- All India Institute of Medical Sciences, Rishikesh, Rishikesh, India
Introduction: The COVID-19 pandemic was soon declared a global health threat and had significant economic and health implications. Unprecedented government measures brought massive shifts in teaching-learning pedagogy in nursing to curb the infection. The study was conducted to explore the predictors of pandemic fatigue among nursing undergraduates and mediating role of individual resilience and coping styles during the third wave in India.
Methods: This online survey included 256 undergraduate nursing students studying at Tertiary Care Teaching Hospital in North India. Lockdown/Pandemic Fatigue Questionnaire, Brief Resilience Scale, and Coping Behavior Questionnaire were used to collect the information. Appropriate descriptive and inferential statistics were applied to compute the results.
Results: Nursing undergraduates reported a moderate level of fatigue during the restrictions imposed at the time of the third wave. Students’ year of study (p = 0.001), tested positive during pandemic (p = 0.003), and post-COVID-19 hospitalization (p = 0.026) were found associated with higher fatigue status. Advanced age (p = 0.046) and higher personal resilience status (p < 0.001) were associated with lower fatigue levels. Resilience status (ß = − 4.311 p < 0.001) and second year of study (ß = 3.198, p = 0.015) were reported as independent predictors of pandemic fatigue in students.
Conclusion: Findings suggest that lockdown-related fatigue was common in nursing undergraduates. Considering negative consequences on mental health, routine psychosocial screening of the nursing students should be conducted. Recommending stress-relieving measures should be enforced to help nursing undergraduates to combat lockdown-induced exhaustion.
Introduction
The COVID-19 pandemic cases were detected in Wuhan in China’s Hubei province for 2 years (Aslan and Pekince, 2021). The COVID-19 pandemic was declared a global threat and significantly impacted each area of life, including health and economics (Labrague and Ballad, 2021). Every government has taken unprecedented measures to control further transmission, including mandatory lockdown, strict social distancing, frequent handwashing, and mandatory home quarantine or isolation after traveling to other parts or another country (Dharra and Kumar, 2021).
In India, the government imposed a countrywide lockdown and a partial lockdown named “night curfew” since the pandemic, forcing people to stay at home, reducing social interaction and physical activities, and leaving them with many psychosocial issues (Kumar et al., 2021). In addition, medical schools around the globe were also shut down before the pandemic reached on peak and left the students amid course completion dilemmas (Harries et al., 2021). However, government mitigating measures, including lockdown and social distancing, helped slow down the transmission of the virus but adversely affected the physical and psychological health and wellbeing of all categories of people, including nursing students (Labrague and Ballad, 2021).
Medical and nursing staff always take the forefront of any particular pandemic or outbreak and risk their lives. They are more prone and vulnerable to getting infection considering close contact with the infection, high stress, lack of rest, and extended duty hours in the hospital (Luberto et al., 2020). Extending course deadlines and duration might further intensify the stress and anxiety among nursing students (Huang et al., 2020). The changes in teaching-learning pedagogy and curriculum delivery of the nursing students might be expected to intensify students’ stress further. In addition, changes in the routine of academic, social restriction, and lifestyle behavior might negatively impact psychological wellbeing (Aslan and Pekince, 2021). Sadly, many health professionals lost their lives while providing care to patients with coronavirus at the hospital in the ongoing pandemic—every new strain of virus hammering the mental health of everyone and creating more panic among health professionals (Aslan and Pekince, 2021).
Resilience is a personality trait that helps an individual become strong and bounce back during a stressful situation or help to cope with adverse conditions (Hamadeh Kerbage et al., 2021). A higher resilience will help adapt to a stressful situation and help deal with mental, emotional, and educational challenges. Earlier literature reported the importance of resilience, ineffective adjustment, improving social relationships, social support, and psychological wellbeing (Yu et al., 2019). Indeed, resilience is considered one of the critical personality attributes affecting the retention of nursing students in their studies (Moloney et al., 2018).
Evidence shows that health professionals and university college students reported a higher incidence of psychological stress than the general population (Luberto et al., 2020). These students are more vulnerable to developing emotional problems, anxiety, stress, and depression considering fear of failure, time crisis, session duration change, exam pattern and timing, neglected self-care, and social restrictions to meeting family and friends (Dyrbye and Shanafelt, 2016; Yu et al., 2019). Huge uncertainties and confusion about the fixed deadline for the pandemic left the students with many questions related to their career selection and future (Agu et al., 2021). Still, there is no light on the other side of dark tunnels, and experts speculate vividly to end this pandemic.
Therefore, there is a pressing need to explore predictors of pandemic fatigue and understand the mediating role of resilience and coping on health after 2 years of the pandemic in nursing undergraduates.
Materials and Methods
Design, Sample, and Settings
This online cross-sectional survey was conducted after the end of the second wave of coronavirus in India when daily cases were reached below 10,000. At the same time, a new strain of COVID-19, Omicron, was knocking on the door to spread panic around the globe. The survey link was supplied with a consent form and asked each participant to provide consent before participating in the online survey. The survey questionnaire, Google Forms, was shared with 300 nursing students on the WhatsApp number of an individual nursing student, and 278 (92.66%) participants responded to the survey. Finally, after carefully scrutinizing the filled questionnaire, 256 questionnaires were deemed suitable for the analysis.
