Obesity and Impaired Metabolic Health Increase Risk of COVID-19-Related Mortality in Young and Middle-Aged Adults to the Level Observed in Older People: The LEOSS Registry
- 1Institute of Diabetes Research and Metabolic Diseases (IDM) of the Helmholtz Center Munich, Tübingen, Germany
- 2Department of Internal Medicine IV, University Hospital of Tübingen, Tübingen, Germany
- 3German Center for Diabetes Research (DZD), Munich, Germany
- 4Department of Internal Medicine I, Faculty of Medicine, University Hospital Cologne, Cologne, University of Cologne, Cologne, Germany
- 5German Center for Infection Research (DZIF), Partner-Site Bonn-Cologne, Cologne, Germany
- 6Department of Internal Medicine II, School of Medicine, University Hospital Rechts der Isar, Technical University of Munich, Munich, Germany
- 7Department of Internal Medicine, Infectious Diseases, University Hospital Frankfurt, Goethe University Frankfurt, Frankfurt am Main, Germany
- 8Department of Infectious Diseases and Infection Control, Ingolstadt Hospital, Ingolstadt, Germany
- 9Department of Internal Medicine II, University Hospital Jena, Jena, Germany
- 10Emergency Department, University Hospital Regensburg, Regensburg, Germany
- 11Department of Internal Medicine I, Passau Hospital, Passau, Germany
- 12Department of Internal Medicine I, Hospital Bremen-Center, Bremen, Germany
- 13Department for Pneumology, Infectiology, Internal Medicine and Intensive Care, gGmbH, Dortmund, Germany
- 14Division of Cardiology, Hospital Maria Hilf Mönchengladbach, Mönchengladbach, Germany
- 15University Clinic for Hematology, Oncology, Hemostaseology and Palliative Care, University of Bochum, Minden, Germany
- 16Internal Medicine III - Gastroenterology and Infectious Diseases, University Hospital of Augsburg, Augsburg, Germany
- 17Department of Internal Medicine, Hematology and Oncology, University Hospital Cologne, Goethe University Frankfurt, Frankfurt am Main, Germany
- 18Helmholtz Center Munich, Faculty of Medicine, Paul Langerhans Institute Dresden, University Hospital, Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 19Department of Endocrinology and Diabetology, Medical Faculty and University Hospital, Heinrich-Heine University, Düsseldorf, Germany
- 20Institute for Clinical Diabetology, German Diabetes Center, Leibniz Center for Diabetes Research at Heinrich- Heine University, Düsseldorf, Germany
- 21Department of Experimental Diabetology, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany
- 22Institute of Experimental Genetics, Helmholtz Zentrum München, Oberschleißheim, Germany
- 23TUM School of Life Sciences (SoLS), Chair of Experimental Genetics, Technische Universität München, Freising, Germany
- 24New Balance Foundation Obesity Prevention Center, Boston Children's Hospital, Boston, MA, United States
- 25Department of Pediatrics, Harvard Medical School, Boston, MA, United States
- 26Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 27Department of Molecular Epidemiology, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany
- 28Department of Gastroenterology, Hepatology and Infectious Diseases, Medical Faculty and University Hospital Düsseldorf, Heinrich Heine University Düsseldorf, Düsseldorf, Germany
Advanced age, followed by male sex, by far poses the greatest risk for severe COVID-19. An unresolved question is the extent to which modifiable comorbidities increase the risk of COVID-19-related mortality among younger patients, in whom COVID-19-related hospitalization strongly increased in 2021. A total of 3,163 patients with SARS-COV-2 diagnosis in the Lean European Open Survey on SARS-CoV-2-Infected Patients (LEOSS) cohort were studied. LEOSS is a European non-interventional multi-center cohort study established in March 2020 to investigate the epidemiology and clinical course of SARS-CoV-2 infection. Data from hospitalized patients and those who received ambulatory care, with a positive SARS-CoV-2 test, were included in the study. An additive effect of obesity, diabetes and hypertension on the risk of mortality was observed, which was particularly strong in young and middle-aged patients. Compared to young and middle-aged (18–55 years) patients without obesity, diabetes and hypertension (non-obese and metabolically healthy; n = 593), young and middle-aged adult patients with all three risk parameters (obese and metabolically unhealthy; n = 31) had a similar adjusted increased risk of mortality [OR 7.42 (95% CI 1.55–27.3)] as older (56–75 years) non-obese and metabolically healthy patients [n = 339; OR 8.21 (95% CI 4.10–18.3)]. Furthermore, increased CRP levels explained part of the elevated risk of COVID-19-related mortality with age, specifically in the absence of obesity and impaired metabolic health. In conclusion, the modifiable risk factors obesity, diabetes and hypertension increase the risk of COVID-19-related mortality in young and middle-aged patients to the level of risk observed in advanced age.
Introduction
As of 14 February 2022, more than 404 million people worldwide have been infected with SARS-CoV-2, resulting in more than 5.7 million deaths (1). Early in the SARS-CoV-2 pandemic, older age was identified as the strongest risk factor for COVID-19-related mortality. Furthermore, male sex and several comorbidities were found to be associated with an increased risk of mortality in patients with COVID-19 (2–4). Obesity and hyperglycemia in the non-diabetic range were additionally identified as potential risk factors for COVID-19 morbidity and mortality (5–9). Of note, these relationships were independent of age, sex and other comorbidities (10–14). Consequently, obesity and impaired metabolic health are now viewed as important modifiable risk factors for disease severity (15–17).
However, recently, in a large, international, multicenter study from 18 sites in 11 countries, of 7,244 patients hospitalized with COVID-19, obesity and diabetes were found to associate with increased adjusted odds of supplemental oxygen/non-invasive ventilatory support, yet, not with mortality (18). Furthermore, in a very large community-based cohort study from the United Kingdom that evaluated data from 6,910,695 patients with a positive SARS-CoV-2 test result, obesity strongly associated with mortality in the younger and middle-aged adults, but not in the older patients (19). Unfortunately, in that study no adjustment for comorbidities could be done. Thus, it is important to clarify whether obesity and other metabolic comorbidities may increase the risk of COVID-19-related mortality, independently of other diseases, specifically in younger and middle-aged patients.
These patients with COVID-19 are generally considered to have substantially lower risk of COVID-19-related mortality, than those older than 65 years. However, risk in younger age groups has become increasingly relevant, with initially selective vaccination of older individuals and rapidly rising incidence of infection and hospitalization among children, adolescents, and young adults (20). Data from the US Centers for Disease Control and Prevention (CDC) suggests that a 35-year-old with diabetes mellitus, hypertension, cardiovascular disease, obesity, or other chronic conditions had a similar risk of COVID-19-related death as a 65-year-old with none of these conditions (21). Furthermore, in an analysis of data from an US Premier Healthcare Database of hospital-based patients with COVID-19, younger patients (age 18–34 years) with morbid obesity, hypertension, and diabetes faced similar risk of death or need for mechanical ventilation, as that observed in middle-aged (age 35–64 years) adults (22). However, these did not consider potential confounding, and in the CDC report no information about comorbidities was available in 22% of the patients (21). Adjustment for sex and other comorbidities, such as cardiovascular, renal and liver disease, is essential, as these comorbidities are strongly related to impaired metabolic health.
To clarify the potential impact of obesity and impaired metabolic health on COVID-19 related mortality in younger adults, we have studied the determinants of COVID-19-related mortality in 3,163 patients with COVID-19 of the Lean European Open Survey on SARS-CoV-2-Infected Patients (LEOSS) cohort study.
