Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.4969
Peer-review started: January 23, 2021
First decision: February 28, 2021
Revised: March 13, 2021
Accepted: May 15, 2021
Article in press: May 15, 2021
Published online: July 6, 2021
The coronavirus disease 2019 (COVID-19) raging around the world still has not been effectively controlled in most countries and regions. As a severe acute respiratory syndrome coronavirus, in addition to the most common infectious pneumonia, it can also cause digestive system disease such as diarrhea, nausea, vomiting, liver function damage, etc. In medical imaging, it manifests as thickening of the intestinal wall, intestinal perforation, pneumoperitoneum, ascites and decreased liver density. Angiotensin-converting enzyme 2 has great significance in COVID-19-related digestive tract diseases. In this review, we summarized the data on the clinical and imaging manifestations of gastro
Core Tip: There are few reviews on the clinical and radiologic manifestations of gastrointestinal and liver in coronavirus disease 2019 (COVID-19). Here, we review the significant information on the management of patients with COVID-19 and the mechanism of how angiotensin-converting enzyme 2, the key factor of COVID-19 infection, relates to severe acute respiratory syndrome coronavirus 2 with digestive tract symptoms. The potential mechanism of fatty change of the liver is discussed in this review as well.
- Citation: Fang LG, Zhou Q. Remarkable gastrointestinal and liver manifestations of COVID-19: A clinical and radiologic overview. World J Clin Cases 2021; 9(19): 4969-4979
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/4969.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.4969
As of January 4, 2021, over 80 million people have been infected with coronavirus disease 2019 (COVID-19), and more than 1.8 million people have died from diseases caused by this virus[1]. In December 2020, a novel coronavirus mutant named VU-202012/01 appeared in the United Kingdom, and this strain has higher infectiousness[2]. The coronavirus, also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a positive-strand RNA virus that can result in a severe respiratory syndrome in humans[3]. The most common COVID-19 symptoms are fever and cough, while nausea, vomiting, and diarrhea are less common[4]. A deeper understanding of the disease has shown that, in addition to the respiratory system, some infected patients had clinical manifestations in the digestive system, especially in the gastrointestinal (GI) tract and liver[5]. A study by Zhou et al[3] revealed that the COVID-19 virus belongs to the SARS-CoV group. The genome similarity between SARS-COV-2 and SARS-CoV reached 80%, and the similarity between SARS-CoV-2 and bat coronavirus BatCoV RaTG13 reached 96%. It was also confirmed that SARS-CoV-2 uses the same cell entry receptor, angiotensin converting enzyme 2 (ACE2), as SARS-CoV. A study of 1099 patients with COVID-19 revealed that 5% of these patients had nausea or vomiting, and 3.8% of them had diarrhea[4].
At the early stage of the COVID-19 pandemic, the public was not sensitive to the GI and liver lesions related to coronavirus, and the connection and mechanism were not fully explored. With the emergence of more and more relevant cases, studies on the manifestations and pathophysiological mechanism of GI and liver diseases related to coronavirus have become clearer. Therefore, this article focuses on reviewing the clinical and radiologic manifestations of the GI tract and liver in patients with COVID-19.
Although respiratory system symptoms are the most typical and significant manifestation of COVID-19 infection, quite a few patients have presented with digestive symptoms, even as initial symptoms[6].
A fairly comprehensive meta-analysis[7] involving 59254 patients from 11 countries showed that 9% of all included patients had GI symptoms. In addition, a meta-analysis by Cheung et al[8] involving 4243 COVID-19 patients concluded that anorexia was present in a large proportion of patients, and other common symptoms included diarrhea, nausea, vomiting, and abdominal pain or discomfort. Another study of 204 patients with COVID-19 performed by Pan et al[6] showed that 48.5% of these patients presented with digestive symptoms as their chief complaint. Moreover, 7 cases had digestive symptoms without respiratory symptoms. Compared to patients without digestive symptoms, the patients with digestive symptoms presented with anorexia (83.8%), vomiting (0.8%), diarrhea (29.3%), and abdominal pain (0.4%) and had a longer hospitalization time and a worse prognosis.
Sultan et al[9] found that 7.8% of patients had symptoms of nausea or vomiting in their pooled analysis of 5955 patients with COVID-19. Notably, Fang et al[10] found that approximately 22.2% of patients complained of loose stools before the diagnosis of COVID-19, and more than 50% of patients with diarrhea had received or were receiving antiviral treatment. In addition, many patients experienced GI symptoms such as nausea, abdominal pain, and diarrhea during hospitalization or after taking the medication, and these symptoms may also be due to the medication[11]. In addition to the high incidence and most reported GI symptoms, a few rare symptoms such as acute hemorrhagic colitis as well as GI bleeding[6,12] have also been reported.
According to previous studies, it can be concluded that diarrhea is the most common GI manifestation in COVID-19 patients. A study conducted by Xu et al[13] showed that diarrhea occurred in 130 of 355 patients, with a prevalence of 36.6% [95% confidence interval (CI): 31.6%-41.9%). Hajifathalian et al[14] found that diarrhea occurred in 234 of 1059 patients, with a prevalence of 22.1% (95%CI: 19.6%-24.7%). Nausea or vomiting was the second most common symptom. A pooled analysis[9] of 5955 patients with COVID-19 showed a prevalence of nausea or vomiting of 7.8% (95%CI: 7.1%-8.5%) in these patients.