Instrumentations
Three structured and standardized questionnaires were used in the study. The Pandemic/Lockdown Fatigue Scale, the Brief Resilience Scale, the Brief Coping Questionnaire, and structured socio-demographics datasheet are used to collect personal and professional information from the participants.
Socio-Demographic Sheet
It consists of information on age, year of study, experience as a bedside nurse, being infected with COVID-19 virus and quarantine status and days, admission to hospital after getting an infection, and loss of family members due to COVID-19 infection. A group of microbiology, nursing, and infectious disease experts was requested to validate the profile. The inclusion items were based on more than 80% expert consensus for the items’ relevancy.
Pandemic/Lockdown Fatigue Scale
This scale was used to assess the exhaustion level among nursing students associated with frequent preventive measures like quarantine, home isolation, and other government-imposed guidelines to stop the spread of the transmission of the COVID-19 virus. It is a ten-item Likert scale ranging from 1 (never) to 5 (always) with a maximum possible score of 50. The scale has an excellent criterion validity and acceptable concurrent validity in earlier similar work (Michielsen et al., 2003; Labrague and Ballad, 2021). The scale’s internal consistency was measured using Cronbach’s alpha and was 0.84 for the present study. The scale content validation sought by the experts in microbiology, nursing, and internal medicine and scale rated relevant and appropriate for the interest of the population. The test–retest validity of the scale was 0.82 in the present study.
Brief Resilience Scale
The scale was used to determine the participants’ ability to bounce back in unpleasant or difficult situations associated with pandemics and subsequent measures used to stop transmission during the pandemic. Students answered the scale by responding to a 5-point Likert scale ranging from 5 (describe me very well) to 0 (does not describe me at all). The scale is well validated in similar previous work (Smith et al., 2008; Labrague and Ballad, 2021), and in the present study, the internal consistency value of the scale was 0.88. The scale’s test–retest reliability was 0.89 in the present study.
Coping Behavior Questionnaire
The present study used a coping behavior questionnaire to measure the nursing undergraduates’ coping measures during a mandatory lockdown or restriction period. The students were requested to respond to this eight-item 5-point Likert scale ranging from 5 (strongly agree) to 1 (strongly disagree). The scale shows excellent criterion validity and acceptable reliability in earlier work reporting an internal consistency value of 0.85 (Savitsky et al., 2020; Labrague and Ballad, 2021). In the current study, the scale’s internal consistency was 0.83.
Ethical Considerations
The study was approved by the Institutional Ethics Committee (AIIMS/IEC/21/642). The survey link also provided a consent form as a mandatory requirement to participate. However, the participants were ensured to protect privacy and confidentiality at each data collection stage and dissemination of the findings. Further, no personal information was obtained to protect the privacy and confidentiality of the students.
Results
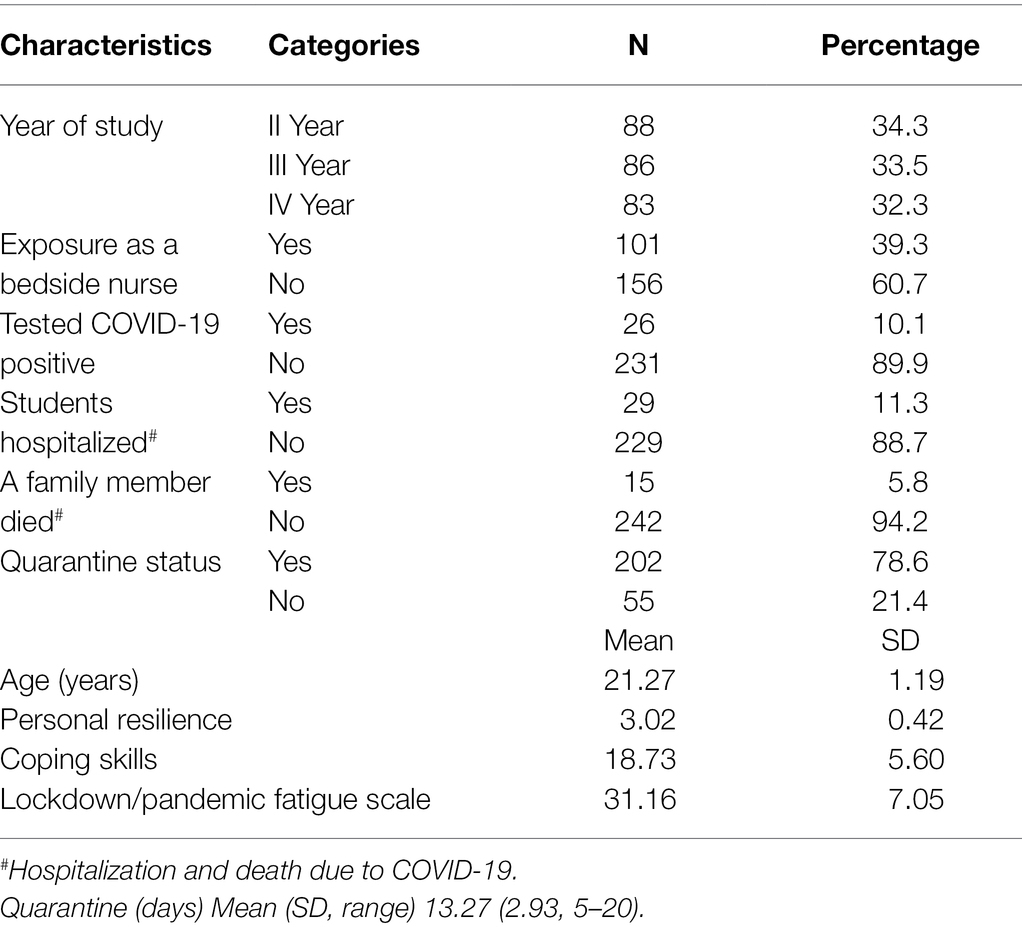
In this online survey, 256 nursing undergraduates studied in a nursing college associated with a teaching hospital were included. The mean age of the students was 21.27 years, with a standard deviation of 1.19 years. All the students were female, considering the admission to female students in the institute. A more significant number of students were from the second year (34.3%), followed by the third year (33.5%) and fourth year (32.3%). Since there was no admission for the new batch due to an ongoing pandemic, there was no participation from the first-year students. 39.3% of students were deployed as bed nurses during the pandemic and had experience as bedside nurses in the hospital. 11.3% of students were hospitalized after testing positive for COVID-19 (10.1%) during the ongoing pandemic.
