Influence of Meteorological Factors on the COVID-19 Transmission with Season and Geographic Location
Abstract
:1. Introduction
2. Data Collection
3. Method
4. Results and Discussion
4.1. The Best-Fitting Model of COVID-19 Infected Cases during the Period of Community-Based Epidemic Prevention and Control
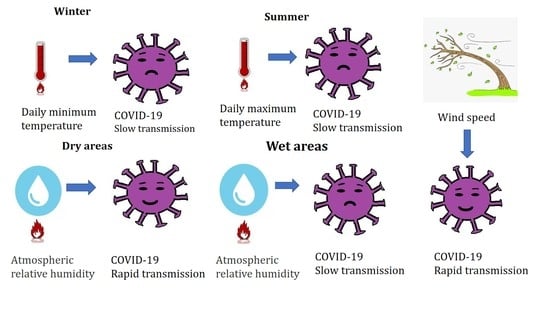
4.2. Influence of Meteorological Factors on COVID-19 Transmission
5. Conclusions and Comments
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Outbreak Situation. Available online: https://www.who.int/ (accessed on 11 November 2020).
- CNR Many Countries in Europe “Closed City”! Why is the Second Outbreak More Serious than the First. Available online: http://www.cnr.cn/ (accessed on 29 October 2020).
- Dhruv, G. Effect of ambient temperature on COVID-19 infection rate. SSRN 2020, 7. [Google Scholar] [CrossRef]
- Qi, H.; Xiao, S.; Shi, R.; Ward, M.P.; Chen, Y.; Tu, W.; Su, Q.; Wang, W.; Wang, X.; Zhang, Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: A time-series analysis. Sci. Total Environ. 2020, 728, 138778. [Google Scholar] [CrossRef] [PubMed]
- Menebo, M.M. Temperature and precipitation associate with Covid-19 new daily cases: A correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020, 737, 139659. [Google Scholar] [CrossRef] [PubMed]
- Bashir, M.F.; Ma, B.; Komal, B.; Bashir, M.A.; Tan, D.; Bashir, M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020, 728, 138835. [Google Scholar] [CrossRef]
- Yao, M.; Zhang, L.; Ma, J.; Zhou, L. On airborne transmission and control of SARS-Cov-2. Sci. Total Environ. 2020, 731, 139178. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, M.; Sharifi, A.; Dorosti, S.; Ghoushchi, S.J.; Ghanbari, N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020, 729, 138705. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S. Effect of meteorological parameters on spread of COVID-19 in India and air quality during lockdown. Sci. Total Environ. 2020, 745, 141021. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Chin, Y.; Huang, J.; He, Y.; Akinwunmi, B.O.; Yu, S.; Zhang, C.J.P.; Ming, W.-K. Meteorological factors and domestic new cases of coronavirus disease (COVID-19) in nine Asian cities: A time-series analysis. medRxiv 2020. [Google Scholar] [CrossRef]
- Auler, A.C.; Cássaro, F.A.M.; Silva, V.O.D.; Pires, L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: A case study for the most affected Brazilian cities. Sci. Total Environ. 2020, 729, 139090. [Google Scholar] [CrossRef]
- Azuma, K.; Kagi, N.; Kim, H.; Hayashi, M. Impact of climate and ambient air pollution on the epidemic growth during COVID-19 outbreak in Japan. Environ. Res. 2020, 190, 110042. [Google Scholar] [CrossRef]
- Pani, S.K.; Lin, N.-H.; RavindraBabu, S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020, 740, 140112. [Google Scholar] [CrossRef] [PubMed]
- Tosepu, R.; Gunawan, J.; Effendy, D.S.; Ahmad, L.O.A.I.; Lestari, H.; Bahar, H.; Asfian, P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020, 725, 138436. [Google Scholar] [CrossRef] [PubMed]
- Haque, S.E.; Rahman, M. Association between temperature, humidity, and COVID-19 outbreaks in Bangladesh. Environ. Sci. Policy 2020, 114, 253–255. [Google Scholar] [CrossRef]
- Shi, P.; Dong, Y.; Yan, H.; Zhao, C.; Li, X.; Liu, W.; He, M.; Tang, S.; Xi, S. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020, 728, 138890. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.L.; Wen, C.L. Meteorological impacts on the incidence of COVID-19 in the U.S. Stoch. Environ. Res. Risk Assess. 2020, 34, 1675–1680. [Google Scholar]