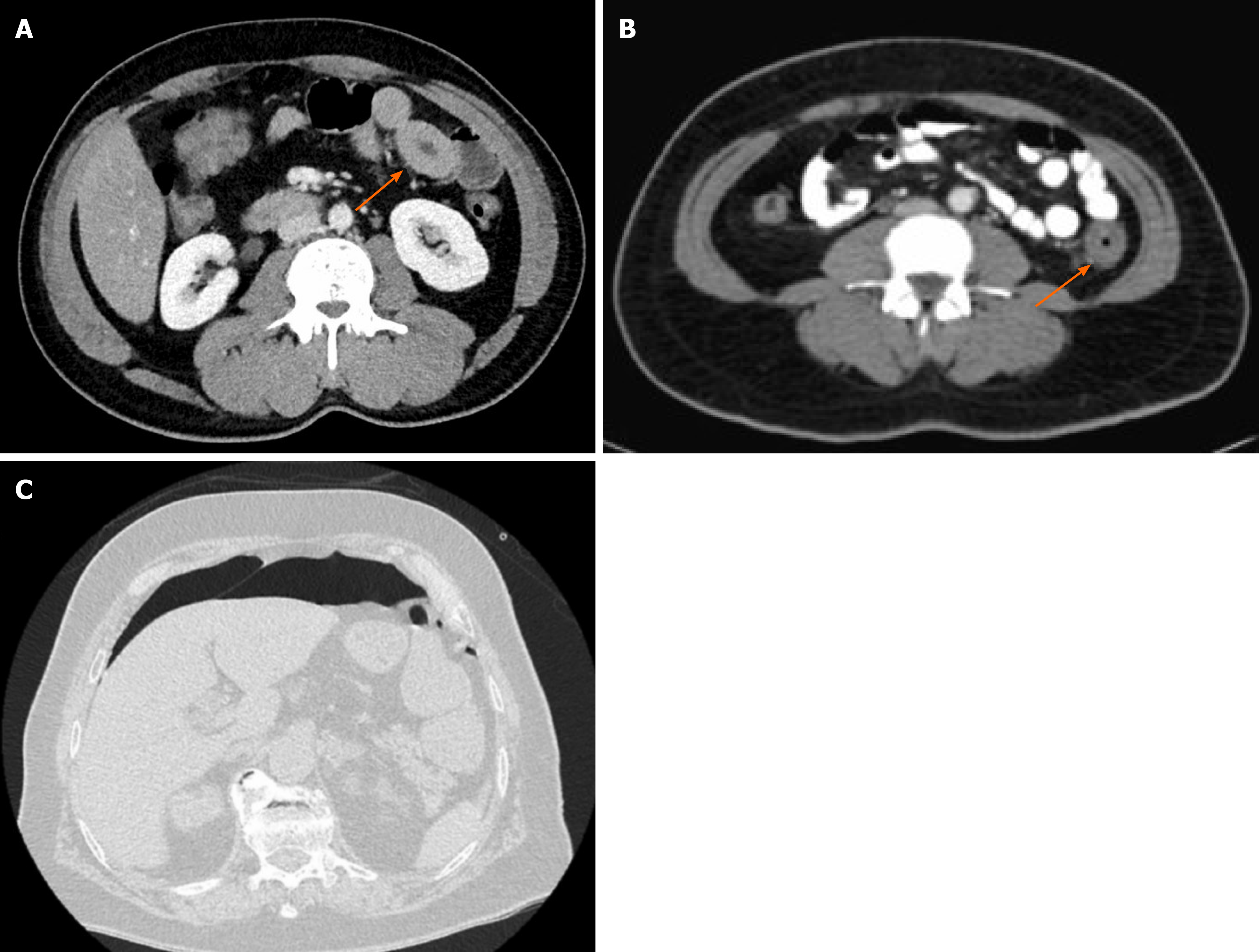
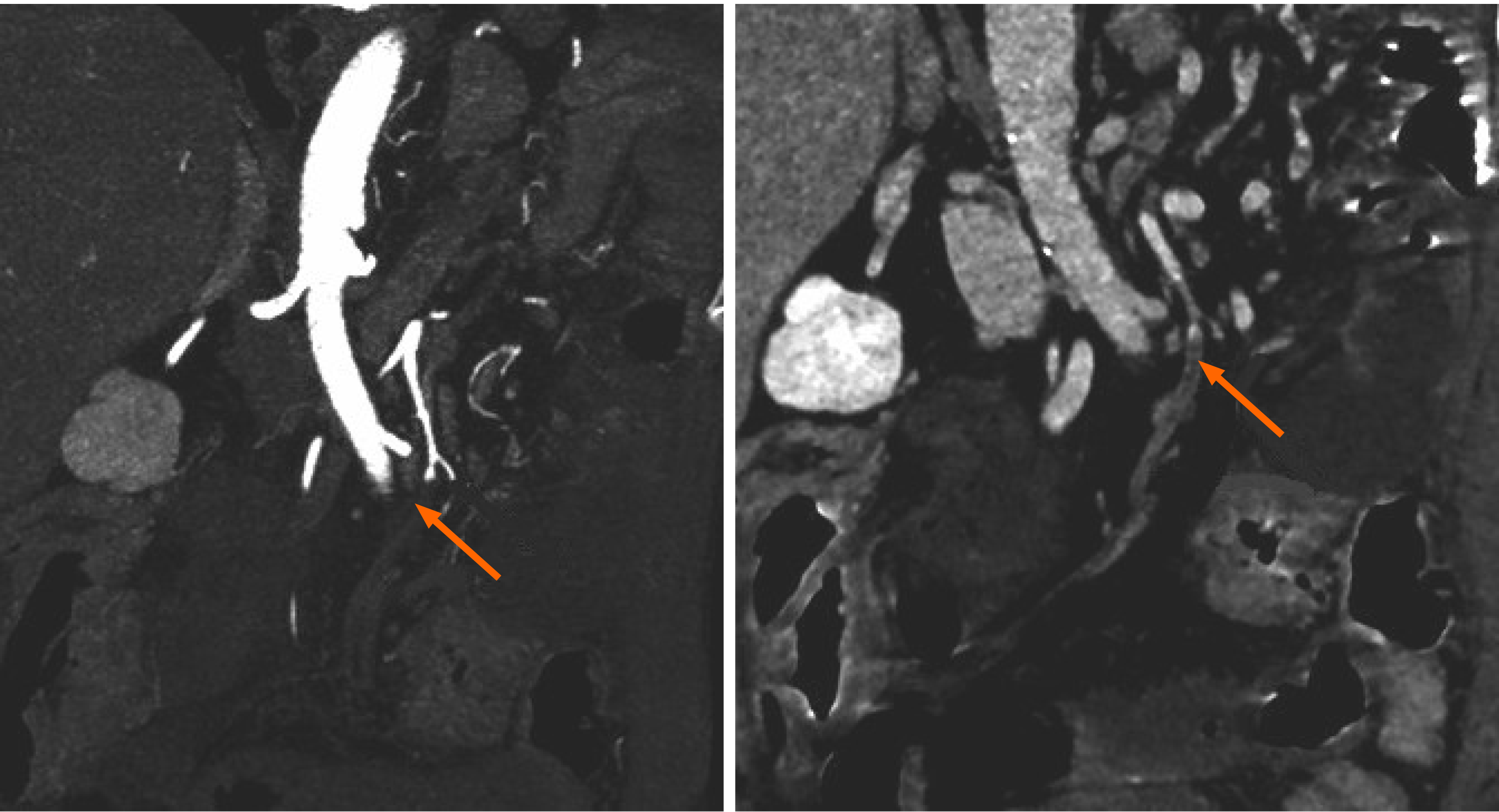
A large number of studies have indicated the pulmonary radiographic features of COVID-19; however, COVID-19-associated GI injury is also seen on imaging. A number of studies[12,15-21] have demonstrated thickening of different areas of the small and large bowel wall. Thickening of the intestinal wall can also be accompanied by hyperemia and thickening of the mesentery. Several case reports have demonstrated a series of GI imaging findings in patients with COVID-19. Funt et al[22] reported a 49-year-old male with COVID-19 infection complaining of left-sided abdominal pain and showed a thick-walled loop of small bowel (arrow) with mild peri-enteric fat stranding in computed tomography (CT) abdominal image; he was finally diagnosed as enteritis (Figure 1A). Another 53-year-old female with COVID-19 infection presented with thick-walled loop of descending colon (arrow) with mild peri-enteric fat stranding in CT image, representing colitis (Figure 1B). One case report[23] involving a COVID-19 infected patient showed extensive pneumoperitoneum caused by perforation of the sigmoid colon on abdominal CT image (Figure 1C). Colonic ileus and intestinal wall pneumatosis were also found on abdominal CT[16,24]. In addition, two separate cases of ileocolic intussusception were detected by ultrasound exami
Research by Bhayana et al[21], which included 42 cases with radiographic images, showed that bowel wall thickening involving the colon or small bowel, intestinal ischemia, ischemia with pneumatosis or portal venous gas and bowel perforation, and a fluid-filled colon were seen in SARS-CoV-2 infected patients. According to these cases, the radiologic manifestations of COVID-19-associated GI disease can present as bowel wall thickening, intussusception, colonic ileus, intestinal wall pneumatosis, and intestinal perforation.
Although GI symptoms are frequently observed, the mechanism of COVID-19-associated GI disease has not been completely elucidated. Therefore, identification of the mechanism of COVID-19 infection is crucial, not just for the treatment of infected patients but for the identification of infected atypical patients. Notably, several possible explanations have been put forward with more and more studies being carried out.
The most frequently proposed mechanism for GI tract injury associated with SARS-CoV-2 is related to the ACE2 cell receptor[29,30]. Hoffmann et al[29] demonstrated that SARS-CoV-2 uses the receptor ACE2 for entry, similar to SARS-CoV. As a principle factor in novel coronavirus, ACE2 is a type I membrane protein expressed in lungs, heart, kidneys, and intestine, and its main physiological function is to promote the maturation of angiotensin[31,32]. Xiao et al[33] found that the ACE2 protein is abundantly expressed in the glandular cells of gastric, duodenal, and