Further, more than three fourth of students underwent quarantine (78.6%), with a mean duration of 13.27 days of quarantine. Sadly, 5.8% of students lost one of their family members in the pandemic after getting COVID-19. The mean scores for the coping and personal resilience measures were 18.74 (SD: 5.60) and 3.02 (SD: 0.42), respectively (Table 1).
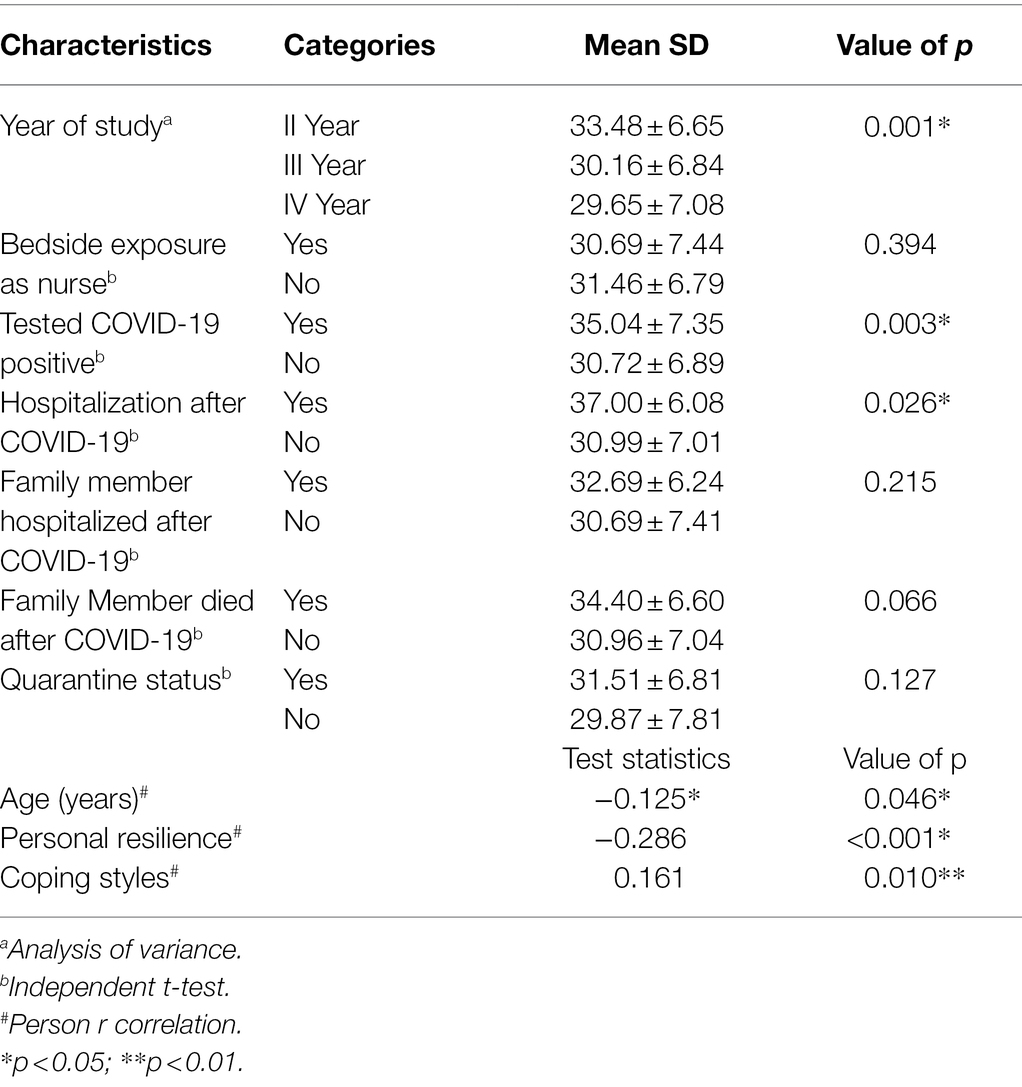
Table 2 shows the students’ responses on the lockdown/pandemic fatigue scale. The mean fatigue scale score was 31.16 (SD: 7.05) out of the maximum possible score of 50. An independent sample t-test shows a significantly higher mean score (p = 0.026) on the fatigue scale for students deployed as bedside nurses during the COVID-19 pandemic than another group. Likewise, students who tested positive during the pandemic reported significantly higher mean scores (p = 0.003) than their counterparts. Further, it has been reported that second-year class students especially said higher fatigue scores (p = 0.001) than third and final-year students. This can be interpreted that higher class students might be experienced enough to handle patients in clinical after their earlier class experiences and hence reported lower fatigue scores compared to second-year students who are a novice and directly deployed to the clinical areas in a serious pandemic situation. Pearson’s correlation coefficient showed a significant negative relationship between age (r = −0.125, p = 0.046) and personal resilience status (r = −0.286, p = <0.01), and lockdown fatigue. However, coping styles showed a positive relationship with lockdown fatigue (r = 0.161, p = 0.010; Table 2).
