Risk Perception of COVID-19 Infection and Adherence to Preventive Measures among Adolescents and Young Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, Procedure
2.2. Measures
- General demographic information including age, gender, ethnicity, education, work status before and during the pandemic, language that the questionnaire was answered in, as well as data on pre-existing chronic diseases or medication.
- Perceived level of information about COVID-19 was measured with a single item (well-informed about COVID-19—yes/no). AYAs also reported which sources they used for COVID-19 related information among social media, broadcasting media, specialized internet resources, conversations with friends/family or others.
- Objective knowledge of COVID-19 manifestations, disease transmission and recommended preventive attitudes were measured using twenty true/false questions, yielding a total knowledge score ranging from 0 to 20, reported as a percentage of correct answers (0–100%).
- Adherence to preventive measures recommended by public health authorities were measured with 4 items (Cronbach’s α = 0.72). AYAs reported how often they washed their hands, avoided group gatherings, reduced unnecessary use of public transportation and avoided public places, using 5-point Likert scales from Never to Always. Participants who answered that they Always followed the four recommendations were classified as having high adherence to preventive measures while others were classified as having low adherence;
- Perception of the risk of becoming a person with COVID-19 was assessed with 2 items (Cronbach’s α = 0.79) in which AYAs reported the perceived risk of COVID-19 infection for themselves and for their family/friends. Responses were given on an 11-point Visual Analog Scale (VAS) from 0 (no risk at all) to 10 (extremely important risk).
- Assessment of factors motivating preventive behaviors included four items (Cronbach’s α = 0.64). Two items related to altruistic motivations: (1) Desire to help to flatten the curve of disease (i.e., reduce the number of new COVID-19 cases); (2) Desire to protect friends/family who are more at risk. Two items were related to personal motives: (3) perceived negative impact on their social life and (4) feeling of not being concerned by COVID-19. All the responses in this section were recorded by a 11-point VAS from 0 (I don’t agree at all) to 10 (I fully agree).
2.3. Data Analysis
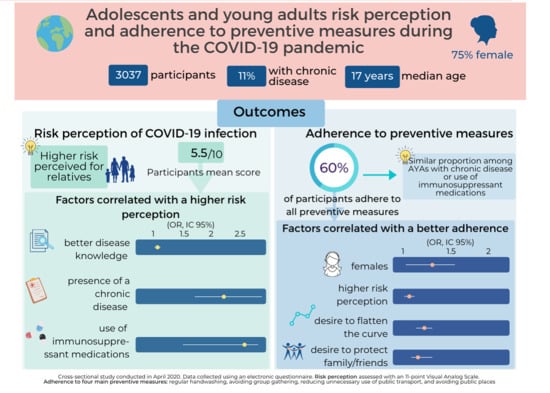
3. Results
3.1. Demogaphic Data
3.2. Objective Knowledge of COVID-19
3.3. Risk Perception
3.4. Adherence of Preventive Measures and Motivators
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiological Characteristics of 2143 Pediatric Patients With 2019 Coronavirus Disease in China. Pediatrics 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.; Zhang, L.; Du, H.; Zhang, J.; Li, Y.Y.; Qu, J.; Zhang, W.; Wang, Y.; Bao, S.; Li, Y.; et al. SARS-CoV-2 Infection in Children. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020. [Google Scholar] [CrossRef]
- Torres, J.P.; Piñera, C.; Maza, V.D.L.; Lagomarcino, A.J.; Simian, D.; Torres, B.; Urquidi, C.; Valenzuela, M.T.; O’Ryan, M. SARS-CoV-2 antibody prevalence in blood in a large school community subject to a Covid-19 outbreak: A cross-sectional study. Clin. Infect. Dis 2020. [Google Scholar] [CrossRef]
- Fontanet, A.; Tondeur, L.; Madec, Y.; Grant, R.; Besombes, C.; Jolly, N.; Pellerin, S.F.; Ungeheuer, M.-N.; Cailleau, I.; Kuhmel, L.; et al. Cluster of COVID-19 in northern France: A retrospective closed cohort study. Medrxiv 2020. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, X.; Zhang, X.; Wei, Z.; Zhang, L.; Xu, J.; Liang, P.; Xu, Y.; Zhang, C.; Xu, A. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J. Infect. 2020, 80, e1–e13. [Google Scholar] [CrossRef]
