Abstract
COVID-19 limitation strategies have led to widespread school closures around the world. The present study reports children’s mental health and associated factors during the COVID-19 school closure in France in the spring of 2020. We conducted a cross-sectional analysis using data from the SAPRIS project set up during the COVID-19 pandemic in France. Using multinomial logistic regression models, we estimated associations between children’s mental health, children’s health behaviors, schooling, and socioeconomic characteristics of the children’s families. The sample consisted of 5702 children aged 8–9 years, including 50.2% girls. In multivariate logistic regression models, children’s sleeping difficulties were associated with children’s abnormal symptoms of both hyperactivity-inattention (adjusted Odds Ratio (aOR) 2.05; 95% Confidence Interval 1.70–2.47) and emotional symptoms (aOR 5.34; 95% CI 4.16–6.86). Factors specifically associated with abnormal hyperactivity/inattention were: male sex (aOR 2.29; 95% CI 1.90–2.76), access to specialized care prior to the pandemic and its suspension during school closure (aOR 1.51; 95% CI 1.21–1.88), abnormal emotional symptoms (aOR 4.06; 95% CI 3.11–5.29), being unschooled or schooled with assistance before lockdown (aOR 2.13; 95% CI 1.43–3.17), and tutoring with difficulties or absence of a tutor (aOR 3.25; 95% CI 2.64–3.99; aOR 2.47; 95% CI 1.48–4.11, respectively). Factors associated with children’s emotional symptoms were the following: being born pre-term (aOR 1.34; 95% CI 1.03–1.73), COVID-19 cases among household members (aOR 1.72; 95% CI 1.08–2.73), abnormal symptoms of hyperactivity/inattention (aOR 4.18; 95% CI 3.27–5.34) and modest income (aOR 1.45; 95% CI 1.07–1.96; aOR 1.36; 95% CI 1.01–1.84). Multiple characteristics were associated with elevated levels of symptoms of hyperactivity-inattention and emotional symptoms in children during the period of school closure due to COVID-19. Further studies are needed to help policymakers to balance the pros and cons of closing schools, taking into consideration the educational and psychological consequences for children.
Similar content being viewed by others
Introduction
The emergence of COVID-19 in 2020 led many countries to implement strict sanitary measures, many of which resulted in substantial changes in children’s lifestyles for several months. On March 31, 2020, 170 countries temporarily closed schools in an attempt to limit the spread of the new coronavirus responsible for this disease1. In France, the first lockdown lasted from March 16 to May 11, 2020, and schools and universities, which offer teaching to 14 million students, closed from the beginning of the lockdown until June 22, 20202. School closures, the absence of usual sports and leisure activities, and a reduction in social contacts may have impacted children’s mental health in an unprecedented manner3,4,5,6,7,8,9. Children may have been exposed to stressors generated by the media, the fear of contagion, the lack of social interactions with individuals outside the immediate family, and by family members affected with COVID-1910,11,12. Moreover, the COVID-19 crisis may have resulted in socioeconomic difficulties (e.g., financial loss and changes in employment status) and impacted the mental health of adults, which in turn may have had indirect effects on mental health in children10,13,14. The potential benefits of closing schools to curb the spread of COVID-19 need to be weighed against the effects on children’s mental health15.
Although there is no consensus on the effectiveness of school closures to minimize the spread of COVID-1915,16,17, deleterious short-term effects on children’s mental health have been observed. A Chinese study of 7143 college students found that 24.9% experienced anxiety related to the COVID-19 outbreak3. Another Chinese cross-sectional study using an online questionnaire on 359 children and 3254 adolescents showed that 22.3% suffered from depressive symptoms during the outbreak18. In addition, an internet-based survey evaluated the behavioral problems of 1264 children using the Strengths and Difficulties Questionnaire (SDQ), in two elementary schools in China during the COVID-19 outbreak19. The prevalence was 6.3% for hyperactivity/inattention and 4.7% for emotional symptoms19. However, to date the majority of studies on this topic have been carried out in China where the epidemic has been of shorter duration than in other parts of the world3,4,18,20,21,22. In France, a survey that used the SDQ on 432 parents showed that 24.7% of their children had hyperactivity/inattention symptoms and that 7.1% had emotional difficulties during the first lockdown in the spring of 202014. This study based on a small sample of children identified significant correlates of these symptoms with parental mental health or financial difficulties, as well as the child’s sleeping difficulties or high screen time use. A study conducted in the Philippines among 952 college students aged 18–22 years old showed that students from poorer households, who do not own laptops and desktop computers, and have a lesser variety of gadgets, exhibited higher disease-related COVID-19 anxiety12. Therefore, social inequalities related to children's health were exacerbated by this unprecedented situation5. These studies had several limitations like a small sample size or the non-inclusion of other factors that might affect children's mental health, such as chronic illness and number of hours of study at home per day23. Furthermore, while a significant number of studies were conducted on the indirect effects of the COVID-19 pandemic on mental health, only a few focused on children13,24. More research is therefore needed to quantify the impact of socioeconomic disparities and inequalities that are exacerbated by school closure and that of the lockdown on children's mental health25.
The present study sought to assess the factors associated with the mental health of children aged 8–9 years-old during the school closure in the first lockdown in spring of 2020 in France. We focused on children’s hyperactivity/inattention and emotional symptoms, and on a range of factors such as health behaviors (e.g., sleeping difficulties), schooling (e.g., tutoring, time devoted to schoolwork), and socioeconomic characteristics of children’s families (e.g., financial difficulties, type of housing, occupational category).