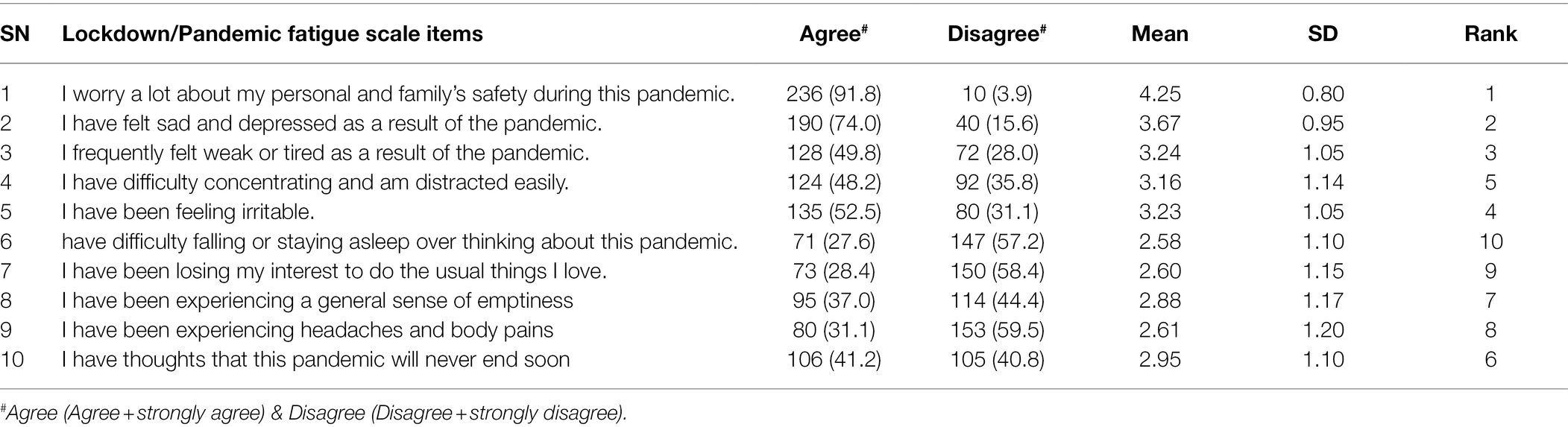
Findings revealed that a few of the items, ‘I worry a lot about my personal and family’s safety during this pandemic’ (m = 4.25), ‘I have felt sad and depressed as a result of the pandemic’ (m = 3.67), and ‘I frequently felt weak or tired as a result of the pandemic’ (m = 3.24) reported more frequently by the participants. On the contrary, a few items that received lower attention were ‘I have difficulty falling or staying asleep over thinking about this pandemic’ (m = 2.58), ‘I have been losing my interest in doing the usual things I love’ (m = 2.60), and ‘I have been experiencing headaches and body pains’ (m = 2.61). Further, looking at the agreement status to fatigue items showed that 91.8% of participants responded that they are worried about personal and family members in the pandemic. Likewise, around two-thirds of the participants (74%) reported feeling depressed and sad during the pandemic, and more than half of the participants (52.5%) felt irritated by a pandemic or its related consequences (Table 3).