rectal epithelia according to immunofluorescent data, which supports the entry of SARS-CoV-2 into the host cells. As a result, both the small and large intestine are susceptible to SARS-CoV-2 infection due to the high expression of ACE2. ACE2 staining is rarely seen in esophageal mucosa, which may be attributed to esophageal epithelium expressing less ACE2 than glandular epithelial cells. It was found that SARS-CoV-2 was expressed not only in lungs, kidneys, and blood vessels but also in the intestine, especially the terminal ileum and colon, and that ACE2 can connect the virus and its target cells, resulting in digestive symptoms[34]. Another study[35] revealed that the interaction between SARS-CoV-2 and ACE2 can disrupt the function of ACE2 and that diarrhea may occur as a manifestation of this functional impairment of ACE2, which is highly expressed in the small intestine, especially in proximal and distal enterocytes.
ACE2 is known to be a cell receptor for SARS-CoV[36]. It is also known that ACE2 controls intestinal inflammation and diarrhea. In the case of SARS-CoV, the spike glycoprotein (S protein) subunit on the virion surface can directly bind to the peptidase domain of ACE2[37] and results in membrane fusion. The S protein of SARS-CoV-2 might infect the host in the same way[3,29,36,38]. As the receptor for SARS-CoV, ACE2 is essential for the expression of neutral amino acid transporters in the gut, and ACE2 can regulate innate immunity and affect the composition of gut microbiota, which may explain why diarrhea and intestinal inflammation occur[39]. Oliveira et al[40] revealed that the ACE2/Ang 1-7 axis can affect the composition of the microbiota by regulating the immune response and is one of the physiological causes of diseases, such as diarrhea and intestinal inflammation. It was found that ACE2 is the key regulator in intestinal inflammation and diarrhea[41]. Furthermore, SARS-CoV-2 may trigger the large-scale release of pro-inflammatory cytokines, such as interleukin-2 and interleukin-7, granulocyte monocyte colony stimulating factor, and tumor necrosis factor alpha, which cause changes in intestinal motility and affect the GI flora, increasing the incidence of diarrhea[42]. The immune response activates the coagulation pathway and leads to the excessive production of pro-inflammatory cytokines, which further leads to multiorgan damage. Thrombin can also increase inflammation through protease-activated receptors[43]. During the course of inflammation, this procoagulant-anticoagulant imbalance easily develops into microth
In addition, another possible mechanism is the “lung-intestine” axis[6,44,45]. Abdominal symptoms can be caused by microbial metabolites and endotoxins that are produced during pneumonia due to the alteration in the gut microbiome. In addition, the adverse effects of antivirals and antibiotics can also induce diarrhea[46].
