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Muller MA et al (2020) Virological assessment of hospitalized patients with COVID-2019. Nature 581(7809):465–469
Mina MJ, Parker R, Larremore DB (2020) Rethinking covid-19 test sensitivity—a strategy for containment. N Engl J Med 383(22):e120
Çelebi G, Pişkin N, Bekleviç AÇ, Altunay Y, Keleş AS, Tüz MA et al (2020) Specific risk factors for SARS-CoV-2 transmission among health care workers in a university hospital. Am J Infect Control 48(10):1225–1230
Robert Koch Institut (2021) Täglicher Lagebericht des RKI zur Coronavirus-Ksrankheit-2019 (COVID-19). https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Jan_2021/2021-01-21-depdf?__blob=publicationFile. Accessed 10 Jun 2021
Statistisches Bundesamt Destatis (2021) Bevölkerungsstand Deutschland. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Bevoelkerungsstand/_inhalthtml. Accessed 10 Jun 2021
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W et al (2020) Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5(9):e475–e483
European Center for Disease Prevention and Control (2020) Personal protective equipment (PPE) needs in healthcare settings for the care of patients with suspected or confirmed novel coronavirus (2019-nCoV). https://www.ecdc.europa.eu/sites/default/files/documents/novel-coronavirus-personal-protective-equipment-needs-healthcare-settingspdf. Accessed 03 Apr 2021
Knibbs LD, Morawska L, Bell SC, Grzybowski P (2011) Room ventilation and the risk of airborne infection transmission in 3 health care settings within a large teaching hospital. Am J Infect Control 39(10):866–872
Fan T, Workman AD, Miller LE, Sakats MM, Rajasekaran K, Brant JA et al (2021) The impact of COVID-19 on Otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg 194599820983732.
Acknowledgements
The authors thank all the participants for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institution or practice at which the studies were conducted. The study was approved by the Ethics Committee of the Faculty of Medicine of the Technical University of Munich.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mayer, M., Zellmer, S., Zenk, J. et al. Status quo after one year of COVID-19 pandemic in otolaryngological hospital-based departments and private practices in Germany. Eur Arch Otorhinolaryngol 279, 1063–1070 (2022). https://doi.org/10.1007/s00405-021-06992-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06992-2