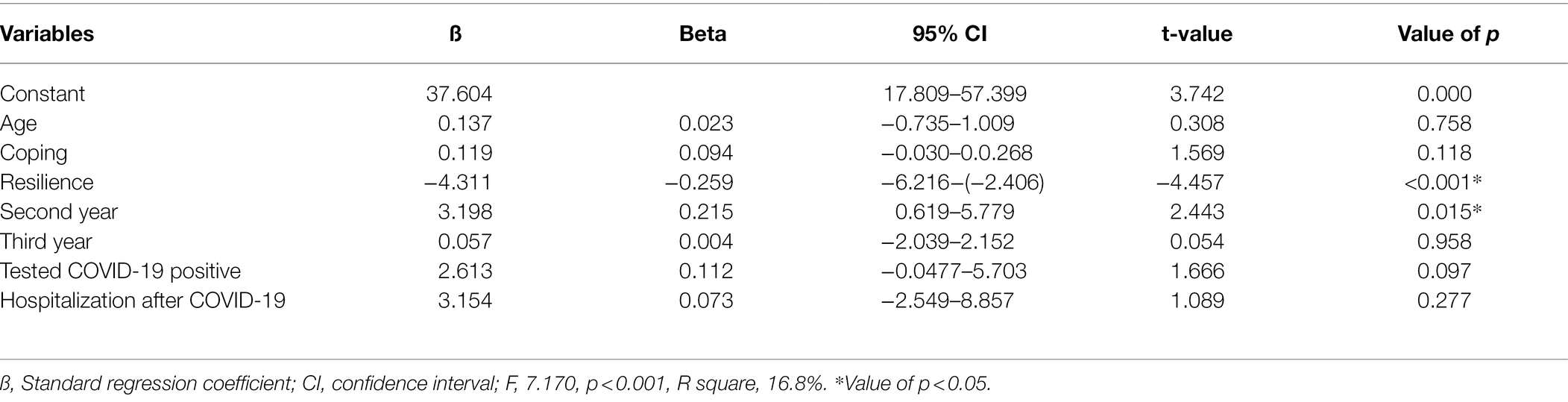
Variables that showed a significant association with lockdown fatigue were entered into the multiple linear regression model. The model explained 16.8% in the variance of the lockdown fatigue, which was statistically significant (F = 7.170, p = <0.001), which indicated the model fit the variables. Out of inserted variables in the model, personal resilience and the second year of the study predicted lockdown fatigue among participants. This can be interpreted as those students who are studying in the lower class (β = 3.198, p = 0.015) and had poor resilience status (β = −4.311, p = <0.001) reported higher fatigue during the ongoing pandemic (Table 4).
Discussion
The current digital survey was conducted to study the pandemic fatigue and the influence of nursing undergraduates’ socio-demographic variables, coping styles, and resilience in mediating fatigue during the third wave of the COVID-19 pandemic between February and May 2021. The government has taken unprecedented measures to curb the further infection of different variants of the COVID-19 virus from time to time. Further, the authors presumed that the sudden shifting of traditional classroom teaching and clinical learning to virtual learning coupled with home or hostel confinement and reduced physical activities during the COVID-19 pandemic might lead to more fatigue in nursing students (Liu et al., 2021). In the certain phase of the pandemic, nursing students are confined in the hostel or wherever they are, which further intensifies many psychological problems, including anxiety, depression, and fatigue (Brooks et al., 2020). Heavy clinical load, daily infection precautionary measures at work and hostel, reduced social connections, and social distancing could lead to mental fatigue, anxiety, frustration, and boredom (Brooks et al., 2020; Chao et al., 2020; Morales-Rodríguez, 2021).
Participants’ mean fatigue score was 31.16 (SD: 7.05), indicating moderate fatigue status during the ongoing pandemic. A crunch of studies used the lockdown/pandemic fatigue scale; hence, authors find it challenging to compare these findings. However, our study results are in line with a study conducted (Labrague and Ballad, 2021) at Muscat, Oman, on college students who used the pandemic fatigue scale (PFS) reported a similar level of fatigue (31.54; SD: 6.93) during the pandemic. Further, a Chinese study (Liu et al., 2021) reported that more than 67.3% of nursing students said fatigue which is almost doubled (36%) to work conducted (Geiger-Brown et al., 2012) on nurses working in different shifts using the Occupational Fatigue Exhaustion Recovery Scale. Our findings are in consensus with the work (Teng et al., 2020), who reported fatigue in 73.7% of frontline healthcare workers during an initial COVID-19 outbreak in China as measured by the Fatigue Self-Assessment Scale (Teng et al., 2020). These results further follow another work from Australia; a few months after lockdown, the Chalder Fatigue Questionnaire reported a significant level of fatigue (Nitschke et al., 2021). Shreds of evidence from the United States, Saudi Arabia, and India report a substantial amount of tiredness, and increased fatigue, boredom, worry, and loneliness, suggesting some efforts to support the affected population to combat the adverse effect of prolonged lockdown, confinement, and other confinement measures imposed by government time to time (Majumdar et al., 2020; Meo et al., 2020). In contrast, medical students’ fatigue status was relatively low (13.8%) before the COVID-19 outbreak (Abdali et al., 2019). Owing to different measurement tools on fatigue between different studies across the globe indicates cautious interpretations and extrapolating of the findings. Considering the negative impact of fatigue on the individual’s physical, mental, cognitive, and behavioral functions (Trendall, 2000), it is imperative to devise support or other stress-relieving strategies to benefit mental health.
The symptoms of fatigue among nursing undergraduates, lack of concertation, irritation, disturbed sleep, feeling depressed and emptiness, and tired are other symptoms reported by the students. These symptoms are in line with the earlier Indian work conducted on professionals and students who reported various indicators of symptoms, including anxiety, higher stress, feeling of sleeplessness, depression, a safety concern for family, tiredness, and worry for personal safety and other physical discomforts, during the lockdown (Majumdar et al., 2020). The reported fatigue symptomatology in this study was similar to the report of the symptoms presented by Australian Psychological Society (2020), which reported a loss of interest in previously enjoyed activities, physical exhaustion, fear, anxiety, emotional outburst, reduced motivation, depression, and difficulty in focusing and problem-solving as a typical array of symptoms of lockdown fatigue.