Methods
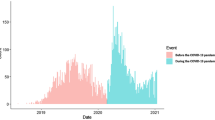
In the early weeks of the COVID-19 crisis, the SAPRIS survey was set up to study the health, social interactions and socioeconomic characteristics of the general population during the crisis in France26. The project was based on the collection of data using the same questionnaire on the participants of five large ongoing French cohorts, three of adults (Constances, E3N-E4N and NutriNet-Santé) and two of children (ELFE/EPIPAGE-2). For the present study, we used data collected on the 5702 children aged 8–9 years old in 2020 and participating in the ELFE and EPIPAGE-2 population-based birth cohorts that focus on child health and include late pre-term and term (ELFE) and very and extremely premature children (EPIPAGE-2) born in 201127,28,29. More details on ELFE and EPIPAGE 2 are available elsewhere27,28,29. Data for the present study were reported by parents during the first lockdown period (from April 16 to May 4, 2020) or immediately after (from May 5 to June 21, 2020), thus encompassing the whole period of school closure30. To make the target populations completely disjointed and complementary, 48 children born before 35 weeks in ELFE were excluded. All methods were performed in accordance with the relevant guidelines and regulations. Ethical approval and written informed consents were obtained from all subjects and/or their legal guardian. The study was approved by the Inserm ethics evaluation committee (no 2020.04.24 bis_20.04.22.74247, 2020 April 27), and the CNIL ((no 920193, 2020 April 30). Representatives of the participants tested and validated the questionnaires, but they did not contribute to other aspects related to the design, conduct, reporting or dissemination of the research.
Children’s mental health
Symptoms of hyperactivity/inattention and emotional symptoms were ascertained by two subscales of the SDQ, a widely used measure of children’s mental health which has satisfactory psychometric properties31,32. These symptoms concerned the 15 days prior to the questionnaire and were reported by parents on a 3-point scale (not true, somewhat true, and certainly true; ranges from 0 to 2) to indicate the extent to which each item applied to their children33,34. The following five items were used to assess symptoms of hyperactivity/inattention: “Restless, overactive, cannot stay still for long”; “Constantly fidgeting or squirming”; “Easily distracted, concentration wanders”; “Thinks things out before acting”; and “Sees tasks through to the end, good attention span”33. The five items used to assess the emotional symptoms were: “Complains of headache/stomach ache”; “Many worries, often seems worried”; “Often unhappy, down-hearted or tearful”; “Nervous or clingy in new situations, easily loses confidence”; and “Many fears, easily scared”32. From the parents' responses to the five items of each subscale, we calculated scores that ranged from 0 to 10 with cut-offs of the French version of the SDQ35. Concerning hyperactivity/inattention, a score ≤ 5 is considered normal, equal to 6 as boundary state (moderate), and > 6 as abnormal. For emotional symptoms, a score ≤ 3 is considered normal, equal to 4 as boundary state (moderate), and > 4 as abnormal.
Covariates
Children’s health behavior
Health behaviors included the following: sleeping difficulties (e.g., difficulty falling asleep, waking up frequently or too early at night without being able to go back to sleep) since the beginning of lockdown (yes: new occurrence, increase, or stability, no: decrease, disappearance or none); time per day spent by child on the following activities: (a) reading, drawing, board games; (b) screen for recreation, (c) social network, (d) physical activity (sports or walks outside; indoor and outdoor physical activity).
Children’s schooling
Educational characteristics included the following: school situation before lockdown (normal; with assistance or unschooled); average time devoted to schoolwork per day (none or less than 1 h, 1–3 h, > 3 h); tutoring difficulty (tutoring with difficulty, tutoring without difficulty, no tutoring); average screen time for educational reasons per day. Tutoring refers to the presence of someone who can help the child with homework (e.g., parents, siblings, grandparents etc.). Screen time for educational reasons refers to time spent on television or other screens to follow school or educational programs.
Socioeconomic characteristics of children’s families
Socioeconomic characteristics included the following: the parents’ occupational category (executive, intermediate and executive, intermediate and employee, independent, laborer, 2 inactive or only one employee/laborer); change in parents’ work situation (change at least for one parent, no change for either parent); parents’ distance working (neither working, one teleworking and the other not working, at least one working outside, both teleworking); perceived financial situation (affluent and constant income; affluent and declining income; modest and constant income; modest and declining income); type of housing (rural house, urban house, flat with balcony/garden, flat without balcony/garden, other); region classified according to the prevalence of COVID-19 at the beginning of the epidemic (High: Ile de France and Grand Est vs Medium: Bourgogne-Franche-Comté, Auvergne-Rhône-Alpes and Hauts-de-France vs. Low: other regions); number of rooms per inhabitant and if the child lived with both parents or not.
Others
Additional data included the following: sex; chronic disease (yes, no); born pre-term (yes, no); children’s access to specialized care prior to the COVID-19 epidemic (e.g., physiotherapist, speech therapist, psychologist, rehabilitation) and its continuation during school closures (yes and pursuit, yes but no pursuit, no); COVID-19 cases among household members (yes, no).
Statistical analysis
We first described child and family sociodemographic characteristics, (i.e., weighted means with standard deviations for continuous variables; frequency with weighted percentages for categorical variables). Descriptive analyses were conducted after correcting the sample data to be representative of children born in France in 201136. For this purpose, a weighting coefficient was calculated. For more information, see the online supplement.
Before performing multiple imputation, we removed variables with more than 30% missing data (screen time and physical activity) and observations with missing data for both outcomes (hyperactivity/inattention and emotional symptoms). Classification and Regression Tree methods (CART, imputation method for mixed data: both Continuous and Categorical)37 for multiple imputation were used to handle missing data. Secondly, to test the association between each covariate and mental health outcomes (i.e., hyperactivity/inattention and emotional symptoms), we used multinomial logistic regressions adjusted on prematurity to estimate Odds Ratios (OR) and 95% confidence intervals (CI). Thirdly, to perform relevant covariate selection, we applied a penalized regression method, Elastic-Net, combining bootstrapping with multiple imputed data38,39,40. We used the variable inclusion probability with a 50% threshold to select variables associated with children’s mental health. Finally, we used multinomial logistic regression to estimate adjusted OR and 95% CI for the association between variables selected by Elastic-Net, prematurity and both mental health outcomes.