Research Design and Methods
Study Design and Patient Cohort
A total of 6,457 consecutive patients, who were included in the LEOSS registry between March 2020 and February 2021, were evaluated. LEOSS is a European non-interventional multi-center cohort study established in March 2020 to address the lack of information on the epidemiology and clinical course of SARS-CoV-2 infection (23, 24). The registry collects data on hospitalized patients of all ages and patients who receive ambulatory medical consultation. As of July 2020, more than 125 sites from 7 different countries have been registered to LEOSS. Daily statistics are provided on the LEOSS website (https://leoss.net). To facilitate the rapid data acquisition needed during a pandemic, LEOSS involves autonomous, self-managed study sites that collect data in an anonymous form. To achieve this, no directly identifying data are stored in the registry and demographic data as well as timestamps are only collected in a rough form. Furthermore, data were documented categorically. Patient privacy was additional protected using the anonymization procedures described by Jakob et al. (24). Data collection is performed once per case, retrospectively after treatment has finished or the patient has died. Although this method precludes longitudinal data collection and follow-up of discharged patients, it has the advantage that no informed consent is necessary. Furthermore, this method provides for the inclusion of data on children and unconscious or deceased patients and avoids problems that could arise from language barriers. All patients had a diagnosis confirmed by positive results of PCR testing. Approval for LEOSS was obtained by the applicable local ethics committees of all participating centers and registered at the German Clinical Trails Register (DRKS, No. S00021145).
Clinical Data and Outcomes
Data were recorded in an electronic case report form operated using the online cohort platform ClinicalSurveys.net, which was developed by the University Hospital of Cologne (UHC), Germany. ClinicalSurveys.net was hosted by QuestBack, Oslo, Norway on servers of UHC, Cologne, as part of a software-as-a-service agreement. Baseline data closest to the first positive SARS-CoV-2 test were analyzed. Demographic, clinical, laboratory and outcome data were extracted from the in-hospital medical records. Operational definitions of the co-morbidities studied are based on the medical diagnosis guidelines that were applied by the treating physicians in the hospital. Diagnosis were either pre-known or newly made by the treating physicians based on the clinical in-hospital evaluation and/or laboratory results. Analyzed laboratory data were collected within 48 h of a positive SARS-CoV-2 PCR result, irrespective of the patient's status. Among the 6,457 patients evaluated only adult (age ≥18 years) patients who had complete information about sex, age, BMI and the comorbidities diabetes, hypertension, coronary artery disease, chronic kidney disease and chronic liver disease (N = 3,517) were considered eligible for the analyses. Among them, a total of 354 patients with missing information on survival were excluded, yielding a sample of 3,163 for the main analyses (Supplementary Figure 1).
Comorbidities were dichotomized (e.g., diabetes present/absent, coronary artery disease present/absent). Comorbidities were set to unknown/missing when all specific comorbidities of one group were unknown or missing. Values documented as unknown were defined as missing. Besides sex, age, BMI and the above-mentioned comorbidities, the following clinical parameters related to metabolic risk, which were not available in all patients, were evaluated: hemoglobin A1c (HbA1c), serum creatinine, serum C-reactive protein (CRP), serum interleukin-6 (IL-6), serum alanine aminotransferase (ALT), serum aspartate aminotransferase (AST), serum gamma-glutamyl transferase (GGT), as well as urine ketone bodies. Clinical parameters were set to unknown/missing if not available. The primary outcome was COVID-19-related mortality. In an exploratory approach disease severity, which is not a hard endpoint, was also studied (uncomplicated phase: patients were either asymptomatic, and had symptoms of upper respiratory tract infection, fever or nausea, emesis, or diarrhea; complicated phase: patients had at least one of the characteristics new need for oxygen supplementation or clinically relevant increase of prior oxygen home therapy, PaO2 at room air < 70 mmHg, SO2 at room air < 90%, increase of AST or ALT > 5 × upper limit of normal, new cardiac arrythmia, new pericardial effusion > 1 cm or new heart failure with pulmonary edema, congestive hepatopathy, or peripheral edema; critical phase patients were dependent on catecholamines, experienced life-threatening cardiac arrhythmia, had mechanical ventilation (invasive or non-invasive), or need for unplanned mechanical ventilation prolongation (> 24 h) of planned mechanical ventilation, liver failure with an INR > 3.5 (quick < 50%), a qSOFA score of > = 2, or acute renal failure with need of dialysis).
Statistical Analyses
We calculated and report patient characteristics as absolute numbers and percentages. For comparison of percentages between groups the χ2-test was used. The odds ratios of baseline characteristics, comorbidities and laboratory parameters, with mortality were assessed in univariate and in multivariable logistic regression models. Univariate and multivariable relationships of baseline characteristics with mortality were also assessed after patients were stratified in young and middle aged (18–55 years; n = 1,068), older age (56–75 years; n = 1,220) and old age (>75 years; n = 875) groups. Then patients in each age group were further categorized by the presence or absence of obesity, of obesity+diabetes and of obesity+diabetes+hypertension. For the main analyses, patients in the three age groups were subdivided into those (i) without obesity (BMI <30 kg·m−2) and without impaired metabolic health (no diabetes and no hypertension, n = 1,098) and in those (ii) having all three risk factors (BMI ≥30 kg·m−2, diabetes and hypertension, n = 259). Kaplan-Meier analyses were used to compare the survival of the patients among these six subgroups. A p < 0.05 was considered to indicate statistical significance. Data management, statistical analysis, and computation of figures were conducted using R (R Development Core Team, Vienna, Austria, Version 3.5.2., 2019). Additional information about the LEOSS questionnaire can be found under https://leoss.net/.
Results
Among the 3,163 patients included in the analyses, data were collected primarily from Germany (N = 95%), as well as from Turkey, Belgium, Switzerland, Spain, Austria, Italy, Bosnia and Herzegovina, United Kingdom and Latvia. A total of 2,989 from 3,144 patients (19 patients with missing information) had an inpatient stay. Disease course was classified as uncomplicated (N = 1,284) complicated (N = 1,130) and critical (N = 749) (24). From the 3,163 patients studied, 2,661 patients recovered from the disease while 502 patients died (Supplementary Table 1).
Univariable and Multivariable Relationships of Patient Characteristics With Mortality
In univariable analyses, among the parameters age, sex, BMI, comorbidities and selected laboratory variables, determined at the day of SARS-COV-2 diagnosis, higher age, male sex, diabetes, hypertension, HbA1c >10%, coronary artery disease, chronic liver disease and liver cirrhosis were associated with an increased risk of mortality (Supplementary Table 2). In a multivariable regression model including all studied parameters, higher age, male sex, BMI ≥35 kg·m−2, diabetes, HbA1c >8.1%, CRP ≥30 mg/L and GGT >10 upper limit of normal were independently associated with an increased risk of mortality (Supplementary Table 3).
To avoid over-adjustment in the statistical models by including variables that are highly related to each other, e.g., the diagnosis of liver cirrhosis and elevated transaminases or chronic kidney disease and elevated serum creatinine, we further focused in the multivariate regression models on the parameters reported in the Table 1. In that parsimonious multivariable regression model higher age, male sex, BMI ≥ 35 kg·m−2, HbA1c >10%, chronic kidney disease and liver cirrhosis were independently associated with an increased risk of mortality. The association with hypertension was borderline, with an adjusted p-value of 0.056 (Table 1, Supplementary Figure 2).