- Szablewski, C.M.; Chang, K.T.; Brown, M.M.; Chu, V.T.; Yousaf, A.R.; Anyalechi, N.; Aryee, P.A.; Kirking, H.L.; Lumsden, M.; Mayweather, E.; et al. SARS-CoV-2 Transmission and Infection Among Attendees of an Overnight Camp—Georgia, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1023–1025. [Google Scholar] [CrossRef]
- Liao, J.; Fan, S.; Chen, J.; Wu, J.; Xu, S.; Guo, Y.; Li, C.; Zhang, X.; Wu, C.; Mou, H.; et al. Epidemiological and Clinical Characteristics of COVID-19 in Adolescents and Young Adults. Innovation 2020, 1. [Google Scholar] [CrossRef]
- Rashid, H.; Ridda, I.; King, C.; Begun, M.; Tekin, H.; Wood, J.G.; Booy, R. Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatr. Respir. Rev. 2015, 16, 119–126. [Google Scholar] [CrossRef]
- Aerts, C.; Revilla, M.; Duval, L.; Paaijmans, K.; Chandrabose, J.; Cox, H.; Sicuri, E. Understanding the role of disease knowledge and risk perception in shaping preventive behavior for selected vector-borne diseases in Guyana. PLoS Negl. Trop. Dis. 2020, 14, e0008149. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.A.; Klein, W.M.; Persoskie, A.; Avishai-Yitshak, A.; Sheeran, P. The Tripartite Model of Risk Perception (TRIRISK): Distinguishing Deliberative, Affective, and Experiential Components of Perceived Risk. Ann. Behav. Med. 2016, 50, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.A.; Klein, W.M.P.; Avishai, A.; Jones, K.; Villegas, M.; Sheeran, P. When does risk perception predict protection motivation for health threats? A person-by-situation analysis. PLoS ONE 2018, 13, e0191994. [Google Scholar] [CrossRef]
- Kim, J.S.; Choi, J.S. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J. Clin. Nurs. 2016, 25, 2542–2549. [Google Scholar] [CrossRef]
- Reniers, R.L.; Murphy, L.; Lin, A.; Bartolome, S.P.; Wood, S.J. Risk Perception and Risk-Taking Behaviour during Adolescence: The Influence of Personality and Gender. PLoS ONE 2016, 11, e0153842. [Google Scholar] [CrossRef] [Green Version]
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef] [Green Version]
- McFall, S.; Garrinton, C. Life Satisfaction and Material Well-being of Children in the UK. In Early Findings from the First Wave of the UK’s Household Longitudinal Study, 1st ed.; Stephanie, L., McFall, C.G., Eds.; Institute for Social and Economic Research: Colchester, UK, 2011. [Google Scholar]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Shim, E.; Chapman, G.B.; Townsend, J.P.; Galvani, A.P. The influence of altruism on influenza vaccination decisions. J. R. Soc. Interface 2012, 9, 2234–2243. [Google Scholar] [CrossRef] [PubMed]
- Wray-Lake, L.; Maggs, J.L.; Johnston, L.D.; Bachman, J.G.; O’Malley, P.M.; Schulenberg, J.E. Associations between community attachments and adolescent substance use in nationally representative samples. J. Adolesc. Health 2012, 51, 325–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metzger, A.; Alvis, L.M.; Oosterhoff, B.; Babskie, E.; Syvertsen, A.; Wray-Lake, L. The Intersection of Emotional and Sociocognitive Competencies with Civic Engagement in Middle Childhood and Adolescence. J. Youth Adolesc. 2018, 47, 1663–1683. [Google Scholar] [CrossRef]
- Institut de la Statistique du Québec. Portrait Social du Québec; Institut de la Statistique du Québec: Québec, QC, Canada, 2010. [Google Scholar]
- Statistics Canada. Visible Minority of Person. Available online: https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=DEC&Id=45152 (accessed on 11 September 2020).
- Statistics Canada. Census of Population. 2016. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?TABID=2&Lang=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=1341679&GK=0&GRP=1&PID=110531&PRID=10&PTYPE=109445&S=0&SHOWALL=0&SUB=0&Temporal=2017&THEME=120&VID=0&VNAMEE=&VNAMEF=&D1=0&D2=0&D3=0&D4=0&D5=0&D6=0 (accessed on 11 September 2020).