Data were analyzed using the nnet package in R (version 3.6.1) with multinomial logistic regressions specified using the multinom function. The mice package and its cart method were used to perform multiple imputation. Finally, the caret, glmnet, doParallel and dplyr packages were applied to implement the Elastic-Net method on imputed data.
Results
Sample characteristics
The study included 5702 children (Table 1). In total, 2808 (50.2%) children were females, 1161 (19.4%) had access to specialized care prior to the COVID-19 epidemic, 289 (4.5%) had chronic disease, and 1122 (2.9%) were premature children. COVID-19 cases were reported in 235 (4.4%) households. Concerning the children’s mental health, hyperactivity/inattention scores were abnormal for 672 (13.6%) and moderate for 452 (8.2%) children, respectively. Emotional difficulties scores were abnormal or moderate for 404 (7.5%) and 288 (5.8%) children, respectively. In terms of children’s health behaviors, 39.9% had sleeping difficulties. Children spent an average of 2 h and 20 min reading, drawing, and playing board games per day, and 2 h and 45 min doing physical activities per day. Regarding screen time, children spent an average of 3 h and 10 min per day for recreation, and 5 min on social networks. Only 188 (2.8%) children were unschooled or in school with assistance before the lockdown, 2764 (62.8%) spent between 1 and 3 h per day on schoolwork and an average of 50 min on educational programs per day. 4202 (96.7%) children had a tutor at home to help them with their homework.
As shown in Table 2, the pandemic situation led to a change in work situation in 1483 (43.9%) households, working from home was implemented in 2371 households (32.6%) and 1813 (41.6%) perceived financial difficulties. Children lived mostly in a house (67.4%) and with their two parents (84.5%). 9.0% and 17.3% of children lived in regions with high or moderate prevalence of COVID, respectively.
Factors associated with hyperactivity/inattention and/or emotional symptoms
The factors associated with hyperactivity/inattention and/or emotional symptoms when adjusting for prematurity are presented in Tables 3 and 4. The factors associated with an increased risk of both hyperactivity/inattention and emotional symptoms in univariate analysis were the following: having chronic disease, being born pre-term, having access to specialized care prior to the COVID-19 epidemic, having difficulties in sleeping, being schooled with assistance or unschooled before the lockdown, having difficulties with tutoring or not having a tutor, low parents’ dominant socio-professional category, presence of change in the parents' work situation, having modest and declining outcome during the lockdown, and not living with both parents. The factor associated with a lower risk of both hyperactivity/inattention and emotional symptoms adjusted on prematurity was having at least one parent who worked outside.
Factors exclusively associated with an increased risk of hyperactivity/inattention adjusted on prematurity were the following: being a boy; having emotional symptoms. Factors associated with a decreased risk of symptoms of hyperactivity/inattention were the following: spending 1–3 h or more than 3 h per day devoted to schoolwork, having parents working remotely, and living in an urban environment.
In contrast, factors only associated with an increased risk of emotional symptoms adjusted on prematurity were the following: presence of COVID-19 cases in the household, hyperactivity/inattention symptoms, having modest and constant income, and living in an urban flat without a balcony/garden. The only factor associated with a lower risk of emotional symptoms was being a boy.
Finally, the number of rooms per inhabitant and the French regions most affected by the COVID-19 epidemic were not associated with children’s mental health.
Factors associated with children’s mental health after Elastic Net selection
The factors most strongly associated with children’s mental health after using Elastic Net selection are presented in Tables 5 and 6. Elastic Net selected 10 factors as most associated with hyperactivity/inattention in children: sex, access to specialized care prior to the COVID-19 epidemic, having emotional symptoms, having sleeping difficulties, being schooled with assistance or unschooled before the lockdown, devoting 1 h or less to school work per day, having difficulties with tutoring or not having a tutor, low parents’ dominant socio-professional category, living in an urban house, and not living with both parents (Table 5).
After adjusting for these 10 factors most associated with hyperactivity/inattention symptoms and prematurity, boys remained at greater risk for abnormal hyperactivity-inattention than girls (aOR 2.29; 95% CI 1.90–2.76). Children who had regular care before the COVID-19 epidemic and could not continue the sessions during the lockdown had an increased risk of abnormal hyperactivity/inattention symptoms (aOR 1.51; 95% CI 1.21–1.88).
Concerning children’s mental health, compared to normal children, children with abnormal emotional symptoms or at boundary state were associated with higher risk of abnormal hyperactivity/inattention symptoms (aOR 4.06; 95% CI 3.11–5.29 and aOR 2.14; 95% CI 1.54–2.97, respectively). Regarding the children’s health behavior, risk of abnormal hyperactivity/inattention symptoms or at boundary state appeared to be higher for children with sleeping difficulties (OR 2.05; 95% CI 1.70–2.47, OR 1.71; 95% CI 1.39–2.10) than in those without sleeping difficulties (Table 5).
Regarding children’s schooling, being schooled with assistance or unschooled was associated with a higher risk of abnormal hyperactivity/inattention (aOR 2.13; 95% CI 1.43–3.17). Spending 1–3 h per day devoted to schoolwork or more than 3 h seemed to be associated with less risk of abnormal hyperactivity/inattention symptoms than spending no time or less than 1 h (aOR 0.55; 95% CI 0.34–0.91 and aOR 0.56; 95% CI 0.33–0.92, respectively). In this multivariate analysis, having difficulties with tutoring or not having a tutor were still associated with a higher risk of abnormal hyperactivity/inattention (aOR 3.25; 95% CI 2.64–3.99 and aOR 2.47; 95% CI 1.48–4.11, respectively).