In conclusion, the main infection mechanism in GI lesions caused by SARS-CoV-2 may be the fusion of SARS-CoV-2 and organs with high expression of ACE2, such as the gastroduodenum, terminal ileum, and rectum, which will destroy the function of ACE2 receptors in the corresponding areas and lead to diarrhea. In addition, the release of a large number of inflammatory factors due to viral infection can lead to corresponding digestive symptoms, including gastroenteritis changes, such as intestinal wall edema and exudation, and intestinal necrosis due to intestinal embolism caused by fibrin clot formation. The “lung-intestine” axis may also be involved in the pathogenesis of COVID-19-associated GI symptoms.
As reported previously, nausea, vomiting, diarrhea, and loss of appetite were the main GI symptoms of patients with COVID-19 infection. More severely, there were previous reports of esophageal bleeding, mesenteric artery embolism, intestinal perforation, and hemorrhagic colitis of patients with COVID-19 infection[12,47]. If not promptly treated, these lesions can eventually lead to shock. Coronavirus-infected patients presenting with GI symptoms had longer duration from illness onset to hospital admission[48].
Almost all the studies on COVID-19-associated liver injuries have revealed abnormal liver function tests such as elevated bilirubin or liver transaminases including alanine transaminase (ALT) and aspartate transaminase (AST). A study by Wang et al[49], which included 69 patients, showed that 23 of these patients had elevated ALT (33%) and 19 had elevated AST (28%) levels. The study by Zhang et al[50] revealed that the incidence of liver injury can reach 78% among patients with confirmed SARS-CoV-2 infection. In addition, Cai et al[51] found that 44 of 298 patients (14.8%) had liver injury, and patients with severe liver injury (36.2%) were more likely to have elevated liver transaminases than those with mild liver injury (9.6%). A retrospective cohort study[52] of 1827 patients with confirmed COVID-19 found that abnormal liver tests were commonly observed (AST 66.9%, ALT 41.6%, alkaline phosphatase 13.5%, total bilirubin 4.3%, albumin 56.7%) on hospital admission. Furthermore, patients with abnormal liver tests were more likely to develop severe COVID-19. Most patients with abnormal liver function tests had minimal elevations pre-hospitalization or at admission, but it was also revealed that patients who received drug treatment (lopinavir/ritonavir, hydroxychloroquine, remdesivir, tocilizumab) experienced more extreme elevations in liver transaminases (> 5 × upper limit of normal) during hospitalization[53]. Of all the COVID-19 patients included in a systematic review[9], the pooled prevalence of abnormally-elevated AST and ALT was 15%, and the combined prevalence of elevated bilirubin was 16.7%.
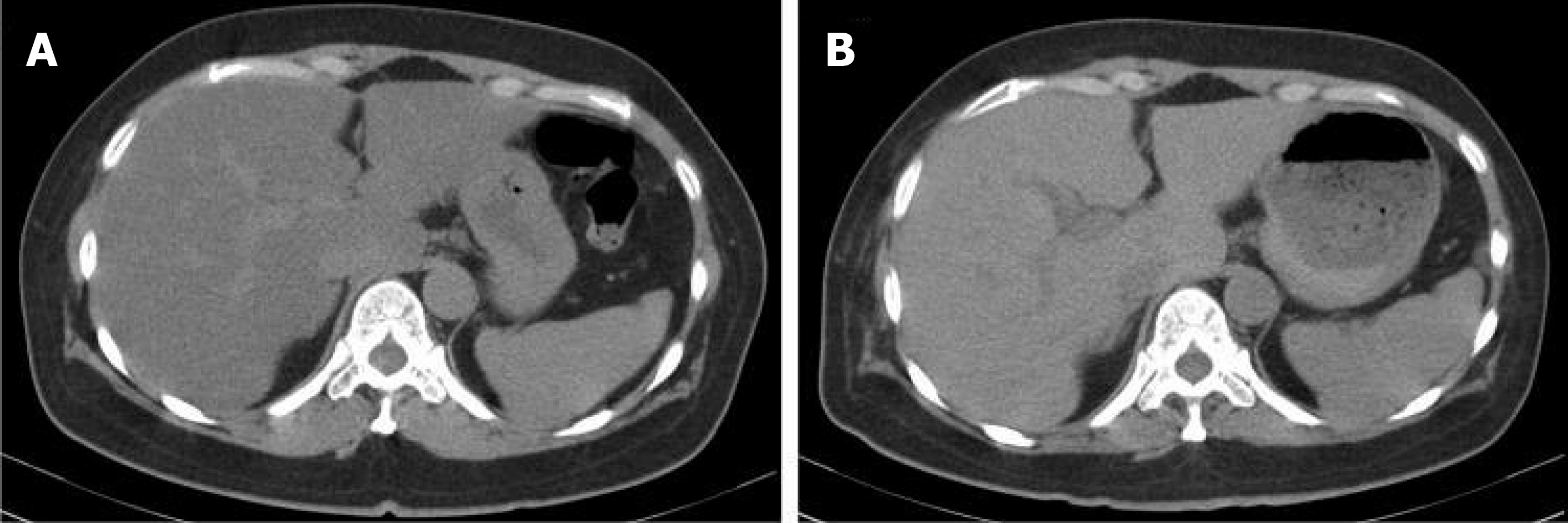
Unfortunately, few studies have investigated the radiographic manifestations of the GI tract and liver of COVID-19 patients. Only a few studies observed cholestasis and hepatocyte steatosis on CT images. Palomar et al[52] found that hepatic steatosis was independently associated with severe COVID-19 pneumonia. A retrospective study[54] of 316 patients revealed that COVID-19 infected individuals had a significantly higher prevalence of steatosis. Uchida et al[55] reported an inpatient 52-year-old woman with COVID-19 infection showing a decreased hepatic CT attenuation value and liver-to-spleen attenuation (L/S) ratio in CT images. The hepatic CT attenuation value and L/S ratio returned to normal level after intensive therapies (Figure 3). It was also found that the results of liver CT images on admission were related to the severity of COVID-19 during hospitalization. Fatty liver and cholestasis were noted on sonographic images in a retrospective cross-sectional study[21] of 412 patients. Pathological studies in COVID-19 showed hepatocellular degeneration with focal necrosis and moderate steatosis in the liver, inflammatory infiltration in the hepatic lobules and portal area, and sinus congestion[56]. CT scans of the upper abdomen usually reveal decreased liver density and fat adhesion around the gallbladder. Homogeneous or heterogeneous low density in the liver is the most common CT manifestation[57]. In addition, the L/S attenuation ratio quantified by CT was measured to indicate the severity of liver damage and indicated a reduced L/S attenuation ratio. Further studies showed that the L/S attenuation ratio and pulmonary lesions were positively correlated with the severity of the disease. Therefore, low liver density and decreased L/S attenuation ratio may be attributable to hepatic steatosis[57]. Furthermore, postmortem liver biopsies in these patients have shown microvesicular steatosis[58].