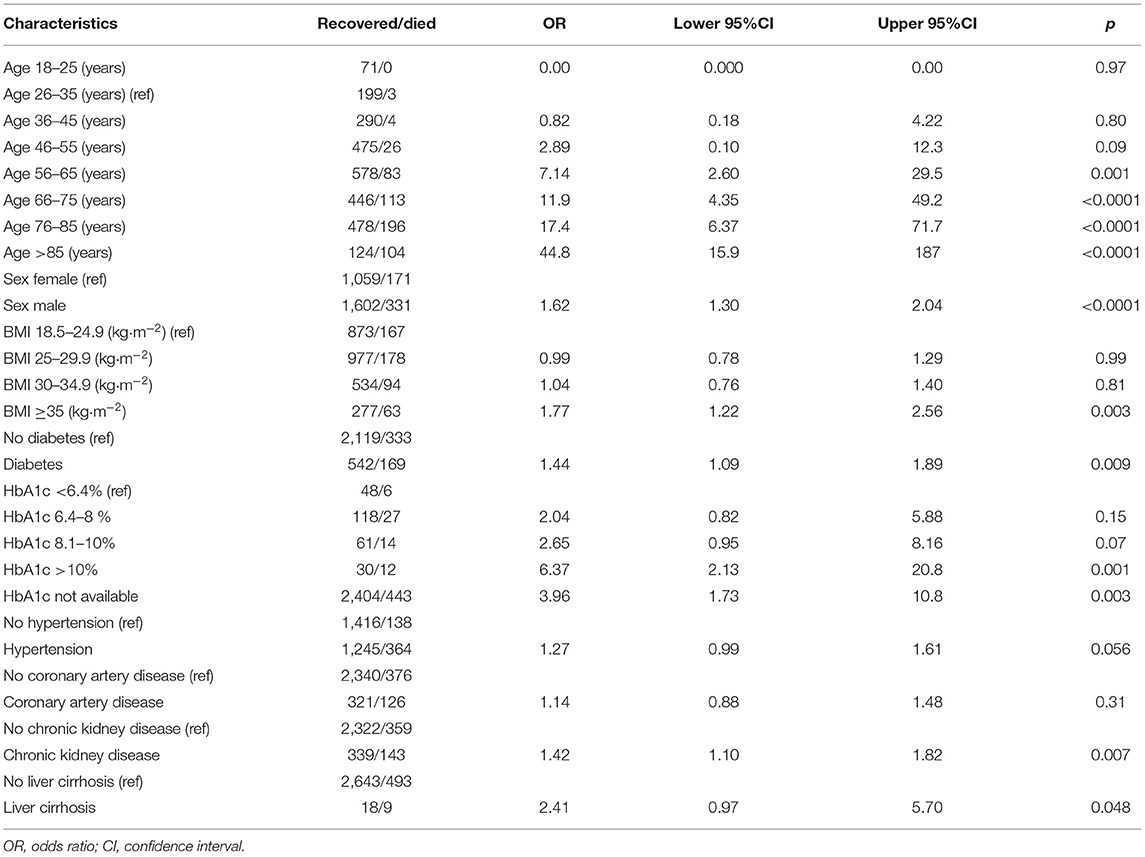
Table 1. Multivariable relationships of selected anthropometrics, comorbidities and laboratory parameters with COVID-19-related mortality.
Risk of Mortality in Young/Middle-Aged, Older and Old Patients
To investigate the relationships of obesity and impaired metabolic health with the risk of mortality in different age groups, patients were divided into three age groups (Supplementary Table 4), with 1,068 young and middle-aged, 1,220 older age and 875 old age groups. Based on the similar sample sizes these three groups were equally strong powered for the investigation of the patient's characteristics with mortality in the statistical analyses. In multivariable regression analyses male sex was associated with a higher risk of mortality in the young/middle-aged and in the old age groups, but not in the older age group. BMI ≥35 kg·m−2 was associated with increased mortality in the young/middle-aged and in the older age groups, but not in the old age group. Diabetes was associated with increased mortality only in the old age group (Supplementary Table 5).
Risk of Mortality in Subjects Stratified by Age and Obesity/Metabolic Health
To compare the contributions of advanced age vs. obesity and impaired metabolic health (diabetes and hypertension) to the mortality risk, we divided the patients into 12 subgroups based upon age and presence or absence of obesity, diabetes and hypertension. First, to investigate an additive effect of these parameters on the mortality risk, we divided the subjects in the three age groups based on the presence or absence of obesity, obesity + diabetes and obesity + diabetes + hypertension. Second, to investigate the impact of obesity + impaired metabolic health (diabetes and hypertension) on the risk of mortality more in detail, we compared the following 6 groups: (1) young and middle-aged without obesity, diabetes and hypertension (N = 593), (2) young and middle-aged with obesity, diabetes and hypertension (N = 31), (3) older age without obesity, diabetes and hypertension (N = 339), (4) older age with obesity, diabetes and hypertension (N = 148), (5) old age without obesity, diabetes and hypertension (N = 166) and (6) old age with obesity, diabetes and hypertension (N = 80).
When the age groups were stratified by the presence or absence of obesity and impaired metabolic health, both, older age and the presence of obesity and impaired metabolic health associated with increased risk of mortality (Figure 1). In the multivariable statistical model (Table 2, Model 1) moderately higher adjusted risks of mortality were observed in the young and middle-aged patients with obesity [N = 195; OR 1.75 (95% CI 0.53–5.13)] and obesity + diabetes [N = 24; OR 2.96 (95% CI 0.16–17.3)], which were statistically not significant, when compared to the young and middle-aged patients without obesity, diabetes or hypertension. However, when compared to the latter group, the adjusted risk of mortality was strongly increased in the young and middle-aged patients with obesity+impaired metabolic health [diabetes + hypertension; N = 31; OR 6.95 (95% CI 1.45–25.6)]. This group had a nearly 7-fold higher risk of mortality, compared to the young and middle-aged patients without obesity, diabetes or hypertension (Table 2, Model 1 and Figure 2).
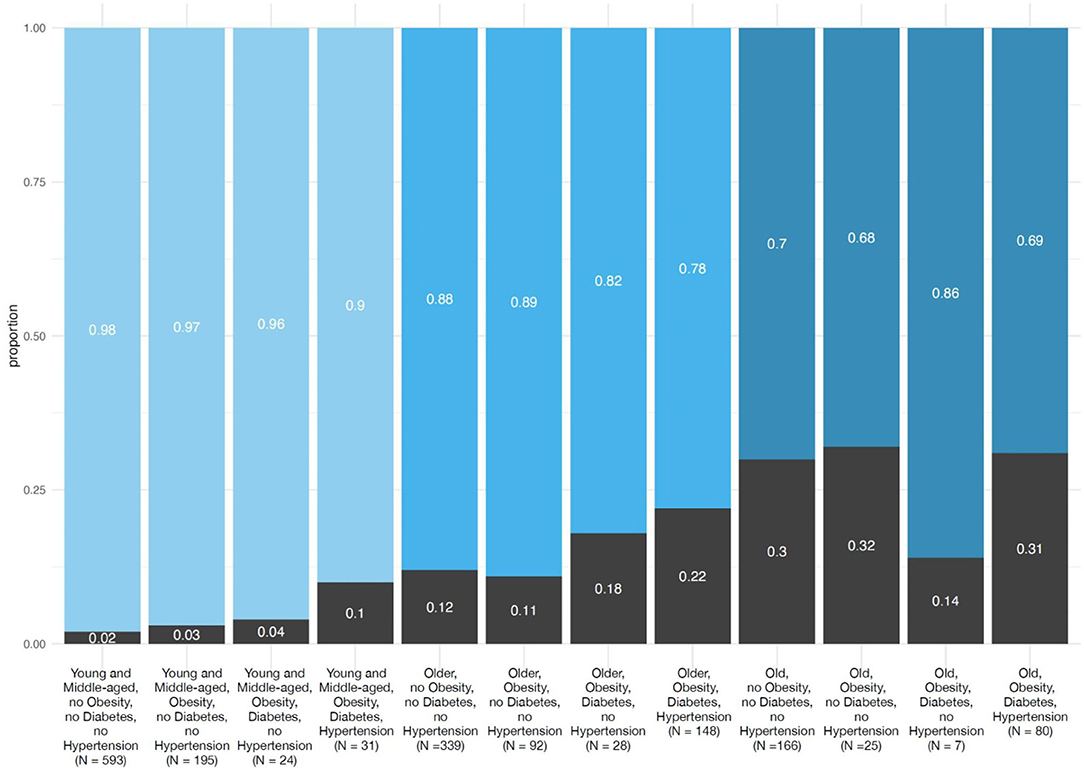
Figure 1. Proportion of COVID-19 patients who recovered and died divided in three age groups based on the presence or absence of obesity, diabetes and hypertension. All COVID-19 patients who recovered and died (n = 3,163) were first divided in three age groups (young and middle aged, 18–55 years, n = 1,068; older age, 56–75 years; n = 1,220 and old age, >75 years; n = 875) and subsequently divided in four groups based on the presence or absence of obesity (BMI ≥ 30 kg·m−2), and impaired metabolic health (diabetes and hypertension).