- Guo, X.-J.; Zhang, H.; Zeng, Y.-P. Transmissibility of COVID-19 in 11 major cities in China and its association with temperature and humidity in Beijing, Shanghai, Guangzhou, and Chengdu. Infect. Dis. Poverty 2020, 9, 1–13. [Google Scholar] [CrossRef]
- Méndez-Arriaga, F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020, 735, 139560. [Google Scholar] [CrossRef]
- Şahin, M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020, 728, 138810. [Google Scholar] [CrossRef]
- Bolaño-Ortiz, T.R.; Camargo-Caicedo, Y.; Puliafito, S.E.; Ruggeri, M.F.; Bolaño-Diaz, S.; Pascual-Flores, R.; Saturno, J.; Ibarra-Espinosa, S.; Mayol-Bracero, O.L.; Torres-Delgado, E.; et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: A look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020, 191, 109938. [Google Scholar] [CrossRef]
- Lolli, S.; Chen, Y.-C.; Wang, S.-H.; Vivone, G. Impact of meteorological conditions and air pollution on COVID-19 pandemic transmission in Italy. Sci.Rep. 2020, 10, 16213. [Google Scholar] [CrossRef]
- Ali, K. Coronavirus Infectious Disease (COVID-19) Modeling: Evidence of Geographical Signals. SSRN 2020, 7, 3568425. [Google Scholar] [CrossRef]
- Wang, M.; Jiang, A.; Gong, L.; Luo, L.; Guo, W.; Li, C.; Zheng, J.; Li, C.; Yang, B.; Zeng, J.; et al. Temperature Significant Change COVID19 Transmission in 429 Cities. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Ahlawat, A.; Wiedensohler, A.; Mishra, S.K. An Overview on the Role of Relative Humidity in Airborne Transmission of SARS-CoV-2 in Indoor Environments. Aerosol. Air Qual. Res. 2020, 20, 1856–1861. [Google Scholar] [CrossRef]
- Yang, W.; Marr, L.C. Dynamics of Airborne Influenza A Viruses Indoors and Dependence on Humidity. PLoS ONE 2011, 6, e21481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhardwaj, R.; Agrawal, A. Likelihood of survival of coronavirus in a respiratory droplet deposited on a solid surface. Phys. Fluids 2020, 32, 061704. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007, 3, e151. [Google Scholar] [CrossRef] [PubMed]
- Polozov, I.V.; Bezrukov, L.; Gawrisch, K.; Zimmerberg, J. Progressive ordering with decreasing temperature of the phospholipids of influenza virus. Nat. Chem. Biol. 2008, 4, 248–255. [Google Scholar] [CrossRef] [Green Version]
- Kumar, M.; Mazumder, P.; Mohapatra, S.; Thakur, A.K.; Dhangar, K.; Taki, K.; Mukherjee, S.; Patel, A.K.; Bhattacharya, P.; Mohapatra, P. A chronicle of SARS-CoV-2: Seasonality, environmental fate, transport, inactivation, and antiviral drug resistance. J. Hazard. Mater. 2020, 124043. [Google Scholar] [CrossRef]
- Audi, A.; AlIbrahim, M.; Kaddoura, M.; Hijazi, G.; Yassine, H.M.; Zaraket, H. Seasonality of Respiratory Viral Infections: Will COVID-19 Follow Suit? Front. Public Health 2020, 8, 576184. [Google Scholar] [CrossRef]
- Bu, J.; Peng, D.-D.; Xiao, H.; Yue, Q.; Han, Y.; Lin, Y.; Hu, G.; Chen, J. Analysis of meteorological conditions and prediction of epidemic trend of 2019-nCoV infection in 2020. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Luo, W.; Majumder, M.; Liu, D.; Poirier, C.; Mandl, K.; Lipsitch, M.; Santillana, M. The role of absolute humidity on transmission rates of the COVID-19 outbreak. SSRN 2020. [Google Scholar] [CrossRef]
- NHC November 11: Daily Briefing on Novel Coronavirus Cases in China. Available online: http://en.nhc.gov.cn/index.html (accessed on 11 November 2020).