At present, the mechanism by which SARS-CoV-2 causes liver damage is not fully understood. It is known that the primary viral entry receptor, ACE2, is highly expressed in the liver[9,59]. The pattern of liver injury is primarily hepatocyte injury rather than cholestasis. Expression of the ACE2 receptor in biliary epithelium is 20 times higher than that in hepatocytes[60]. SARS-CoV-2 can directly lead to viral cytopathic lesions with microvesicular steatosis and invasion of hepatic lobules or portal veins through the cytopathic effects of direct immune damage to hepatocytes[56,61]. SARS-CoV-2 can access the biliary system via the portal vein; thus Hundt et al[53] insisted that a direct cytopathic effect by SARS-CoV-2 is probably not the main mechanism of liver damage. This injury may be related to overactivation of Kupffer cells, virus-induced cytotoxic T cell response, and innate immune response that induces regulatory dysregulation[62]. In addition to this, SARS-CoV-2 can also trigger the massive release of pro-inflammatory cytokines, which can exacerbate underlying liver injury[63]. So far, the mechanism of fatty change of the liver has not been certainly discussed.
Potential association between novel coronavirus infection and hepatocyte steatosis may due to the following factors. Firstly, disorganized intestinal flora can increase the absorption of monosaccharides, which in turn promote the synthesis of fatty acids and triglycerides in the liver by increasing the activity of acetyl-CoA carboxylase and fatty acid synthase[64]. Secondly, drugs received by patients with COVID-19 may induce an acute energy crisis by interrupting adenosine triphosphate synthesis by mitochondria, resulting in microvesicular steatosis[65]. Thirdly, ACE2 plays an important role in releasing cytokines produced through the c-Jun N-terminal kinase and inhibitor of nuclear factor κ B kinase-β pathways in COVID-19 patients, which induce insulin resistance and lead to ectopic accumulation of fat in various organs, including the liver[42,66,67].
COVID-19 may do harm to liver and can ultimately result in severe body damage. On one side, it is known that non-alcoholic fatty liver disease is a major cause of liver cirrhosis and hepatocellular carcinoma. On the other side, coronavirus-infected patients with metabolic syndrome and liver steatosis are more likely to develop drug-induced liver injury[68]. In addition, it was revealed that coronavirus-infected patients with chronic liver disease were at a higher risk of prolonged hospitalization and death[69]. Besides, patients complicated with chronic liver disease, decompensated cirrhosis, and hepatocellular carcinoma may be predictors of higher overall mortality during the course of infection[70].
With further knowledge on COVID-19, SARS-CoV-2 has been found to affect the function of the ACE2 cell receptor and the function of the respiratory system and cause digestive system diseases (Table 1). Clinical manifestations of COVID-19 in the GI tract include diarrhea, nausea, vomiting, etc. Radiologic manifestations include intestinal wall thickening, intestinal obstruction, intestinal perforation, pneumoperitoneum, ascites, etc. With regard to liver damage, liver function is impaired, liver enzymes and bilirubin are elevated, and fatty liver changes and cholestasis are observed on CT images. The distribution and high expression of ACE2 receptors in gastric, duodenal, jejunal terminal, colon, and bile duct cells are possibly involved in the pathogenesis of COVID-19. In addition, the inflammatory storm caused by SARS-CoV-2 also increases the risk of diarrhea and causes direct cell damage.
| Ref. | Gastrointestinal clinical manifestations | Gastrointestinal radiologic manifestations | Liver clinical manifestations | Liver radiologic manifestations |
| Pan et al[6] | Anorexia, Vomiting, Diarrhea, Abdominal pain | |||
| Cheung et al[8] | Anorexia, Diarrhea, Nausea, Vomiting, Abdominal pain or discomfort | |||
| Sultan et al[9] | Nausea, Vomiting | Elevated AST and ALT | ||
| Fang et al[10] | Loose stool, Diarrhea | |||
| Pan et al[6], Carvalho et al[12] | Hemorrhagic colitis/GI bleeding | |||
| Xu et al[13] | Diarrhea | |||
| Hajifathalian et al[14] | Diarrhea | |||
| Carvalho et al[12], Guo et al[19], Kim et al[17], Bhayana et al[21], Jaijakul et al[18], Calinescu et al[20], Tang et al[15], Sattar et al[16] | Bowel wall thickening, Hyperemia, Mesenteric thickening | |||
| Corrêa Neto et al[23] | Perforation | |||
| Sattar et al[16], Behzad et al[24] | Colonic ileus, Intestinal wall pneumatosis | |||
| Martínez-Castaño et al[25], Moazzam et al[26] | Ileocolic intussusception | |||
| Culver et al[27] | Ascites | |||
| Bhayana et al[21] | Bowel wall thickening, Cholestasis | Fatty liver, Cholestasis | ||
| Farina et al[28] | Ischemic changes in loops of the small bowel | |||
| Wang et al[49] | Elevated ALT and AST | |||
| Zhang et al[50] | Abnormal ALT and AST | |||
| Cai et al[51] | Abnormal ALT and AST | |||
| Hundt et al[53] | Abnormal liver tests | |||
| Palomar et al[52], Uchida et al[55] | Hepatic steatosis | |||
| Medeiros et al[54] | Steatosis | |||
| Lei et al[57] | Pericholecystic fat stranding, Homogeneous/heterogeneous liver hypodensity |
However, the pathogenesis and radiologic features of COVID-19-associated digestive changes have not been fully determined, impeding diagnostic sensitivity and appropriate treatment. More in-depth and comprehensive studies are necessary to help us understand SARS-CoV-2 infection-related digestive symptoms. Under the circumstance of novel coronavirus mutation, more information is essential to deal with the emergency response more comprehensively and timely.