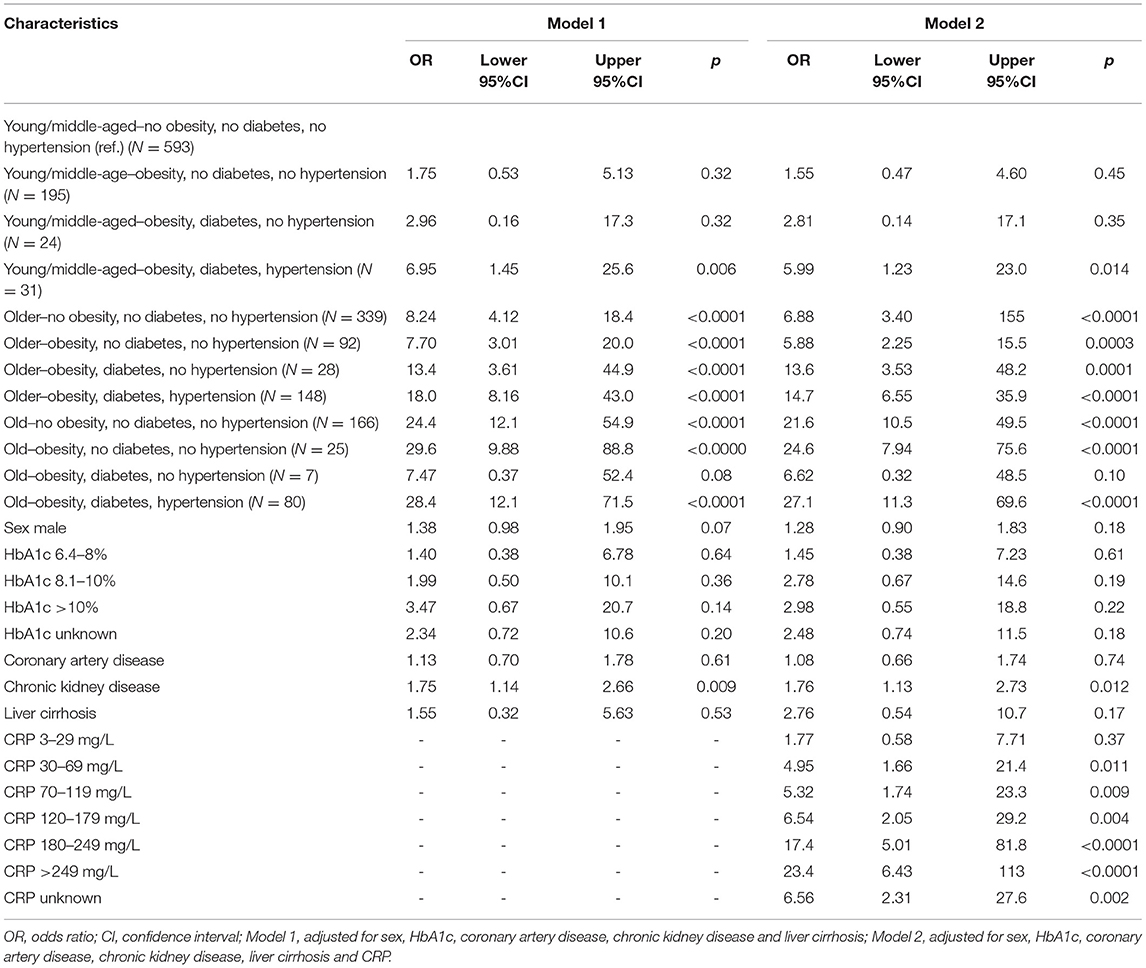
Table 2. Multivariable relationships of three age groups based on the presence (unhealthy) or absence (healthy) of obesity, diabetes and hypertension and selected anthropometrics, comorbidities and laboratory parameters with COVID-19-related mortality.
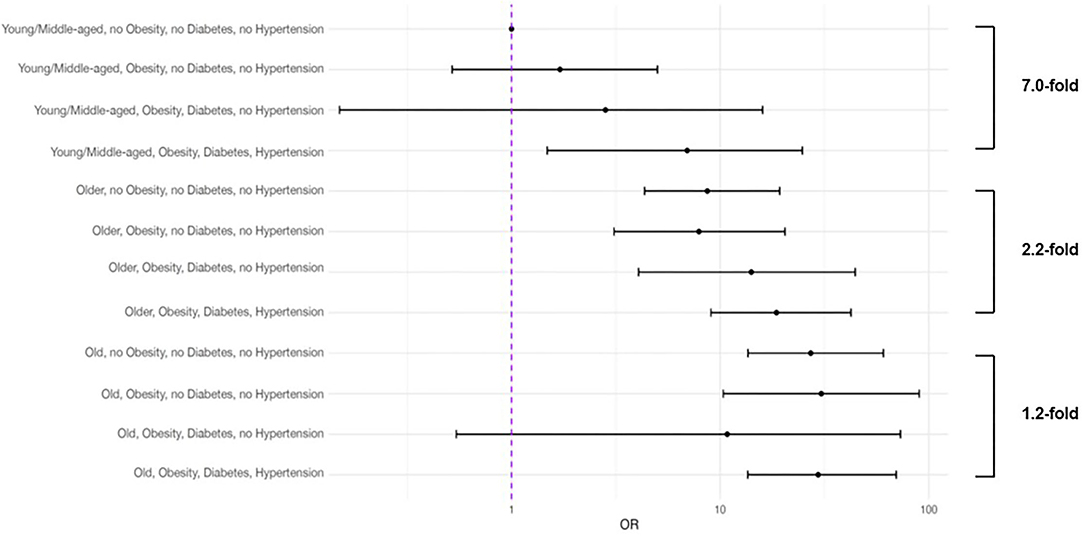
Figure 2. Multivariable relationships of selected anthropometrics, comorbidities and laboratory parameters with COVID-19-related mortality in three age groups based on the presence (unhealthy) or absence (healthy) of obesity, diabetes and hypertension. All COVID-19 patients who recovered and died (n = 3,163) were first divided in three age groups (young and middle aged, 18–55 years, n = 1,068; older age, 56–75 years; n = 1,220 and old age, >75 years; n = 875) and subsequently divided in two groups (n = 1,357) based on the presence (unhealthy) or absence (healthy) of obesity (BMI ≥ 30 kg·m−2), and impaired metabolic health (diabetes and hypertension). All parameters shown were included in the multivariable regression analysis.