Students’ year of study, COVID-19 positive status, and post-COVID-19 hospitalization directly impacted the development of lockdown fatigue. In particular, final-year and third-year students reported lower lockdown fatigue than second-year students. These findings are anticipated, as, during the study, students will be exposed to different clinical conditions and environments to develop positive temperament and adaptive behavior to work with different kinds of patients, which help a student to further deal with such kind of disastrous conditions (Benner, 2004; Sonika and Kumar, 2019). The present study’s findings of lower stress among the higher level of education are also in consensus with the previous studies conducted on nursing students (Kumar and Nancy, 2011; Dharra and Kumar, 2021). Furthermore, previous work on stress among nursing students showed a declining trend as they progress to higher studies, similar to the present report (Kumar and Nancy, 2011; Fornés-Vives et al., 2016). These findings of higher stress in lower-class students indicate developing an evidence-based support system through evidence-based intervention to assist budding nurses in developing coping strategies and adaptative resilience to deal with such disastrous situations effectively.
Further, regression analysis findings showed a significant negative association of personal resilience with lockdown fatigue, suggesting a protective role of individual resilience against the negative consequences of restrictions faced during mandatory home isolation or quarantine during the pandemic. These study findings align with the earlier work that reported a significant negative relationship between personal resilience and lockdown fatigue in college students (Labrague and Ballad, 2021). Close similar findings presented in earlier work reported a positive impact of personal resilience on improving mental health and psychological outcomes among different populations around the globe (Tsay et al., 2001; Charuvastra and Cloitre, 2008; Ran et al., 2020). The study findings draw the mentor and teachers’ attention to building resilience as a strategy to help a student bounce back from such adversity and traumatic situations. To our current knowledge, this is the first of its study in the area, highlighting the impact of individual resilience and coping styles on combating negative consequences on mental health associated with a pandemic, hence supplementing the existing knowledge in this area of research.
Students who used higher coping styles showed higher lockdown fatigue in the current study. Previous studies on nursing students also have identical findings for a significant correlation between fatigue and nursing students’ coping (Nurhidayati et al., 2021). Likewise, another study reported a significant relationship between coping mechanisms and fatigue, suggesting a positive impact of coping mechanisms on fatigue during adverse situations (Michalec et al., 2013). In contrast, the findings on the relationship between coping and fatigue are in non-accordance with many previously published studies that reported a negative relationship between coping mechanisms and fatigue (Tugade and Fredrickson, 2004; Cao et al., 2020; Tull et al., 2020). These contentious findings on coping and fatigue provide additional knowledge to understand the precise mediating effect of coping mechanisms in acute and chronic adversity, including the current pandemic. Instead, higher coping use in students might help reduce fatigue and other mental health issues, including irritation, sleeplessness, distraction, sadness, and body aches compared to students not or less use of coping strategies as mentioned in earlier research (Labrague and De los Santos, 2020; Labrague, 2021; Roberts et al., 2021). However, authors speculate the use of a different tool and longer duration of a pandemic for such unforeseen results on the relationship between coping and fatigue. However, it is vital to devise strategies to improve resilience and coping mechanisms among nursing students to maintain and improve their mental health and overall psychological well-being.
Limitations
The study should be appraised under many limitations, and other researchers should be cautious while interpreting and extrapolating the results. First, the cross-sectional nature of the survey impedes computing the exact relationship between different variables, including fatigue, coping, and resilience. It is difficult to interpret from the study that higher resilient and coping mechanisms students have lesser fatigue during the lockdown in comparison to counterparts. Hence, the authors recommend using different study designs, including randomized controlled trials or case–control studies, to understand the mediating effect of resilience in improving fatigue and coping skills in students. Second, a study with a higher sample size is recommended to enhance generalizability over other similar populations. Third, online surveys carry inherent bias, including social-desirability bias, and need caution to interpret the findings.
Conclusion
As per the findings, lockdown-related fatigue was common in nursing undergraduates during the third wave of the COVID-19. Further, the junior students reported tested positive and were hospitalized during the pandemic reported higher fatigue than their counterparts. The study reported that senior students with higher resilience levels said lower fatigue, indicating the significance of perceived professional self-confidence and the need for preparation and precautions to take in a disease outbreak. These findings also reflect the necessity of developing junior students’ professional competencies and patient handling. However, a structured curriculum and adequate clinical exposure will train the students in developing professional competencies and patient handling skills.