Manuscript source: Invited manuscript
Specialty type: Infectious Diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shimizu Y, Vetrugno L S-Editor: Wang JL L-Editor: Filipodia P-Editor: Xing YX
| 1. | Johns Hopkins University and Medicine. Johns Hopkins Corona Virus Resource Center (2021) Maps and Trends. Available from: https://coronavirus.jhu.edu/map.html. [Cited in This Article: ] |
| 2. | Wise J. Covid-19: New coronavirus variant is identified in UK. BMJ. 2020;371:m4857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 226] [Cited by in F6Publishing: 202] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 3. | Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15248] [Cited by in F6Publishing: 13132] [Article Influence: 3283.0] [Reference Citation Analysis (0)] |
| 4. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19202] [Cited by in F6Publishing: 17990] [Article Influence: 4497.5] [Reference Citation Analysis (5)] |
| 5. | Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2672] [Cited by in F6Publishing: 2375] [Article Influence: 593.8] [Reference Citation Analysis (2)] |
| 6. | Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, Li P, Hu B, Wang J, Hu C, Jin Y, Niu X, Ping R, Du Y, Li T, Xu G, Hu Q, Tu L. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am J Gastroenterol. 2020;115:766-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1160] [Cited by in F6Publishing: 1137] [Article Influence: 284.3] [Reference Citation Analysis (0)] |
| 7. | Borges do Nascimento IJ, Cacic N, Abdulazeem HM, von Groote TC, Jayarajah U, Weerasekara I, Esfahani MA, Civile VT, Marusic A, Jeroncic A, Carvas Junior N, Pericic TP, Zakarija-Grkovic I, Meirelles Guimarães SM, Luigi Bragazzi N, Bjorklund M, Sofi-Mahmudi A, Altujjar M, Tian M, Arcani DMC, O'Mathúna DP, Marcolino MS. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 305] [Article Influence: 76.3] [Reference Citation Analysis (2)] |
| 8. | Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan KH, Yuen KY, Leung WK. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis. Gastroenterology. 2020;159:81-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1113] [Cited by in F6Publishing: 1046] [Article Influence: 261.5] [Reference Citation Analysis (1)] |
| 9. | Sultan S, Altayar O, Siddique SM, Davitkov P, Feuerstein JD, Lim JK, Falck-Ytter Y, El-Serag HB; AGA Institute. Electronic address: ewilson@gastro.org. AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19. Gastroenterology 2020; 159: 320-334. e27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 283] [Cited by in F6Publishing: 276] [Article Influence: 69.0] [Reference Citation Analysis (1)] |
| 10. | Fang D, Ma JD, Guan JL, Wang MR, Song Y, Tian DA, Li PY. Manifestations of Digestive system in hospitalized patients with novel coronavirus pneumonia in Wuhan, China: a single-center, descriptive study. Zhonghua Xiaohua Zazhi. 2020;40:E005. [Cited in This Article: ] |
| 11. | Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843-851. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 594] [Cited by in F6Publishing: 554] [Article Influence: 138.5] [Reference Citation Analysis (0)] |
| 12. | Carvalho A, Alqusairi R, Adams A, Paul M, Kothari N, Peters S, DeBenedet AT. SARS-CoV-2 Gastrointestinal Infection Causing Hemorrhagic Colitis: Implications for Detection and Transmission of COVID-19 Disease. Am J Gastroenterol. 2020;115:942-946. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 124] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 13. | Xu S, Fu L, Fei J, Xiang HX, Xiang Y, Tan ZX, Li MD, Liu FF, Li Y, Han MF, Li XY, Yu DX, Zhao H, Xu DX. Acute kidney injury at early stage as a negative prognostic indicator of patients with COVID-19: a hospital-based retrospective analysis. 2020 Preprint. Available from: MedRxiv:20042408. [DOI] [Cited in This Article: ] |
| 14. | Hajifathalian K, Krisko T, Mehta A, Kumar S, Schwartz R, Fortune B, Sharaiha RZ; WCM-GI research group. Gastrointestinal and Hepatic Manifestations of 2019 Novel Coronavirus Disease in a Large Cohort of Infected Patients From New York: Clinical Implications. 2020; 159: 1137-1140. Gastroenterology. 2020;159:1137-1149. e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 15. | Tang L, Cheng X, Tian C, Wang R, Zhou H, Wu W, Yan L, Zeng X. Computed tomography (CT) intestinal alterations of Coronavirus Disease 2019 (COVID-19) from the imaging perspective: a case description. Quant Imaging Med Surg. 2020;10:1145-1149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Sattar Y, Connerney M, Rauf H, Saini M, Ullah W, Mamtani S, Syed U, Luddington S, Walfish A. Three Cases of COVID-19 Disease With Colonic Manifestations. Am J Gastroenterol. 2020;115:948-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Kim J, Thomsen T, Sell N, Goldsmith AJ. Abdominal and testicular pain: An atypical presentation of COVID-19. Am J Emerg Med 2020; 38: 1542.e1-1542. e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 18. | Jaijakul S. Colitis as a Sole Presentation of SARS-CoV-2 Infection: Case Report. SN Compr Clin Med. 2020;1-3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Guo Y, Hu X, Yu F, Chen J, Zheng W, Liu J, Zeng P. Abdomen CT findings in a COVID-19 patient with intestinal symptoms and possibly false negative RT-PCR before initial discharge. Quant Imaging Med Surg. 2020;10:1158-1161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Calinescu AM, Vidal I, Grazioli S, Lacroix L, Wildhaber BE. Beware of Too Aggressive Approach in Children With Acute Abdomen During COVID-19 Outbreak! Ann Surg. 2020;272:e244-e245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Catalano O, Gee MS, Hahn PF, Harisinghani M, Kilcoyne A, Lee SI, Mojtahed A, Pandharipande PV, Pierce TT, Rosman DA, Saini S, Samir AE, Simeone JF, Gervais DA, Velmahos G, Misdraji J, Kambadakone A. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology. 2020;297:E207-E215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 217] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 22. | Funt SA, Cohen SL, Wang JJ, Sanelli PC, Barish MA. Abdominal pelvic CT findings compared between COVID-19 positive and COVID-19 negative patients in the emergency department setting. Abdom Radiol (NY). 2021;46:1498-1505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Corrêa Neto IJF, Viana KF, da Silva MBS, da Silva LM, de Oliveira G, de Silva Cecchini AR, Rolim AS, Robles L. Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease. J Coloproctology. 