Older patients without obesity, diabetes or hypertension had a higher adjusted risk of mortality [N = 339; OR 8.24 (95% CI 4.12–18.4)], compared to young and middle-aged patients without obesity, diabetes or hypertension. This risk increased in the presence of obesity, diabetes and hypertension and older patients having all three risk factors (N = 148) had an adjusted OR for mortality of 18.0 (95% CI 8.16–43.0), compared to young and middle-aged patients without obesity, diabetes or hypertension. Interestingly, this risk was merely 2.2-fold higher than the risk of older patients without obesity, diabetes and hypertension (Table 2, Model 1 and Figure 2).
Old patients without obesity, diabetes and hypertension had a very high adjusted risk of mortality [N = 166; OR 24.4 (95% CI 12.1–54.9)], compared to young and middle-aged patients without obesity, diabetes or hypertension. However, in the old patients, obesity, diabetes or hypertension only weakly increased this risk [1.2-fold higher; N = 80; OR 28.4 (95% CI 12.1–71.5)] (Table 2, Model 1 and Figure 2).
Similar relationships were observed when patients were stratified in those with an uncomplicated and a severe (complicated phase and critical phase) course of the disease. For example, when compared to the young and middle-aged patients without obesity, diabetes or hypertension, the adjusted risk of severe COVID-19 was increased in the young and middle-aged patients with obesity + impaired metabolic health [diabetes + hypertension; N = 31; OR 2.60 (95% CI 1.87–3.64)]. Furthermore, this risk was comparable to the risk observed in older non-obese and metabolically healthy patients [n = 339; OR 2.66 (95% CI 2.01–3.52)] (Supplementary Table 6).
Among the patients who died, most deaths occurred within the first 2 weeks of follow-up. In Kaplan-Meier survival analyses young and middle-aged patients with obesity and impaired metabolic (diabetes + hypertension) health had a similar time-to-death to those in the older age group without obesity and impaired metabolic health (Figure 3). Compared to young and middle-aged patients without obesity and impaired metabolic health (group 1), the adjusted OR of mortality was 6.95 (95% CI 1.45–25.6) in the young and middle-aged group with obesity and impaired metabolic health (group 2), which was not statistically different from the risk in the older age group without obesity and impaired metabolic health [OR 8.24 (95% CI 4.12–18.4)] (Table 2, Model 1 and Figure 2).
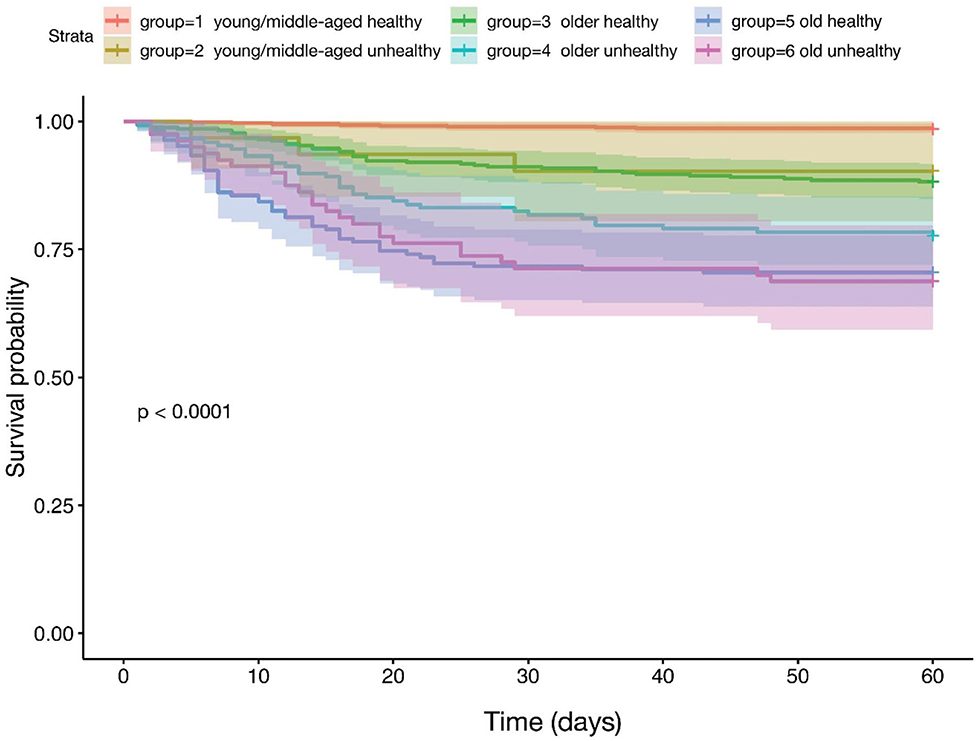
Figure 3. Kaplan-Meier survival comparing three age groups based on the presence (unhealthy) or absence (healthy) of obesity, diabetes and hypertension. All COVID-19 patients who recovered and died (n = 3,163) were first divided in three age groups (young and middle aged, 18–55 years, n = 1,068; older age, 56–75 years; n = 1,220 and old age, >75 years; n = 875) and subsequently divided in two groups (n = 1,357) based on the presence (unhealthy) or absence (healthy) of obesity (BMI ≥ 30 kg·m−2), and impaired metabolic health (diabetes and hypertension).
We then explored parameters that may explain the elevated risk of COVID-19-related mortality with age, specifically in the absence of obesity and impaired metabolic health. We additionally adjusted our multivariable regression model for CRP levels (Table 2, Model 2). This resulted in an attenuation of the elevated risk of mortality observed in older and old patients without obesity and impaired metabolic health, when compared to young and middle-aged patients without obesity and impaired metabolic health, by 17 and 11%, respectively.
To address, whether the increased risk of mortality that associated with obesity and impaired metabolic health and that was very high, particularly in the group of young and middle-aged patients, may be predominantly driven by the risk in middle-aged patients, we also divided the patients in a younger (age 18–35 years) group and a middle-aged (age 36–55 years) group. Although the sample size was very low, only allowing an exploratory evaluation, we found that young patients with obesity and impaired metabolic health had a 4.2-fold higher risk of mortality, compared to the young patients without obesity and impaired metabolic health. A similarly increased risk (3.5-fold) was observed in the middle-aged patients with obesity and impaired metabolic health, compared to the middle-aged patients without obesity and impaired metabolic health (Supplementary Table 7).
Discussion
Both, high BMI and adverse cardiometabolic status, are now established risk factors for severe COVID-19 (25). However, the risk attributed to these factors is considered to be lower than that of advanced age and perhaps also male sex. Nevertheless, the relative importance of these risk factors has not been well-studied. This knowledge gap may have direct public health implications, as metabolic risk factors–unlike age and sex–are modifiable (15–17). In this multi-national study, mostly including hospitalized patients with COVID-19, we found similar relationships of metabolic risk factors and adiposity, with COVID-19-related mortality, as were reported by previous studies (2–14). This allowed us to address an important question: to what extent does obesity, diabetes and hypertension, which were recently found to account for almost 60% of the COVID-19 hospitalizations in the United States (26), increase the risk of COVID-19-related mortality in younger patients, when compared to older patients. We found that an additive effect of obesity, diabetes and hypertension on the risk of COVID-19-related mortality exists. Compared to the respective older and old groups without these risk factors, the adjusted risk of mortality increased particularly strong in the young and middle-aged groups with these risk factors. In this respect, compared to young and middle-aged patients without obesity, patients merely having obesity only had a moderately increased adjusted mortality risk. This risk increased considerably in young and middle-aged patients with obesity and diabetes. Such an increase in risk was not observed in the older and old patients. Importantly, the presence of all three risk factors, obesity diabetes and hypertension, independently of other comorbidities and of sex, increased the risk of COVID-19-related mortality in younger and middle-aged patients to the risk level that we observed in older patients without these diseases. This finding is potentially of major public health relevance, as younger age is considered to protect from severe COVID-19.