- Bawazir, A.; Al-Mazroo, E.; Jradi, H.; Ahmed, A.; Badri, M. MERS-CoV infection: Mind the public knowledge gap. J. Infect. Public Health 2018, 11, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Seale, H.; McLaws, M.L.; Heywood, A.E.; Ward, K.F.; Lowbridge, C.P.; Van, D.; Gralton, J.; MacIntyre, C.R. The community’s attitude toward swine flu and pandemic influenza. Med. J. Aust. 2009, 191, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Fielding, R.; Lam, W.W.; Ho, E.Y.; Lam, T.H.; Hedley, A.J.; Leung, G.M. Avian influenza risk perception, Hong Kong. Emerg. Infect. Dis. 2005, 11, 677–682. [Google Scholar] [CrossRef]
- Lau, J.T.; Kim, J.H.; Tsui, H.; Griffiths, S. Perceptions related to human avian influenza and their associations with anticipated psychological and behavioral responses at the onset of outbreak in the Hong Kong Chinese general population. Am. J. Infect. Control 2007, 35, 38–49. [Google Scholar] [CrossRef]
- Van den Broucke, S. Why health promotion matters to the COVID-19 pandemic, and vice versa. Health Promot. Int. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarocostas, J. How to fight an infodemic. Lancet 2020, 395, 676. [Google Scholar] [CrossRef]
- Dkhar, S.A.; Quansar, R.; Saleem, S.M.; Khan, S.M.S. Knowledge, attitude, and practices related to COVID-19 pandemic among social media users in J&K, India. Indian J. Public Health 2020, 64, S205–S210. [Google Scholar] [CrossRef]
- Roma, P.; Monaro, M.; Muzi, L.; Colasanti, M.; Ricci, E.; Biondi, S.; Napoli, C.; Ferracuti, S.; Mazza, C. How to Improve Compliance with Protective Health Measures during the COVID-19 Outbreak: Testing a Moderated Mediation Model and Machine Learning Algorithms. Int. J. Environ. Res. Public Health 2020, 17, 7252. [Google Scholar] [CrossRef]
- Montgomery, S.C.; Donnelly, M.; Bhatnagar, P.; Carlin, A.; Kee, F.; Hunter, R.F. Peer social network processes and adolescent health behaviors: A systematic review. Prev. Med. 2019, 130. [Google Scholar] [CrossRef]
- World Health Organization. WHO Strategic Framework for Effective Communications; Department of Communications 20, Avenue Appia CH-1211 Geneva 27 Switzerland; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Calistri, P.; Iannetti, S.; Danzetta, M.L.; Narcisi, V.; Cito, F.; Sabatino, D.D.; Bruno, R.; Sauro, F.; Atzeni, M.; Carvelli, A.; et al. The components of ‘One World—One Health’ approach. Transbound Emerg. Dis. 2013, 60 (Suppl. 2), 4–13. [Google Scholar] [CrossRef] [Green Version]
- Casanova, M.; Pagani Bagliacca, E.; Silva, M.; Patriarca, C.; Veneroni, L.; Clerici, C.A.; Spreafico, F.; Luksch, R.; Terenziani, M.; Meazza, C.; et al. How young patients with cancer perceive the COVID-19 (coronavirus) epidemic in Milan, Italy: Is there room for other fears? Pediatr. Blood Cancer 2020, 67, e28318. [Google Scholar] [CrossRef] [PubMed]

| Total, No. (%) | 3037 (100) |
| Age, median (IQR), years | 17 (15–20) |
| Gender, No. (%) | |
| Male | 740 (24.4) |
| Female | 2266 (74.6) |
| Other | 31 (1.0) |
| Language used to answer the questionnaire, No. (%) | |
| French | 2905 (95.6) |
| English | 132 (4.4) |
| Education, highest diploma obtained, No. (%) | |
| Elementary | 1144 (37.7) |
| Secondary | 1055 (34.7) |
| College | 693 (22.9) |
| University | 137 (4.5) |
| Other | 4 (0.1) |
| None | 4 (0.1) |
| Current school program, No. (%) (n = 1569) b | |
| Natural sciences (Sciences, mathematics, and engineering) | 347 (22.1) |