Implications for Nursing Management
Nursing students face enormous challenges during the ongoing pandemic, including the transition of teaching-learning pedagogy, deployment in different levels of clinical assignment, and many other personal and professional obligations. Individual resilience helps beat the negative consequences of pandemic fatigue in nursing students. Nursing educators should prioritize proactive measures to reduce pandemic-induced fatigue and strengthen personal resilience among students. Resilience promotional strategies could be an alternative intervention to improve more use of positive coping strategies to enhance the mental health promotion of nursing students.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation on a individual request of a researcher to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee, All India Institute of Medical Sciences, AIIMS Rishikesh. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RK considered and designed the study, conducted research, provided research materials, and collected and organized data. KB wrote the initial and final draft of the manuscript and provided logistic support. YB analyzed and interpreted data and did the final editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdali, N., Nobahar, M., and Ghorbani, R. (2019). Evaluation of emotional intelligence, sleep quality, and fatigue among Iranian medical, nursing, and paramedical students: A cross-sectional study. Qatar Med. J. 2019:15. doi: 10.5339/qmj.2019.15
Agu, C. F., Stewart, J., McFarlane-Stewart, N., and Rae, T. (2021). COVID-19 pandemic effects on nursing education: looking through the lens of a developing country. Int. Nurs. Rev. 68, 153–158. doi: 10.1111/inr.12663
Aslan, H., and Pekince, H. (2021). Nursing students' views on the COVID-19 pandemic and their percieved stress levels. Perspect. Psychiatr. Care 57, 695–701. doi: 10.1111/ppc.12597
Australian Psychological Society. (2020). Managing lockdown fatigue. Available at: https://psychology.org.au/getmedia/74e7a437-997c-4eea-a49c-30726ce94cf0/20aps-is-covid-19-public-lockdown-fatigue.pdf (Accessed January 20, 2022).
Benner, P. (2004). Using the dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bull. Sci. Technol. Soc. 24, 188–199. doi: 10.1177/0270467604265061
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287:112934. doi: 10.1016/j.psychres.2020.112934
Chao, M., Chen, X., Liu, T., Yang, H., and Hall, B. J. (2020). Psychological distress and state boredom during the COVID-19 outbreak in China: the role of meaning in life and media use. Eur. J. Psychotraumatol. 11:1769379. doi: 10.1080/20008198.2020.1769379
Charuvastra, A., and Cloitre, M. (2008). Social bonds and posttraumatic stress disorder. Annu. Rev. Psychol. 59, 301–328. doi: 10.1146/annurev.psych.58.110405.085650
Dharra, S., and Kumar, R. (2021). Promoting mental health of nurses During the coronavirus pandemic: will the rapid deployment of Nurses' training programs During COVID-19 improve self-efficacy and reduce anxiety? Cureus 13:e15213. doi: 10.7759/cureus.15213
Dyrbye, L., and Shanafelt, T. (2016). A narrative review on burnout experienced by medical students and residents. Med. Educ. 50, 132–149. doi: 10.1111/medu.12927
Fornés-Vives, J., Garcia-Banda, G., Frias-Navarro, D., and Rosales-Viladrich, G. (2016). Coping, stress, and personality in Spanish nursing students: A longitudinal study. Nurse Educ. Today 36, 318–323. doi: 10.1016/j.nedt.2015.08.011
Geiger-Brown, J., Rogers, V. E., Trinkoff, A. M., Kane, R. L., Bausell, R. B., and Scharf, S. M. (2012). Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol. Int. 29, 211–219. doi: 10.3109/07420528.2011.645752
Hamadeh Kerbage, S., Garvey, L., Willetts, G., and Olasoji, M. (2021). Undergraduate nursing students' resilience, challenges, and supports during corona virus pandemic. Int. J. Ment. Health Nurs. 30, 1407–1416. doi: 10.1111/inm.12896
Harries, A. J., Lee, C., Jones, L., Rodriguez, R. M., Davis, J. A., Boysen-Osborn, M., et al. (2021). Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study. BMC Med. Educ. 21:14. doi: 10.1186/s12909-020-02462-1
Huang, L., Lei, W., Xu, F., Liu, H., and Yu, L. (2020). Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS One 15:e0237303. doi: 10.1371/journal.pone.0237303
Kumar, R., and Nancy, N. (2011). Stress And coping strategies Among nursing students. Nurs. Midwifery Res. J. 7, 141–151. doi: 10.33698/nrf0134
Kumar, R., Singh, V., Mohanty, A., Bahurupi, Y., and Gupta, P. (2021). Corona health-care warriors in India: knowledge, attitude, and practices during COVID-19 outbreak. J. Educ. Health Promot. 10:44. doi: 10.4103/jehp.jehp_524_20
Labrague, L. J. (2021). Pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment during the covid-19 pandemic: The mediating role of resilience. J. Nurs. Manag. 29, 1992–2001. doi: 10.1111/jonm.13383
Labrague, L. J., and Ballad, C. A. (2021). Lockdown fatigue among college students during the COVID-19 pandemic: predictive role of personal resilience, coping behaviors, and health. Perspect. Psychiatr. Care 57, 1905–1912. doi: 10.1111/ppc.12765