For socioeconomic characteristics, the low parents’ occupational category (laborer) was still associated with a higher risk of abnormal hyperactivity/inattention as compared to the executive category (aOR 1.66; 95% CI 1.01–2.71). Compared to living in a rural house, living in an urban house was associated with less risk of abnormal hyperactivity/inattention symptoms (aOR 0.79; 95% CI 0.64–0.97).
Concerning the factors most associated with emotional symptoms, Elastic Net selected the following seven variables: being born pre-term, COVID-19 cases in the household, hyperactivity-inattention symptoms, sleeping difficulties, parents’ occupational category, change in parents’ work situation, and financial situation (Table 6). The results described below are adjusted on these seven variables.
Children born pre-term remained at a higher risk of abnormal emotional symptoms (aOR 1.34; 95% CI 1.03–1.73). The presence of COVID-19 cases in the household (aOR 1.72; 95% CI 1.08–2.73), abnormal symptoms of hyperactivity/inattention (aOR 4.18; 95% CI 3.27–5.34) and sleeping difficulties (aOR 5.34; 95% CI 4.16–6.86) remained risk factors of abnormal emotional symptoms (Table 6). In this multivariate analysis, only the “intermediate and executive” parents’ occupational category was still associated with a higher risk of abnormal emotional symptoms as compared to the "executive" category (aOR 1.61; 95% CI 1.16–2.21). Having a modest income remained a risk factor of abnormal emotional symptoms (aOR 1.45; 95% CI 1.07–1.96; aOR 1.36; 95% CI 1.01–1.84). A change in parents’ work situation during school closures was no longer significantly associated with emotional symptoms.
Discussion
Main findings and interpretations
Our study showed high rates of hyperactivity/inattention and emotional symptoms during school closure due to COVID-19 in France. It also helped in identifying risk factors of hyperactivity/inattention and/or emotional symptoms in children. Difficulties in sleeping and parents’ occupational category were the only factors independently associated in the multivariate models with both dimensions of mental disorder. Factors specifically associated with hyperactivity/inattention were the following: sex, presence of regular care and its pursuit during school closure, emotional symptoms, school situation, presence of tutoring and difficulties with it, and type of housing. Factors related to emotional symptoms were the following: being born pre-term, the presence of COVID-19 cases in the household, hyperactivity/inattention and financial difficulties.
Children’s sex, chronic disease, specialized care and being born pre-term
In the context of the COVID-19 crisis, our results indicate a higher risk of hyperactivity/inattention among boys than girls, and a higher risk of emotional symptoms among girls than boys. Findings by others were similar outside the context of the COVID-19 pandemic41,42 and our findings are consistent with those of recent studies on it4,43,44. A cross-sectional online survey of 8079 Chinese adolescents aged 12–18 affected by the COVID-19 pandemic revealed that female gender was the most important risk factor for depressive and anxiety symptoms4.
After adjustment on covariates, we found that children who had access to specialized care prior to the COVID-19 pandemic and who were unable to continue follow up during school closures had a higher risk of abnormal hyperactivity-inattention. Being born pre-term was associated with a higher risk of abnormal emotional symptoms during the COVID-19 pandemic. These results are coherent with epidemiological studies conducted outside the COVID-19 context which found that pre-and perinatal factors (e.g. prematurity, chronic disease) are associated with Attention-Deficit/Hyperactivity Disorder (ADHD)45,46,47 and emotional problems48,49, although the definite causes remain unknown. While being born pre-term is a known risk factor for hyperactivity/inattention disorder50,51, it is the association between prematurity and emotional symptoms that is emphasized by our findings.
COVID-19 cases in the household
In our multivariate analyses, the presence of COVID-19 cases in the household seemed to be a risk factor of abnormal emotional symptoms in children. This was one of the strongest associations according to Elastic Net. These results are in line with a large cross-sectional online survey of 44,447 college students conducted in China52. Compared with students who reported not having infected or suspected cases in family members and relatives, those who reported having confirmed and suspected cases in family members and relatives had a higher risk of depressive symptoms (OR 4.06; 95% CI 1.62–10.19 and OR 2.11; 95% CI 1.11–4.00, respectively)52. Interestingly, several studies evidenced an association between emotional symptoms and COVID-19 epidemic-related factors such as potential exposure to the virus, fear of infection (i.e., self- and/or family members), and loss of loved ones3,53,54. Other studies found an increased risk of post-traumatic stress disorder (PTSD) symptoms55 and moderate to high perceived stress scores56 in isolated/quarantined individuals during the COVID-19 pandemic. Mental stress, anxiety, depressive symptoms, insomnia and fear are triggered by the pandemic itself, mandatory preventive measures, and COVID-19-related circumstances53,54,57.
Children’s mental health
Our findings showed that during the school closure in France, hyperactivity/inattention and emotional symptoms were associated. Elastic Net found this to be one of the strongest associations. Our results confirm those of another study conducted outside the epidemic context which showed a stronger correlation between hyperactivity/inattention and emotional symptoms in the SDQ34.
Children’s health behavior: sleep difficulties
Our study is consistent with recent reports on the association between difficulties in sleeping and children's mental health during the COVID-19 pandemic14, in particular with hyperactivity/inattention and emotional symptoms. Difficulty in sleeping is one of the most predictive variables of hyperactivity/inattention in children, as well as emotional symptoms. Our findings confirm those of previous studies conducted outside the COVID-19 pandemic58,59,60. Hyperactivity/inattention and emotional symptoms are both characteristics of children with ADHD. A meta-analysis of 16 studies comparing sleep in ADHD children versus controls found that the former were significantly more impaired than the latter on most subjective and some objective sleep measures60. The relationship between ADHD and difficulties in sleeping is bidirectional59,61,62,63. ADHD may cause sleep problems and sleep problems may cause or mimic ADHD58,59. Moreover, a reciprocal relationship between sleep quality and anxiety problems seems very likely, although the specific mechanisms that contribute to these sleep disturbances remain unclear64,65,66,67.