| Art and social sciences | 639 (40.7) |
| Early childhood care and education | 83 (5.3) |
| Health Sciences | 461 (29.4) |
| Other | 39 (2.5) |
| Ethnicity, No. (%) | |
| Afro-Caribbean | 158 (5.2) |
| Asian | 161 (5.3) |
| Caucasian | 2274 (75.3) |
| Central and South America | 157 (5.2) |
| First Nations | 105 (3.5) |
| Middle East | 154 (5.1) |
| Other | 12 (0.4) |
| Employed before the pandemic (full time or part-time), No. (%) | 1441 (47.4) |
| Current work status, No. (%) (n = 1441) c | |
| Work less | 131 (9.1) |
| Work more | 95 (6.6) |
| Work the same | 310 (21.5) |
| Work from home | 104 (7.2) |
| Stopped working | 801 (55.6) |
| Disease knowledge score, No. (%) d | |
| Under 50% | 10 (0.3) |
| 50–74% | 627 (20.6) |
| 75–89% | 1679 (55.3) |
| More than 90% | 721 (23.7) |
| Know someone with COVID-19, No. (%) | 556 (18.3) |
| Self | 15 (0.5) |
| Family | 165 (5.4) |
| Friends | 258 (8.5) |
| Acquaintance | 139 (4.6) |
| Know someone who died from COVID-19, No. (%) | 54 (1.8) |
| Family | 23 (0.8) |
| Friends | 13 (0.4) |
| Acquaintance | 18 (0.6) |
| Chronic disease, No. (%) | 348 (11.5) |
| Currently taking medication, No. (%) | 255 (8.4) |
| Currently taking Immunosuppressant medication, No. (%) | 105 (3.4) |
| Strictly follow preventive measures, No. (%) e | 1823 (60.0) |
| Risk perception score, mean (DS) | 5.56 (2.6) |
| Adjusted Odds Ratio | 95% Confidence Interval | p Value | |
|---|---|---|---|
| Current school program c | |||
| Early childhood care and education program in college or in university | 1.70 | (1.12–2.59) | 0.01 |
| Disease knowledge score d | 1.06 | (1.01–1.11) | 0.02 |
| Chronic disease | 2.31 | (1.82–2.93) | <0.001 |
| Immunosuppressant medication | 2.53 | (1.67–3.87) | <0.001 |
| Adjusted Odds Ratio | CI (95%) | p Value | |
|---|---|---|---|
| Age | 0.97 | (0.93–1.01) | 0.10 |
| Female gender | 1.29 | (1.08–1.55) | 0.006 |
| Work before pandemic | 0.79 | (0.67–0.93) | 0.004 |
| Current school program c | |||
| Arts and social sciences | 1.55 | (1.21–1.98) | <0.001 |
| Health sciences | 1.86 | (1.40–2.47) | <0.001 |
| Disease knowledge score d | 1.03 | (0.99–1.08) | 0.12 |
| Language used to answer this questionnaire | |||
| French | 1 | 1 | 0.003 |
| English | 1.94 | (1.25–3.02) | |
| Higher perceived risk of COVID-19 infection e | 1.06 | (1.02–1.10) | 0.003 |
| Motivators for taking preventive measures | |||
| To flatten the curve | 1.18 | (1.12–1.25) | <0.001 |
| To protect family and friends | 1.14 | (1.05–1.24) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.Y.; Gong, R.N.; Sassine, S.; Morsa, M.; Tchogna, A.S.; Drouin, O.; Chadi, N.; Jantchou, P. Risk Perception of COVID-19 Infection and Adherence to Preventive Measures among Adolescents and Young Adults. Children 2020, 7, 311. https://doi.org/10.3390/children7120311
Yang XY, Gong RN, Sassine S, Morsa M, Tchogna AS, Drouin O, Chadi N, Jantchou P. Risk Perception of COVID-19 Infection and Adherence to Preventive Measures among Adolescents and Young Adults. Children. 2020; 7(12):311. https://doi.org/10.3390/children7120311
Chicago/Turabian StyleYang, Xin Yu, Rui Ning Gong, Samuel Sassine, Maxime Morsa, Alexandra Sonia Tchogna, Olivier Drouin, Nicholas Chadi, and Prévost Jantchou. 2020. "Risk Perception of COVID-19 Infection and Adherence to Preventive Measures among Adolescents and Young Adults" Children 7, no. 12: 311. https://doi.org/10.3390/children7120311