Labrague, L. J., and De los Santos, J. A. A. (2020). COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 28, 1653–1661. doi: 10.1111/jonm.13121
Liu, S., Xi, H. T., Zhu, Q. Q., Ji, M., Zhang, H., and Yang, B. X.,, et al. (2021). The prevalence of fatigue among Chinese nursing students in post-COVID-19 era. PeerJ, 9:e11154. doi: 10.7717/peerj.11154
Luberto, C. M., Goodman, J. H., Halvorson, B., Wang, A., and Haramati, A. (2020). Stress and coping Among health professions students During COVID-19: A perspective on the benefits of mindfulness. Global Adv. Health and Med. 9:2164956120977827. doi: 10.1177/2164956120977827
Majumdar, P., Biswas, A., and Sahu, S. (2020). COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 37, 1191–1200. doi: 10.1080/07420528.2020.1786107
Meo, S. A., Abukhalaf, A. A., Alomar, A. A., Sattar, K., and Klonoff, D. C. (2020). Covid-19 pandemic: impact of quarantine on medical students’ mental well-being and learning behaviors. Pakistan J. Med. Sci. 36, S43–S48. doi: 10.12669/pjms.36.COVID19-S4.2809
Michalec, B., Diefenbeck, C., and Mahoney, M. (2013). The calm before the storm? Burnout and compassion fatigue among undergraduate nursing students. Nurse Educ. Today 33, 314–320. doi: 10.1016/j.nedt.2013.01.026
Michielsen, H. J., De Vries, J., and Van Heck, G. L. (2003). Psychometric qualities of a brief self-rated fatigue measure: The fatigue assessment scale. J. Psychosom. Res. 54, 345–352. doi: 10.1016/S0022-3999(02)00392-6
Moloney, W., Boxall, P., Parsons, M., and Cheung, G. (2018). Factors predicting registered Nurses' intentions to leave their organization and profession: A job demands-resources framework. J. Adv. Nurs. 74, 864–875. doi: 10.1111/jan.13497
Morales-Rodríguez, F. M. (2021). Fear, stress, resilience and coping strategies during covid-19 in Spanish university students. Sustain. (Switzerland) 13:5824. doi: 10.3390/su13115824
Nitschke, J. P., Forbes, P. A. G., Ali, N., Cutler, J., Apps, M. A. J., Lockwood, P. L., et al. (2021). Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 26, 553–569. doi: 10.1111/bjhp.12485
Nurhidayati, T., Rahayu, D. A., and Alfiyanti, D. (2021). Nursing students' coping for burnout and fatigue online learning during coronavirus disease 2019 pandemic. Open Access Macedonian J. Med. Sci. 9, 92–96. doi: 10.3889/oamjms.2021.5857
Ran, L., Wang, W., Ai, M., Kong, Y., Chen, J., and Kuang, L. (2020). Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 262:113261. doi: 10.1016/j.socscimed.2020.113261
Roberts, N. J., McAloney-Kocaman, K., Lippiett, K., Ray, E., Welch, L., and Kelly, C. (2021). Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir. Med. 176:106219. doi: 10.1016/j.rmed.2020.106219
Savitsky, B., Findling, Y., Ereli, A., and Hendel, T. (2020). Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ. Pract. 46:102809. doi: 10.1016/j.nepr.2020.102809
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., and Bernard, J. (2008). The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med. 15, 194–200. doi: 10.1080/10705500802222972
Sonika, S., and Kumar, R. (2019). Resilience, psychological well-being, and coping strategies in medical students. Indian J. Psychiatric Nurs. 16:92. doi: 10.4103/iopn.iopn_22_19
Teng, Z., Wei, Z., Qiu, Y., Tan, Y., Chen, J., Tang, H., et al. (2020). Psychological status and fatigue of frontline staff two months after the COVID-19 pandemic outbreak in China: A cross-sectional study. J. Affect. Disord. 275, 247–252. doi: 10.1016/j.jad.2020.06.032
Trendall, J. (2000). Concept analysis: chronic fatigue. J. Adv. Nurs. 32, 1126–1131. doi: 10.1046/j.1365-2648.2000.01583.x
Tsay, S. L., Halstead, M. T., and McCrone, S. (2001). Predictors of coping efficacy, negative moods and post-traumatic stress syndrome following major trauma. Int. J. Nurs. Pract. 7, 74–83. doi: 10.1046/j.1440-172X.2001.00257.x
Tugade, M. M., and Fredrickson, B. L. (2004). Resilient individuals use positive emotions to bounce Back From negative emotional experiences. J. Pers. Soc. Psychol. 86, 320–333. doi: 10.1037/0022-3514.86.2.320
Tull, M. T., Edmonds, K. A., Scamaldo, K. M., Richmond, J. R., Rose, J. P., and Gratz, K. L. (2020). Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 289:113098. doi: 10.1016/j.psychres.2020.113098
Keywords: COVID-19, nursing, students, coping, resilience, fatigue
Citation: Kumar R, Beniwal K and Bahurupi Y (2022) Pandemic Fatigue in Nursing Undergraduates: Role of Individual Resilience and Coping Styles in Health Promotion. Front. Psychol. 13:940544. doi: 10.3389/fpsyg.2022.940544
Edited by:
Alexander V. Libin, MedStar Health Research Institute (MHRI), United StatesReviewed by:
Jose Maria De La Roca-Chiapas, University of Guanajuato, MexicoAna Figueiredo, Pontifical Catholic University of Rio Grande do Sul, Brazil
Copyright © 2022 Kumar, Beniwal and Bahurupi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rajesh Kumar, rajeshrak61@gmail.com
 Rajesh Kumar
Rajesh Kumar Kalpana Beniwal
Kalpana Beniwal Yogesh Bahurupi
Yogesh Bahurupi