Children’s schooling: school situation, time devoted to schoolwork, and tutoring
In multivariate analyses, being unschooled or schooled with assistance before the lockdown was associated with a higher risk of abnormal hyperactivity/inattention. Spending 1–3 h or more than 3 h per day on schoolwork seemed to be associated with a lower risk of abnormal hyperactivity/inattention symptoms than spending no time or less than 1 h. Furthermore, children without a tutor and those with tutoring difficulties were at greater risk for abnormal hyperactivity–inattention compared with those without tutoring difficulties. Our results are consistent with those of a previous study, which found that prolonged school closure regardless of the epidemic context can cause significant mental health problems in children, especially among economically disadvantaged groups68. While schools are essential for children’s academic education, they also play an important role in addressing their physiological and mental health needs68,69. However, according to Elastic Net, these schooling variables are not strongly associated with emotional symptoms.
Socioeconomic characteristics of children’s families
Our multivariate analyses found an increased risk of abnormal emotional symptoms in children whose families experienced financial difficulties. Children of parents in a low socio-professional category were also the most affected in terms of hyperactivity/inattention. Similar results were recently reported in a French community-based sample of 432 parents and their children during the COVID-19 lockdown14. The authors showed that family socioeconomic factors such as financial difficulties and unemployed parents were significantly associated with a higher risk of children’s mental health problems, such as hyperactivity/inattention and emotional symptoms14. Stability of family income was significantly associated with children's psychological difficulties during the COVID 19 pandemic3, due to economic decline and the stress that it causes70,71.
Our adjusted analysis showed that, compared to living in a rural house, living in an urban house was associated with a lower risk of hyperactivity/inattention during school closure in France. The type of housing was not associated with emotional symptoms in multivariate analysis after an Elastic Net selection. These results are contrary to most studies showing a lower risk of ADHD in children living in rural rather than urban areas72,73. A large web-based survey of 8177 Italian students found that poor housing (i.e., living in apartments < 60 m2 with poor views and poor indoor quality) was associated with an increased risk of depressive symptoms during lockdown74. In addition, an Iranian study which evaluated people's preferences and priorities to choose healthy homes after the COVID-19 pandemic revealed that the most critical priorities for residents were natural light, having a view, acoustic protection, and an open or semi-open space75. Our conflicting results may be explained by the greater proximity to other children in urban than in rural areas.
Contrary to findings in the literature18, our adjusted analysis did not find a significant association between living in one of the regions of France most affected by COVID 19 and children's mental health. Finally, living with both parents was found to be protective for hyperactivity/inattention but not for emotional symptoms. Living with both parents has been shown to be a protective factor for children's mental health in the context of the COVID-19 pandemic, since a Chinese study of 7143 college students found that living with parents was a protective factor against anxiety (OR 0.75; 95% CI 0.60–0.95)3. A recent study on the mental health of children aged 9–18 in France also showed the protective effect of a two-parent family on the psychological distress of children during the COVID-19 pandemic76.
Strengths and limitations
This study has some limitations. First, owing to too many missing data regarding screen time and physical activity, we were unable to estimate the associations between these variables and the presence of hyperactivity/inattention or emotional symptoms in children. The results could be different or even more marked in the general population. Second, only a few parents reported their alcohol and smoking consumption as well as their mental disorders, which prevented us from taking these variables into account in our analyses. Third, we did not have any objective measures of sleep quality but only a parent's self-reported measure of difficulty sleeping. Fourth, we had no data on the consumption of media information related to the pandemic in minutes per day and quality of information received. We did not have access to the children's temperament which has already been shown to be a predictor of emotional disorders and hyperactivity/inattention in children77. It could be interesting for future research to take this variable into account, especially since there is already a validated tool in French78. Therefore, we were not able to study the association between these environmental factors with children's mental health, even though significant associations have already been reported44,53,79. Fifth, our data were collected during a period of school closure in the first COVID-19 wave in France, so we could not analyze data on children's mental health prior to the lockdown. As a result, we were unable to assess the impact of school closure on children's mental health independently from that of the COVID-19 pandemic. Sixth, we could not re-evaluate the mental health of the children, yet it is possible that the reopening of schools in France has resulted in health benefits for them. Future study designs should include re-assessment of mental health and compare children's health scores between countries that implemented vs. did not implement school closure as a preventive measure. Future research should also investigate potential environmental factors that might influence children's mental health, such as parental history of mental illness, consumption of media information related to COVID-19, and domestic violence. In addition, the causal relationship between environmental factors related to COVID-19 and children’s mental health should be explored.
The study also has some strengths. First, it includes the large number of parent respondents during school closures in France at the beginning of the COVID 19 pandemic. It also includes pre-term children, a population more at risk for hyperactivity/inattention, so it provides more power for studying risk and protective factors in a lockdown situation. Second, we were able to control a wide range of possible covariates from sociodemographic and socioeconomic characteristics of children's families to children's schooling. To our knowledge, this is the first study to consider a set of variables related to children's housing and schooling. Third, using validated measures of hyperactivity/inattention and emotional symptoms (SDQ) with satisfactory psychometric properties is a strength and novel aspect of this study31,34. Overall, we believe that our findings contribute to the evolving debate concerning school closure and children's mental health. We suggest that school closure due to COVID-19 could increase the risk of mental health problems and exacerbate health inequalities71. Our findings provide important guidance for the development of children's psychological support strategies in France.