Studies including COVID-19 patients from the United Kingdom reported that diabetes most strongly increased the risk of COVID-19-related mortality in younger patients (27, 28). Furthermore, data from the US CDC and the US Premier Healthcare Database of hospital-based patients with COVID-19 previously suggested that younger patients with obesity, diabetes or other comorbidities, have an increased risk of COVID-19-related death, that amounted to the risk often observed in older patients (21, 22). However, in those studies no adjustment for sex and comorbidities was done. In our study, diabetes was associated with an increased risk of COVID-19-related mortality in younger and in middle-aged patients, but this relationship was attenuated with adjustment for sex, BMI and other comorbidities. Thus, our findings indicate that obesity, diabetes and hypertension comprise a phenotype strongly associated with increased risk of COVID-19-related mortality in young and middle-aged patients, independently of other important determinants of severe COVID-19.
These findings may have several clinical implications. First, they support the recommendations of international medical societies, that obesity, diabetes and hypertension are important risk factors that should be critically considered by health care providers, when COVID-19 is being diagnosed in a patient. Intense clinical surveillance of these patients, particularly during the early stages of the disease, should be ensured. This approach is also supported by our findings of an increased mortality of obese and metabolically unhealthy COVID-19 patients during the first 2 weeks after diagnosis, independently of age.
Second, in view of the changing demographics of hospitalizations–with a substantial increase among patients <55 years relative to older people (21)–health care providers should not assume that younger individuals generally are at lower risk for severity of COVID-19. Consequently, younger people with these common risk factors should also be prioritized in vaccination strategies.
Third, there is increasing concern that SARS-CoV-2 will not only become an endemic virus and that an emergent coronavirus may cause severe disease in children (29–31), but that new variants of SARS-CoV-2 may evade the body's immune response, both in vaccinated and in not yet vaccinated people (29–35). Particularly the second year of the COVID-19 pandemic has been dominated by variants of concern (36, 37). Among them, mutations of the SARS-CoV-2 spike protein, the primary antigen, may be problematic, as most recently suggested for the Omicron (B.1.1.529) SARS-CoV-2 variant of concern1. In this respect obesity and diabetes may become even more important risk factors than currently considered. Obesity and impaired metabolic health may adversely influence the efficacy of SARS-CoV-2 vaccines (38, 39). In this respect, most recently some preliminary data indicate that obesity, diabetes and CVD may predispose for vaccine breakthrough COVID-19 infections (40–42). Premature immunesenescence, accelerated aging of the immune system, particularly of the CD4+ and CD8+ T cell compartments, has been found in people with obesity or type 2 diabetes (43–45). Intriguingly, as a mechanism explaining this observation, intact insulin signaling was observed to play an important role in modulating the body's immune response. Insulin receptor signaling has an impact on T cell glucose metabolism and amino acid handling. In rodents, insulin receptor-deficient T cells were found to have reduced inflammatory potential and poor protective immunity against H1N1 influenza infection (46). Considering that obesity, especially central adiposity, and impaired metabolic health, strongly associate with insulin resistance (47–49), and a healthy diet and exercise (50), as well as new dietary concepts to improve the gut microbiome (51) are very helpful to improve metabolic health, reduction of fat mass and a healthy diet may be critical for the coming months of the SARS-CoV-2 pandemic.
Fourth, most recently it was shown that, beyond the acute illness, substantial burden of health loss, including disorders of lipid metabolism, diabetes and obesity, is observed in COVID-19 survivors (52, 53). Although, this has not been investigated, yet, the presence of obesity and impaired metabolic health prior to the SARS-CoV-2 infection may particularly increase the burden of health loss in COVID-19 survivors. This may be problematic especially for younger patients, who may, thereby, experience a larger amount of years of life lost, than older patients.
A strength of our study is that the multi-center LEOSS registry prospectively collects epidemiological and clinical data based on a pre-specified protocol. Furthermore, the hospitals have the capacity to also monitor patients with asymptomatic or mild SARS-CoV-2 infections. However, there are several limitations. This study analyzed factors associated with disease course at initial presentation, not treatment, and cannot assess causality. We cannot rule out the presence of confounding from socioeconomic status, health insurance issues and access to health services and country specific testing capacities, among other factors. Some of these factors could be correlated with delayed diagnosis and therefore a more complicated clinical stage at initial presentation. Furthermore, the highest documentation rates were performed by University hospitals in larger cities; consequently, rural areas might be underrepresented. Finally, the sample size in the younger age groups was relatively small, most probably resulting from the fact that younger people generally are less often hospitalized with COVID-19 compared to middle-aged and older people. The small sample size in some of the groups may result in that a statistical error may occur from skewed group comparisons.
In conclusion, we found that obesity, diabetes and hypertension have an additive effect on COVID-19-related mortality and that this effect is particularly strong in young and middle-aged patients. Furthermore, we found that obesity, diabetes and hypertension increased the risk of COVID-19-related mortality in young and middle-aged patients to the risk level that we observed in older but metabolically healthy patients. Importantly, this increased risk was independent of other comorbidities and of sex. Awareness of health care providers about this strong impact of obesity and impaired metabolic health on the risk of COVID-19-related mortality may be critical to intensify surveillance of younger patients infected with SARS-CoV-2 and to motivate subjects at risk to lose weight and improve their metabolic health.
Data Availability Statement
Patient data from the LEOSS registry are subject to the LEOSS governance, data use, and access policy (policy text available on https://leoss.net). Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Local Ethics Committees of all participating centers and registered at the German Clinical Trails Register (DRKS, No. S00021145). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
NS and KS analyzed the data and wrote the manuscript. NS, KS, MHe, and AB designed the study. CJ, AW, YK, SB, MMR, FH, MHa, CP, MHo, JD, KW, CR, JV, MSt, and BJ collected the data and contributed to the discussion. MHe, AF, RW, HP, MSo, MRo, AS, BG, MA, DL, MSc, and AB critically reviewed the manuscript and contributed to the discussion. NS is the guarantor of this study. All authors contributed to the article and approved the submitted version.
Funding
The LEOSS registry was supported by the German Centre for Infection Research (DZIF) and the Willy Robert Pitzer Foundation. This article was also supported by funding from the German Centre for Diabetes Research (DZD).