2020;40:269-272. [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 24. | Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin Imaging. 2020;66:35-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 176] [Cited by in F6Publishing: 172] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 25. | Martínez-Castaño I, Calabuig-Barbero E, Gonzálvez-Piñera J, López-Ayala JM. COVID-19 Infection Is a Diagnostic Challenge in Infants With Ileocecal Intussusception. Pediatr Emerg Care. 2020;36:e368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 26. | Moazzam Z, Salim A, Ashraf A, Jehan F, Arshad M. Intussusception in an infant as a manifestation of COVID-19. J Pediatr Surg Case Rep. 2020;59:101533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 27. | Culver A, Arbelot C, Bechis C, Cassir N, Leone M. First description of SARS-CoV-2 in ascites. IDCases. 2020;21:e00836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Farina D, Rondi P, Botturi E, Renzulli M, Borghesi A, Guelfi D, Ravanelli M. Gastrointestinal: Bowel ischemia in a suspected coronavirus disease (COVID-19) patient. J Gastroenterol Hepatol. 2021;36:41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020; 181: 271-280. e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11946] [Cited by in F6Publishing: 13051] [Article Influence: 3262.8] [Reference Citation Analysis (0)] |
| 30. | Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444-1448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3274] [Cited by in F6Publishing: 3410] [Article Influence: 852.5] [Reference Citation Analysis (0)] |
| 31. | Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, Donovan M, Woolf B, Robison K, Jeyaseelan R, Breitbart RE, Acton S. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. Circ Res. 2000;87:E1-E9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2045] [Cited by in F6Publishing: 2084] [Article Influence: 86.8] [Reference Citation Analysis (0)] |
| 32. | Qi F, Qian S, Zhang S, Zhang Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun. 2020;526:135-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 523] [Cited by in F6Publishing: 692] [Article Influence: 173.0] [Reference Citation Analysis (0)] |
| 33. | Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-1833. e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1985] [Cited by in F6Publishing: 1900] [Article Influence: 475.0] [Reference Citation Analysis (1)] |
| 34. | Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 585] [Cited by in F6Publishing: 627] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 35. | Lee IC, Huo TI, Huang YH. Gastrointestinal and liver manifestations in patients with COVID-19. J Chin Med Assoc. 2020;83:521-523. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 126] [Article Influence: 31.5] [Reference Citation Analysis (2)] |
| 36. | Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC, Choe H, Farzan M. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450-454. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4113] [Cited by in F6Publishing: 4359] [Article Influence: 207.6] [Reference Citation Analysis (0)] |
| 37. | Li F, Li W, Farzan M, Harrison SC. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309:1864-1868. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1488] [Cited by in F6Publishing: 1483] [Article Influence: 78.1] [Reference Citation Analysis (0)] |
| 38. | Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W, Bao L, Zhang B, Liu G, Wang Z, Chappell M, Liu Y, Zheng D, Leibbrandt A, Wada T, Slutsky AS, Liu D, Qin C, Jiang C, Penninger JM. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875-879. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2710] [Cited by in F6Publishing: 2536] [Article Influence: 133.5] [Reference Citation Analysis (0)] |
| 39. | Perlot T, Penninger JM. ACE2 - from the renin-angiotensin system to gut microbiota and malnutrition. Microbes Infect. 2013;15:866-873. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 164] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 40. | Oliveira Andrade JM, de Farias Lelis D, Mafra V, Cota J. The Angiotensin Converting Enzyme 2 (ACE2), Gut Microbiota, and Cardiovascular Health. Protein Pept Lett. 2017;24:827-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Hashimoto T, Perlot T, Rehman A, Trichereau J, Ishiguro H, Paolino M, Sigl V, Hanada T, Hanada R, Lipinski S, Wild B, Camargo SM, Singer D, Richter A, Kuba K, Fukamizu A, Schreiber S, Clevers H, Verrey F, Rosenstiel P, Penninger JM. ACE2 Links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487:477-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 787] [Cited by in F6Publishing: 895] [Article Influence: 74.6] [Reference Citation Analysis (0)] |
| 42. | Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020;8:e46-e47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 789] [Cited by in F6Publishing: 828] [Article Influence: 207.0] [Reference Citation Analysis (0)] |
| 43. | José RJ, Williams AE, Chambers RC. Proteinase-activated receptors in fibroproliferative lung disease. Thorax. 2014;69:190-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 44. | Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, Hansbro PM. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017;15:55-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 622] [Cited by in F6Publishing: 798] [Article Influence: 99.8] [Reference Citation Analysis (0)] |
| 45. | Dhar D, Mohanty A. Gut microbiota and Covid-19- possible link and implications. Virus Res. 2020;285:198018. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 330] [Cited by in F6Publishing: 364] [Article Influence: 91.0] [Reference Citation Analysis (0)] |
| 46. | Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, Wu Y, Xiao W, Liu S, Chen E, Chen W, Wang X, Yang J, Lin J, Zhao Q, Yan Y, Xie Z, Li D, Yang Y, Liu L, Qu J, Ning G, Shi G, Xie Q. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020;369:m1849. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 623] [Cited by in F6Publishing: 638] [Article Influence: 159.5] [Reference Citation Analysis (1)] |
| 47. | Lin L, Jiang X, Zhang Z, Huang S, Fang Z, Gu Z, Gao L, Shi H, Mai L, Liu Y, Lin X, Lai R, Yan Z, Li X, Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997-1001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 630] [Cited by in F6Publishing: 617] [Article Influence: 154.3] [Reference Citation Analysis (0)] |
| 48. | Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC, Ghosh S, Chen MH. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667-678. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 741] [Cited by in F6Publishing: 692] [Article Influence: 173.0] [Reference Citation Analysis (0)] |