Implications
The current focus on measures to contain COVID-19 transmission around the world may distract attention from emerging mental health issues57,80. The closure of schools due to COVID-19 and the lockdown could lead to an increase in mental disorders in children, especially among vulnerable populations. Efforts must be made to address the pandemic situation while considering children's mental health and to adapt the delivery of care to meet the demands of COVID-1971. Our findings have important clinical and policy implications. In this global public health emergency, identifying vulnerable groups of children and environmental risk factors of children's mental health is a critical step in developing and adapting mental health services and tools81. Health authorities and governments should implement services that improve the mental health of the population, particularly that of vulnerable children. Emerging digital applications such as telehealth, social media, and mobile health could serve to promote children's mental health82.
Conclusion
This study conducted in France explored several risk factors of hyperactivity/inattention and emotional symptoms in children during the school closure due to the COVID-19 pandemic. Some factors that may increase the risk of children developing mental health problems are described: sex, pre-existing health disorders, COVID cases in the household, difficulties in sleeping and in schooling, and sociodemographic and socioeconomic disparities. Policymakers need to balance the pros and cons of reopening school, taking into consideration the educational and psychological consequences for children. Therefore, it is essential to implement appropriate protective measures to manage the unprecedented repercussions of school closure on children's mental health while avoiding an increase in socio-economic inequalities.
Data availability
In regards to data availability, data of the study are protected under the protection of health data regulation set by the French National Commission on Informatics and Liberty (Commission Nationale de l’Informatique et des Libertés, CNIL). The data can be available upon reasonable request after a consultation with the steering committee of the Sapris study. The French law forbids us to provide free access to Sapris data; access could however be given by the steering committee after legal verification of the use of the data.
Abbreviations
- ADHD:
-
Attention-deficit/hyperactivity disorder
- aOR:
-
Adjusted odds ratio
- CART:
-
Classification and regression tree
- CI:
-
Confidence intervals
- OR:
-
Odds ratio
- SDQ:
-
Strength and difficulties questionnaire
- VIP:
-
Variable inclusion probability
References
UNESCO. Education: From Disruption to Recovery. https://en.unesco.org/covid19/educationresponse (UNESCO, 2020).
Antona, D. et al. COVID-19 chez l’enfant (moins de 18 ans). État des lieux de la littérature en amont de la réouverture annoncée des crèches et des écoles. État de la littérature au 24 avril 2020. Synthèse rapide COVID-19. Santé Publique France. /import/covid-19-chez-l-enfant-moins-de-18-ans-.-etat-des-lieux-de-la-litterature-en-amont-de-la-reouverture-annoncee-des-creches-et-des-ecoles.-etat-de-l (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287, 112934 (2020).
Zhou, S. J. et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29(6), 749–758 (2020).
Singh, S. et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 24, 113429 (2020).
Jiao, W. Y. et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 221, 264–266 (2020).
Guessoum, S. B. et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 291, 113264 (2020).
Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C. & Espada, J. P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. PsyArXiv. Preprint at https://psyarxiv.com/5bpfz/ (2020).
Ghosh, R., Dubey, M. J., Chatterjee, S. & Dubey, S. Impact of COVID -19 on children: Special focus on the psychosocial aspect. Minerva Pediatr. 2(3), 226–235 (2020).
De Figueiredo, C. S. et al. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatry 106, 110171 (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet Lond. Engl. 395, 912–920 (2020).
Cleofas, J. V. & Rocha, I. C. N. Demographic, gadget and internet profiles as determinants of disease and consequence related COVID-19 anxiety among Filipino college students. Educ. Inf. Technol. Figshare https://doi.org/10.1007/s10639-021-10529-9 (2021).
Spinelli, M., Lionetti, F., Pastore, M. & Fasolo, M. Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. https://doi.org/10.2139/ssrn.3582790 (2020).
Moulin, F. et al. Risk and protective factors related to children’s symptoms of emotional difficulties and hyperactivity/inattention during the COVID-19-related lockdown in France: Results from a community sample. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01752-3 (2021).
Head, J. R. et al. The effect of school closures and reopening strategies on COVID-19 infection dynamics in the San Francisco Bay Area: A cross-sectional survey and modeling analysis. MedRxiv Prepr. Serv. Health Sci. Figshare https://doi.org/10.1101/2020.08.06.20169797 (2020).
Danis, K. et al. Cluster of Coronavirus Disease 2019 (COVID-19) in the French Alps, February 2020. Clin. Infect. Dis. 71(15), 825–832 (2020).
Ludvigsson, J. F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 109(6), 1088–1095 (2020).
Duan, L. et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 275, 112–118 (2020).
Liu, Q. et al. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in china. J. Affect. Disord. 279, 412–416 (2021).
Tang, S., Xiang, M., Cheung, T. & Xiang, Y. T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent–child discussion. J. Affect. Disord. https://doi.org/10.1016/j.jad.2020.10.016 (2020).
Xie, X. et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 174(9), 898 (2020).
Liu, N. et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 287, 112921 (2020).
Wiguna, T. et al. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front. Psychiatry https://doi.org/10.3389/fpsyt.2020.598756 (2020).
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immunity 89, 531–542 (2020).
Viner, R. M. et al. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 4(5), 397–404 (2020).
COVID-19 and Confinement: A Large-Scale French Survey of Social Challenges and Health INSERM. https://presse.inserm.fr/en/covid-19-and-confinement-a-large-scale-french-survey-of-social-challenges-and-health/39099/ (2020).
Étude Longitudinale Française depuis l’Enfance. Ined Institut National d’études Démographiques. https://www.elfe-france.fr/ (2021).
Charles, M. A. et al. Cohort profile: The French national cohort of children (ELFE): Birth to 5 years. Int. J. Epidemiol. 49(2), 368–369 (2020).
EPIPAGE 2: a preterm birth cohort in France in 2011. BMC Pediatr. https://doi.org/10.1186/1471-2431-14-97 (2021).
Carrat, F. et al. Incidence and risk factors of illnesses presumably caused by a SARS-CoV-2 infection in the general population during the lockdown period: A multi-cohort study. BMC Infect. Dis. https://doi.org/10.21203/rs.3.rs-90873/v1 (2020).
Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 40(11), 1337–1345 (2001).
Goodman, A. & Goodman, R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J. Am. Acad. Child Adolesc. Psychiatry 48(4), 400–403 (2009).
Axford, N. Defining and Classifying Children in Need Vol. 590 (Routledge, 2017).
Hall, C. L. et al. The validity of the strengths and difficulties questionnaire (SDQ) for children with ADHD symptoms. PLoS ONE https://doi.org/10.1371/journal.pone.0218518 (2019).
Shojaei, T., Wazana, A., Pitrou, I. & Kovess, V. The strengths and difficulties questionnaire: Validation study in French school-aged children and cross-cultural comparisons. Soc. Psychiatry Psychiatr. Epidemiol. 44(9), 740–747 (2009).
Thierry, X. et al. Les enfants à l’épreuve du premier confinement. Popul. Soc. 585(1), 1–4 (2021).
Burgette, L. F. & Reiter, J. P. Multiple imputation for missing data via sequential regression trees. Am. J. Epidemiol. 172(9), 1070–1076 (2010).
Zhao, Y. & Long, Q. Variable selection in the presence of missing data: imputation-based methods. Wiley Interdiscip. Rev. Comput. Stat. https://doi.org/10.1002/wics.1402 (2017).
Heymans, M. W., Van Buuren, S., Knol, D. L., Van Mechelen, W. & De Vet, H. C. Variable selection under multiple imputation using the bootstrap in a prognostic study. BMC Med. Res. Methodol. 7, 33 (2007).
Zou, H. & Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. Ser. B Stat. Methodol. 67(2), 301–320 (2005).
Mowlem, F. D. et al. Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. Eur. Child Adolesc. Psychiatry 28(4), 481–489 (2019).
Barriuso-Lapresa, L. M., Hernando-Arizaleta, L. & Rajmil, L. Reference values of the strengths and difficulties questionnaire (SDQ) version for parents in the Spanish population, 2006. Actas Esp Psiquiatr. 42(2), 43–48 (2014).
Laurens, K. R. et al. Middle childhood survey (MCS) of mental health and well-being at age 11 years in an Australian population cohort. BMJ Open https://doi.org/10.1136/bmjopen-2017-016244 (2015).
Hou, F., Bi, F., Jiao, R., Luo, D. & Song, K. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China: A cross-sectional study. BMC Public Health 20(1), 1648 (2020).
Thapar, A. Attention deficit hyperactivity disorder. Lancet 387(10024), 1240–1250 (2016).
Banaschewski, T. et al. Attention-deficit/hyperactivity disorder. Dtsch Ärztebl Int. 114(9), 149–159 (2017).
Faraone, S. V. et al. Attention-deficit/hyperactivity disorder. Nat. Rev. Dis. Primer 1(1), 1–23 (2015).
Montagna, A. & Nosarti, C. Socio-emotional development following very preterm birth: Pathways to psychopathology. Front. Psychol. https://doi.org/10.3389/fpsyg.2016.00080 (2016).
Fountoulakis, K. N. et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J. Affect. Disord. 279, 624–629 (2021).
Franz, A. P. et al. Attention-deficit/hyperactivity disorder and very preterm/very low birth weight: A meta-analysis. Pediatrics https://doi.org/10.1542/peds.2017-1645 (2018).
Linnet, K. M. et al. Gestational age, birth weight, and the risk of hyperkinetic disorder. Arch. Dis. Child. 91(8), 655–660 (2006).
Wang, Z. H. et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. J. Affect. Disord. 275, 188–193 (2020).
Pedrosa, A. L. et al. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front. Psychol. https://doi.org/10.3389/fpsyg.2020.566212 (2020).
Islam, S.M.D.-U., Bodrud-Doza, M., Khan, R. M., Haque, M. A. & Mamun, M. A. Exploring COVID-19 stress and its factors in Bangladesh: A perception-based study. Heliyon 6(7), e04399 (2020).
TMGH-Global COVID-19 Collaborative. Psychological impacts and post-traumatic stress disorder among people under COVID-19 quarantine and isolation: A global survey. Int. J. Environ. Res. Public Health 18(11), 5719 (2021).
Huy, N. et al. Perceived stress of quarantine and isolation during COVID-19 pandemic: A global survey. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.656664 (2021).
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M. & Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 66(4), 317–320 (2020).
Hvolby, A. Associations of sleep disturbance with ADHD: Implications for treatment. Atten. Deficit Hyperact. Disord. 7(1), 1–18 (2015).
Cortese, S., Faraone, S. V., Konofal, E. & Lecendreux, M. Sleep in children with attention-deficit/hyperactivity disorder: Meta-analysis of subjective and objective studies. J. Am. Acad. Child Adolesc. Psychiatry 48(9), 894–908 (2009).
Sadeh, A., Pergamin, L. & Bar-Haim, Y. Sleep in children with attention-deficit hyperactivity disorder: A meta-analysis of polysomnographic studies. Sleep Med. Rev. 10(6), 381–398 (2006).
Reynaud, E., Forhan, A., Heude, B., Charles, M. A. & Plancoulaine, S. Association of night-waking and inattention/hyperactivity symptoms trajectories in preschool-aged children. Sci. Rep. 8(1), 15412 (2018).
Hoffman, J. A. & Miller, E. A. Addressing the consequences of school closure due to COVID-19 on children’s physical and mental well-being. World Med. Health Policy 12, 300–310 (2020).
Bahn, G. H. Coronavirus disease 2019, school closures, and children’s mental health. J. Korean Acad. Child Adolesc. Psychiatry 31(2), 74–79 (2020).
Brown, W. J. et al. A review of sleep disturbance in children and adolescents with anxiety. J. Sleep Res. 27(3), e12635 (2018).