Leoss Study Group
We express our deep gratitude to all study teams supporting the LEOSS study. The LEOSS study group contributed at least 5 per mille to the analyses of this study: University Hospital Duesseldorf (Bjoern-Erik Ole Jensen), Technical University of Munich (Christoph Spinner), University Hospital Frankfurt (Maria Vehreschild), Hospital Ingolstadt (Stefan Borgmann), University Hospital Regensburg (Frank Hanses), University Hospital Jena (Maria Madeleine Ruethrich), Hospital Passau (Julia Lanznaster), Hospital Bremen-Center (Christiane Piepel), Hospital Dortmund (Martin Hower), Maria Hilf Hospital Moenchengladbach (Juergen vom Dahl), Johannes Wesling Hospital Minden Ruhr University Bochum (Kai Wille), University Hospital Augsburg (Christoph Römmele), University Hospital Freiburg (Siegbert Rieg), University Hospital Wuerzburg (Nora Isberner), Elisabeth Hospital Essen (Ingo Voigt), Marien Hospital Herne Ruhr University Bochum (Timm Westhoff), Municipal Hospital Karlsruhe (Christian Degenhardt), University Hospital Schleswig-Holstein Luebeck (Nadja Kaeding), Hospital Ernst von Bergmann (Lukas Tometten), Hospital Leverkusen (Lukas Eberwein), University Hospital Essen (Sebastian Dolff), Elbland Hospital Riesa (Joerg Schubert), University Hospital of Giessen and Marburg (Janina Trauth), University Hospital Ulm (Beate Gruener), Robert-Bosch-Hospital Stuttgart (Katja Rothfuss), Nephrological Center Villingen-Schwenningen (Bernd Hohenstein), University Hospital Tuebingen (Silvio Nadalin), Bundeswehr Hospital Koblenz (Dominic Rauschning), University Hospital Erlangen (Richard Strauss), Helios Hospital Pirna (Christian Riedel), University Hospital Saarland (Robert Bals), University Hospital Cologne (Norma Jung), Hacettepe University (Murat Akova), Hospital Braunschweig (Jan Kielstein), Hospital of the Augustinian Cologne (Stefani Roeseler), Catholic Hospital Bochum (St. Josef Hospital), Ruhr University Bochum (Kerstin Hellwig), Tropical Clinic Paul-Lechler Hospital Tuebingen (Claudia Raichle), Hospital Preetz (Helga Peetz), Hospital St. Joseph-Stift Dresden (Lorenz Walter), Malteser Hospital St. Franziskus Flensburg (Milena Milovanovic), Medical School Hannover (Gernot Beutel), National MS Center Melsbroek (Marie D'Hooghe), Practice at Ebertplatz Cologne (Christoph Wyen), University Hospital Dresden (Katja de With), University Hospital Schleswig-Holstein - Kiel (Anette Friedrichs).
The LEOSS study infrastructure group: Jörg Janne Vehreschild (Goethe University Frankfurt), Carolin E. M. Jakob (University Hospital of Cologne), Lisa Pilgram (Goethe University Frankfurt), Melanie Stecher (University Hospital of Cologne), Max Schons (University Hospital of Cologne), Susana Nunes de Miranda (University Hospital of Cologne), Clara Bruenn (University Hospital of Cologne), Nick Schulze (University Hospital of Cologne), Sandra Fuhrmann (University Hospital of Cologne), Annika Claßen (University Hospital of Cologne), Bernd Franke (University Hospital of Cologne), Fabian Praßer (Charité, Universitätsmedizin Berlin) und Martin Lablans (University Medical Center Mannheim).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.875430/full#supplementary-material
Footnotes
1. ^https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern
References
1. Available, online at: https://covid19.who.int/ (accessed February 14, 2022).
2. Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. (2020) 382:2372-4. doi: 10.1056/NEJMc2010419
3. Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. Factors associated with death in critically Ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. (2020) 180:1436-47. doi: 10.1001/jamainternmed.2020.3596
4. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with COVID−19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. (2020) 369:m1985. doi: 10.1136/bmj.m1985
5. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. (2020) 21:e13128. doi: 10.1111/obr.13128
6. Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. (2020) 16:341-2. doi: 10.1038/s41574-020-0364-6
7. Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanism. Circulation. (2020) 142:4-6. doi: 10.1161/CIRCULATIONAHA.120.047659
8. Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. (2020) 8:782–92. doi: 10.1016/S2213-8587(20)30238-2
9. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. (2021) 17:11-30. doi: 10.1038/s41574-020-00435-4
10. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with COVID-19. N Engl J Med. (2020) 382:2534-43. doi: 10.1056/NEJMsa2011686
11. Hamer M, Kivimaki M, Gale CR, Batty GD. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav Immun. (2020) 87:184-7. doi: 10.1016/j.bbi.2020.05.059
12. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. (2020) 584:430-6. doi: 10.1038/s41586-020-2521-4
13. Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. (2020) 8:813-22. doi: 10.1016/S2213-8587(20)30272-2
14. Wang S, Ma P, Zhang S, Song S, Wang Z, Ma Y, et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia. (2020) 63:2102–11. doi: 10.1007/s00125-020-05209-1
15. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected - obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. (2021) 17:135-49. doi: 10.1038/s41574-020-00462-1
16. Drucker DJ. Diabetes, obesity, metabolism, and SARS-CoV-2 infection: the end of the beginning. Cell Metab. (2021) 33:479–98. doi: 10.1016/j.cmet.2021.01.016
17. Lockhart SM, O'Rahilly S. When two pandemics meet: why is obesity associated with increased COVID-19 mortality? Med. (2020) 1:33–42. doi: 10.1016/j.medj.2020.06.005
18. Longmore DK, Miller JE, Bekkering S, Saner C, Mifsud E, Zhu Y, et al. Diabetes and overweight/obesity are independent, nonadditive risk factors for in-hospital severity of COVID-19: an international, multicenter retrospective meta-analysis. Diabetes Care. (2021) 44:1281-90. doi: 10.2337/figshare.13616024.v1
19. Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O'Rahilly S, Aveyard P, et al. Associations between body-mass index and COVID-19 severity in 6. 9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. (2021) 9:350–9. doi: 10.1016/S2213-8587(21)00089-9
20. Leidman E, Duca LM, Omura JD, Proia K, Stephens JW, Sauber-Schatz EK. COVID-19 Trends among persons aged 0-24 years - United States, March 1-December 12, 2020. MMWR Morb Mortal Wkly Rep. (2021) 70:88–94. doi: 10.15585/mmwr.mm7003e1
21. Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, et al. Coronavirus disease 2019 case surveillance—United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:759–65. doi: 10.15585/mmwr.mm6924e2
22. Cunningham JW, Vaduganathan M, Claggett BL, Jering KS, Bhatt AS, Rosenthal N, et al. Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med. (2020) 181:379-81. doi: 10.1001/jamainternmed.2020.5313
23. Jakob CEM, Kohlmayer F, Meurers T, Vehreschild JJ, Prasser F. Design and evaluation of a data anonymization pipeline to promote open science on COVID-19. Sci Data. (2020) 7:435. doi: 10.1038/s41597-020-00773-y
24. Jakob CEM, Borgmann S, Duygu F, Behrends U, Hower M, Merle U, et al. First results of the “Lean European open survey on SARS-CoV-2-infected patients (LEOSS)”. Infection. (2021) 49:63–73. doi: 10.1007/s15010-020-01499-0
25. Centers for Disease Control Prevention. Science Brief: Evidence Used to Update the List of Underlying Medical Conditions that Increase a Person's Risk of Severe Illness From COVID-19 Atlanta: Centers for Disease Control and Prevention. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html (accessed March 29, 2021).