| 49. | Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical Features of 69 Cases With Coronavirus Disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:769-777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 557] [Cited by in F6Publishing: 676] [Article Influence: 169.0] [Reference Citation Analysis (0)] |
| 50. | Zhang B, Zhou X, Qiu Y, Song Y, Feng F, Feng J, Song Q, Jia Q, Wang J. Clinical characteristics of 82 cases of death from COVID-19. PLoS One. 2020;15:e0235458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 269] [Cited by in F6Publishing: 305] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 51. | Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, Su Y, Ma Z, Zhang Y, Li Z, He Q, Liu L, Fu Y, Chen J. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75:1742-1752. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 252] [Cited by in F6Publishing: 323] [Article Influence: 80.8] [Reference Citation Analysis (0)] |
| 52. | Palomar-Lever A, Barraza G, Galicia-Alba J, Echeverri-Bolaños M, Escarria-Panesso R, Padua-Barrios J, Halabe-Cherem J, Hernandez-Molina G, Chargoy-Loustaunau TN, Kimura-Hayama E. Hepatic steatosis as an independent risk factor for severe disease in patients with COVID-19: A computed tomography study. JGH Open. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 53. | Hundt MA, Deng Y, Ciarleglio MM, Nathanson MH, Lim JK. Abnormal Liver Tests in COVID-19: A Retrospective Observational Cohort Study of 1,827 Patients in a Major U.S. Hospital Network. Hepatology. 2020;72:1169-1176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 167] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 54. | Medeiros AK, Barbisan CC, Cruz IR, de Araújo EM, Libânio BB, Albuquerque KS, Torres US. Higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol (NY). 2020;45:2748-2754. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 55. | Uchida Y, Uemura H, Yamaba S, Hamada D, Tarumoto N, Maesaki S, Mochida S. Significance of liver dysfunction associated with decreased hepatic CT attenuation values in Japanese patients with severe COVID-19. J Gastroenterol. 2020;55:1098-1106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5228] [Cited by in F6Publishing: 5526] [Article Influence: 1381.5] [Reference Citation Analysis (2)] |
| 57. | Lei P, Zhang L, Han P, Zheng C, Tong Q, Shang H, Yang F, Hu Y, Li X, Song Y. Liver injury in patients with COVID-19: clinical profiles, CT findings, the correlation of the severity with liver injury. Hepatol Int. 2020;14:733-742. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 58. | Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, Lau G. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol. 2020;73:451-453. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 336] [Cited by in F6Publishing: 377] [Article Influence: 94.3] [Reference Citation Analysis (2)] |
| 59. | Xu L, Liu J, Lu M, Yang D, Zheng X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020;40:998-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 558] [Cited by in F6Publishing: 536] [Article Influence: 134.0] [Reference Citation Analysis (0)] |
| 60. | Perisetti A, Gajendran M, Mann R, Elhanafi S, Goyal H. COVID-19 extrapulmonary illness - special gastrointestinal and hepatic considerations. Dis Mon. 2020;66:101064. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 61. | Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;40:2095-2103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 293] [Cited by in F6Publishing: 317] [Article Influence: 79.3] [Reference Citation Analysis (0)] |
| 62. | Bangash MN, Patel J, Parekh D. COVID-19 and the liver: little cause for concern. Lancet Gastroenterol Hepatol. 2020;5:529-530. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 272] [Cited by in F6Publishing: 338] [Article Influence: 84.5] [Reference Citation Analysis (0)] |
| 63. | Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1184] [Cited by in F6Publishing: 1219] [Article Influence: 304.8] [Reference Citation Analysis (4)] |
| 64. | Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA. 2004;101:15718-15723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3967] [Cited by in F6Publishing: 4110] [Article Influence: 205.5] [Reference Citation Analysis (4)] |
| 65. | Dash A, Figler RA, Sanyal AJ, Wamhoff BR. Drug-induced steatohepatitis. Expert Opin Drug Metab Toxicol. 2017;13:193-204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 66. | Gao Z, Hwang D, Bataille F, Lefevre M, York D, Quon MJ, Ye J. Serine phosphorylation of insulin receptor substrate 1 by inhibitor kappa B kinase complex. J Biol Chem. 2002;277:48115-48121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 558] [Cited by in F6Publishing: 533] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 67. | Ozes ON, Akca H, Mayo LD, Gustin JA, Maehama T, Dixon JE, Donner DB. A phosphatidylinositol 3-kinase/Akt/mTOR pathway mediates and PTEN antagonizes tumor necrosis factor inhibition of insulin signaling through insulin receptor substrate-1. Proc Natl Acad Sci USA. 2001;98:4640-4645. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 292] [Cited by in F6Publishing: 306] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 68. | Boeckmans J, Rodrigues RM, Demuyser T, Piérard D, Vanhaecke T, Rogiers V. COVID-19 and drug-induced liver injury: a problem of plenty or a petty point? Arch Toxicol. 2020;94:1367-1369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 69. | Singh S, Khan A. Clinical Characteristics and Outcomes of Coronavirus Disease 2019 Among Patients With Preexisting Liver Disease in the United States: A Multicenter Research Network Study. Gastroenterology 2020; 159: 768-771. e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 205] [Cited by in F6Publishing: 248] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 70. | Kim D, Adeniji N, Latt N, Kumar S, Bloom PP, Aby ES, Perumalswami P, Roytman M, Li M, Vogel AS, Catana AM, Wegermann K, Carr RM, Aloman C, Chen V, Rabiee A, Sadowski B, Nguyen V, Dunn W, Chavin K, Zhou K, Lizaola-Mayo B, Moghe A, Debes J, Lee TH, Branch A, Viveiros K, Chan W, Chascsa D, Kwo P, Dhanasekaran R. Predictors of Outcomes of COVID-19 in Patients with Chronic Liver Disease: US Multi-center Study. Clin Gastroenterol Hepatol. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 158] [Article Influence: 52.7] [Reference Citation Analysis (0)] |