Quach, J. L., Nguyen, C. D., Williams, K. E. & Sciberras, E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 172(2), e174363 (2018).
Nunes, S., Campbell, M. K., Klar, N., Reid, G. J. & Stranges, S. Relationships between sleep and internalizing problems in early adolescence: Results from Canadian National Longitudinal Survey of Children and Youth. J. Psychosom Res. 139, 110 (2020).
Hysing, M., Sivertsen, B., Garthus-Niegel, S. & Eberhard-Gran, M. Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav. Dev. 42, 111–118 (2016).
Catalano, R. et al. The health effects of economic decline. Annu. Rev. Public Health 32(1), 431–450 (2011).
Golberstein, E., Gonzales, G. & Meara, E. How do economic downturns affect the mental health of children? Evidence from the national health interview survey. Health Econ. 28(8), 955–970 (2019).
Wathelet, M. et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open https://doi.org/10.1001/jamanetworkopen.2020.25591 (2020).
Moreno, C. et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 7(9), 813–824 (2020).
Donovan, G. H., Michael, Y. L., Gatziolis, D., Mannetje, A. & Douwes, J. Association between exposure to the natural environment, rurality, and attention-deficit hyperactivity disorder in children in New Zealand: A linkage study. Lancet Planet. Health 3(5), 226–234 (2019).
Knopf, H., Hölling, H., Huss, M. & Schlack, R. Prevalence, determinants and spectrum of attention-deficit hyperactivity disorder (ADHD) medication of children and adolescents in Germany: Results of the German Health Interview and Examination Survey (KiGGS). BMJ Open 2(6), e000477 (2012).
Amerio, A. et al. COVID-19 Lockdown: Housing built environment’s effects on mental health. Int. J. Environ. Res. Public Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7459481/ (2020).
Zarrabi, M., Yazdanfar, S.-A. & Hosseini, S.-B. COVID-19 and healthy home preferences: The case of apartment residents in Tehran. J. Build. Eng. 35, 102021 (2021).
Vandentorren, S. et al. Premiers résultats des facteurs associés à la résilience et à la santé mentale des enfants et des adolescents (9–18 ans) lors du premier confinement lié à la Covid-19 en France. Santé Publique France. /import/premiers-resultats-des-facteurs-associes-a-la-resilience-et-a-la-sante-mentale-des-enfants-et-des-adolescents-9–18-ans-lors-du-premier-confinemen (2021).
Abulizi, X. et al. Temperament in infancy and behavioral and emotional problems at age 5.5: The EDEN mother-child cohort. PLoS ONE 12(2), e0171971 (2017).
Asch, M. et al. Psychometric properties of a French version of the junior temperament and character inventory. Eur. Child Adolesc. Psychiatry 18(3), 144–153 (2009).
Nekliudov, N. A. et al. Excessive media consumption about COVID-19 is associated with increased state anxiety: Outcomes of a large online survey in Russia. J. Med. Internet Res. 22(9), e20955 (2020).
Khan, M. I., Saleem, H. A. R., Anwar, M. F. & Chang, Y.-C. Novel coronavirus and emerging mental health issues—A timely analysis of potential consequences and legal policies perspective. Fudan J. Humanit. Soc. Sci. 14(1), 87–105 (2021).
Fitzpatrick, K. M., Drawve, G. & Harris, C. Facing new fears during the COVID-19 pandemic: The state of America’s mental health. J. Anxiety Disord. 75, 102 (2020).
Ye, J. Pediatric mental and behavioral health in the period of quarantine and social distancing with COVID-19. JMIR Pediatr. Parent. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7389340/ (2020).
Acknowledgements
We are grateful to the New-Aquitaine region and its AMI FLASH Recherche et Innovations COVID, without whom the project would never have started. The authors warmly thank all the volunteers of the ELFE, and EPIPAGE2 cohorts. We thank the staff of the SAPRIS study group that have worked with dedication and engagement to collect and manage the data used for this study and to ensure continuing communication with the cohort participants.
Funding
Sponsor and funding sources played no role in the study design, data collection, analysis, interpretation or drafting of the study. MM and CG had full access to all data in the study. ANR (Agence Nationale de la Recherche, 0009/SAPRIS/997/NB), Fondation pour la Recherche Médicale, Direction Générale de la Recherche et de l'Innovation, Institut Gustave Roussy, the New-Aquitaine region.
Author information
Authors and Affiliations
Consortia
Contributions
M.M. contributed to the literature search, data analysis, and wrote the first draft of the manuscript. C.G., M.M., and A.R. contributed to the data interpretation and writing. S.B., L.M. and T.S. contributed to the data analysis. All authors reviewed the manuscript. C.G. was the senior author of the manuscript. M.M. and C.G. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
Mrs Maeva Monnier has been funded by the New-Aquitaine region (AMI Flash Recherche et Innovations COVID). The other authors declare no competing interests related to this paper.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Monnier, M., Moulin, F., Thierry, X. et al. Children's mental and behavioral health, schooling, and socioeconomic characteristics during school closure in France due to COVID-19: the SAPRIS project. Sci Rep 11, 22373 (2021). https://doi.org/10.1038/s41598-021-01676-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01676-7
This article is cited by
-
Emotional and behavioral changes in French children during the COVID-19 pandemic: a retrospective study
Scientific Reports (2023)
-
The long shadow of the COVID-19 pandemic on children and adolescents’ mental health
European Child & Adolescent Psychiatry (2023)
-
Child health and development in the course of the COVID-19 pandemic: are there social inequalities?
European Journal of Pediatrics (2023)
-
Parents’ depression and anxiety associated with hyperactivity-inattention and emotional symptoms in children during school closure due to COVID-19 in France
Scientific Reports (2023)
-
Effective high-throughput RT-qPCR screening for SARS-CoV-2 infections in children
Nature Communications (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.