26. O'Hearn M, Liu J, Cudhea F, Micha R, Mozaffarian D. Coronavirus disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis. J Am Heart Assoc. (2021) 10:e019259. doi: 10.1161/JAHA.120.019259
27. Dennis JM, Mateen BA, Sonabend R, Thomas NJ, Patel KA, Hattersley AT, et al. Type 2 diabetes and COVID-19-related mortality in the critical care setting: a national cohort study in England, March-July 2020. Diabetes Care. (2021) 44:50–7. doi: 10.2337/dc20-1444
28. McGovern AP, Thomas NJ, Vollmer SJ, Hattersley AT, Mateen BA, Dennis JM. The disproportionate excess mortality risk of COVID-19 in younger people with diabetes warrants vaccination prioritisation. Diabetologia. (2021) 64:1184-6. doi: 10.1007/s00125-021-05404-8
29. Phillips N. The coronavirus is here to stay - here's what that means. Nature. (2021) 590:382-4. doi: 10.1038/d41586-021-00396-2
30. Lavine JS, Bjornstad ON, Antia R. Immunological characteristics govern the transition of COVID-19 to endemicity. Science. (2021) 371:741-5. doi: 10.1126/science.abe6522
31. Paules CI, Fauci AS. COVID-19: The therapeutic landscape. Med. (2021) 2:493–7. doi: 10.1016/j.medj.2021.04.015
32. Rubin R. COVID-19 Vaccines vs variants-determining how much immunity is enough. JAMA. (2021) 325:1241-43. doi: 10.1001/jama.2021.3370
33. Callaway E. Fast-spreading COVID variant can elude immune responses. Nature. (2021) 589:500-1. doi: 10.1038/d41586-021-00121-z
34. Hie B, Zhong ED, Berger B, Bryson B. Learning the language of viral evolution and escape. Science. (2021) 371:284-8. doi: 10.1126/science.abd7331
35. Sabino EC, Buss LF, Carvalho MPS, Prete CA Jr, Crispim MAE, Fraiji NA, et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet. (2021) 397:452-5. doi: 10.1016/S0140-6736(21)00183-5
36. Bushman M, Kahn R, Taylor BP, Lipsitch M, Hanage WP. Population impact of SARS-CoV-2 variants with enhanced transmissibility and/or partial immune escape. Cell. (2021) 184:6229-42.e18. doi: 10.1016/j.cell.2021.11.026
37. Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. (2021) 19:409–24. doi: 10.1038/s41579-021-00573-0
38. Ledford H. How obesity could create problems for a COVID vaccine. Nature. (2020) 586:488-9. doi: 10.1038/d41586-020-02946-6
39. Stefan N. Metabolic disorders, COVID-19 and vaccine-breakthrough infections. Nat Rev Endocrinol. (2022) 18:75-6. doi: 10.1038/s41574-021-00608-9
40. Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. (2021) 384:1412–23. doi: 10.1056/NEJMoa2101765
41. Juthani PV. Hospitalisation among vaccine breakthrough COVID-19 infections. Lancet Infect Dis. (2021) 21:1485–6. doi: 10.1016/S1473-3099(21)00558-2
42. Agrawal U, Katikireddi SV, McCowan C, Mulholland RH, Azcoaga-Lorenzo A, Amele S, et al. COVID-19 hospital admissions and deaths after BNT162b2 and ChAdOx1 nCoV-19 vaccinations in 2·57 million people in Scotland (EAVE II): a prospective cohort study. Lancet Respir Med. (2021) 9:1439–49. doi: 10.1016/S2213-2600(21)00380-5
43. Kumar V. How could we forget immunometabolism in SARS-CoV2 infection or COVID-19? Int Rev Immunol. (2021) 40:72–107. doi: 10.1080/08830185.2020.1840567.
44. De La Fuente M, De Castro NM. Obesity as a model of premature immunosenescence. Curr Immunol Rev. (2012) 8:63-75. doi: 10.2174/157339512798991290
45. Lau EYM, Carroll EC, Callender LA, Hood GA, Berryman V, Pattrick M, et al. Type 2 diabetes is associated with the accumulation of senescent T cells. Clin Exp Immunol. (2019) 197:205-13. doi: 10.1111/cei.13344
46. Tsai S, Clemente-Casares X, Zhou AC, Lei H, Ahn JJ, Chan YT, et al. Insulin receptor-mediated stimulation boosts T cell immunity during inflammation and infection. Cell Metab. (2018) 28:922-34.e4. doi: 10.1016/j.cmet.2018.08.003
47. Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. (2006) 444:881–7. doi: 10.1038/nature05488
48. Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. (2019) 7:715–25. doi: 10.1016/S2213-8587(19)30084-1
49. Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. (2020) 8:616-27. doi: 10.1016/S2213-8587(20)30110-8
50. Magkos F, Hjorth MF, Astrup A. Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. (2020) 16:545–55. doi: 10.1038/s41574-020-0381-5
51. Canfora EE, Meex RCR, Venema K, Blaak EE. Gut microbial metabolites in obesity, NAFLD and T2DM. Nat Rev Endocrinol. (2019) 15:261–73. doi: 10.1038/s41574-019-0156-z
52. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequalae of COVID-19. Nature. (2021) 594:259–64. doi: 10.1038/s41586-021-03553-9
Keywords: obesity, diabetes, hypertension, impaired metabolic health, mortality, COVID-19
Citation: Stefan N, Sippel K, Heni M, Fritsche A, Wagner R, Jakob CEM, Preißl H, von Werder A, Khodamoradi Y, Borgmann S, Rüthrich MM, Hanses F, Haselberger M, Piepel C, Hower M, vom Dahl J, Wille K, Römmele C, Vehreschild J, Stecher M, Solimena M, Roden M, Schürmann A, Gallwitz B, Hrabe de Angelis M, Ludwig DS, Schulze MB, Jensen BEO and Birkenfeld AL (2022) Obesity and Impaired Metabolic Health Increase Risk of COVID-19-Related Mortality in Young and Middle-Aged Adults to the Level Observed in Older People: The LEOSS Registry. Front. Med. 9:875430. doi: 10.3389/fmed.2022.875430
Received: 14 February 2022; Accepted: 08 April 2022;
Published: 11 May 2022.
Edited by:
Roger Nlandu Ngatu, Kagawa University, JapanReviewed by:
Olivier Mukuku, Institut Supérieur des Techniques Médicales de Lubumbashi, Democratic Republic of CongoJens Jordan, German Aerospace Center (DLR), Germany
Quanman Li, Zhengzhou University, China
Copyright © 2022 Stefan, Sippel, Heni, Fritsche, Wagner, Jakob, Preißl, von Werder, Khodamoradi, Borgmann, Rüthrich, Hanses, Haselberger, Piepel, Hower, vom Dahl, Wille, Römmele, Vehreschild, Stecher, Solimena, Roden, Schürmann, Gallwitz, Hrabe de Angelis, Ludwig, Schulze, Jensen and Birkenfeld. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norbert Stefan, norbert.stefan@med.uni-tuebingen.de
†These authors have contributed equally to this work
 Norbert Stefan
Norbert Stefan Katrin Sippel
Katrin Sippel Martin Heni
Martin Heni Andreas Fritsche
Andreas Fritsche Robert Wagner
Robert Wagner Carolin E. M. Jakob4,5
Carolin E. M. Jakob4,5  Hubert Preißl
Hubert Preißl Yascha Khodamoradi
Yascha Khodamoradi Stefan Borgmann
Stefan Borgmann Jürgen vom Dahl
Jürgen vom Dahl Michele Solimena
Michele Solimena Michael Roden
Michael Roden Annette Schürmann
Annette Schürmann Baptist Gallwitz
Baptist Gallwitz David S. Ludwig
David S. Ludwig Matthias B. Schulze
Matthias B. Schulze Bjoern Erik Ole Jensen
Bjoern Erik Ole Jensen Andreas L. Birkenfeld
Andreas L. Birkenfeld