- Chen, D.; Yang, Y.; Zhang, Y.; Yu, W. Prediction of COVID-19 spread by sliding mSEIR observer. Inf. Sci. 2020, 63, 222203. [Google Scholar] [CrossRef]
- Delamater, P.L.; Street, E.J.; Leslie, T.F.; Yang, Y.T.; Jacobsen, K.H. Complexity of the basic reproduction number (R0). Emerg. Infect. Dis. 2019, 25, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, Z.; Song, W.; Ding, Z.; Guan, Q.; Yang, X.; Xu, Q.; Wang, X.; Xia, Y. Linking key intervention timings to rapid declining effective reproduction number to quantify lessons against COVID-19. Front. Med. 2020, 14, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Al-Khani, A.M.; Khalifa, M.A.; Almazrou, A.; Saquib, N. The SARS-CoV-2 pandemic course in Saudi Arabia: A dynamic epidemiological model. Infect. Dis. Model. 2020, 5, 766–771. [Google Scholar]
- Postavaru, O.; Anton, S.; Toma, A. COVID-19 pandemic and chaos theory. Math. Comput. Simul. 2020, 181, 138–149. [Google Scholar] [CrossRef]
- Pei, T.; Wang, X.; Song, C.; Liu, Y.; Huang, Q.; Shu, H.; Chen, X.; Guo, S.; Zhou, C. Review on spatiotemporal analysis and modeling of COVID-19 pandemic. J. Geo-Inform. Sci. 2021, 23. [Google Scholar] [CrossRef]
- Dalziel, B.D.; Pourbohloul, B.; Ellner, S.P. Human mobility patterns predict divergent epidemic dynamics among cities. Proc. R. Soc. B Biol. Sci. 2013, 280, 20130763. [Google Scholar] [CrossRef]
- Soebiyanto, R.P.; Adimi, F.; Kiang, R.K. Modeling and predicting seasonal influenza transmission in warm regions using climatological parameters. PLoS ONE 2010, 5, 0009450. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Zhou, J.; Yao, J.; Zhang, X.; Li, L.; Xu, X.; He, X.; Wang, B.; Fu, S.; Niu, T. Impact of meteorological factors on the COVID-19 transmission: A multi-city study in China. Sci. Total Environ. 2020, 726, 138513. [Google Scholar] [CrossRef]
- Eames, I.; Tang, J.; Li, Y.; Wilson, P. Airborne transmission of disease in hospitals. R. Soc. 2009, 6, 691–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, I.T.S.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.W.; Leung, D.Y.C.; Ho, T. Evidence of Airborne Transmission of the Severe Acute Respiratory Syndrome Virus. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zoran, M.A.; Savastru, R.S.; Savastru, D.M.; Tautan, M.N. Assessing the relationship between surface levels of PM2. 5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020, 738, 139825. [Google Scholar] [CrossRef] [PubMed]
- Woese, C. Thermal inactivation of animal viruses. Ann. N. Y. Acad. Sci. 1960, 83, 741–751. [Google Scholar] [CrossRef]
- Nielsen, J.; Mazick, A.; Glismann, S.; Mølbak, K. Excess mortality related to seasonal influenza and extreme temperatures in Denmark, 1994-2010. BMC Infect. Dis. 2011, 11, 350. [Google Scholar] [CrossRef] [Green Version]
- Cervino, G.; Fiorillo, L.; Surace, G.; Paduano, V.; Fiorillo, M.T.; De Stefano, R.; Laudicella, R.; Baldari, S.; Gaeta, M.; Cicciù, M. SARS-CoV-2 Persistence: Data Summary up to Q2 2020. Data 2020, 5, 81. [Google Scholar] [CrossRef]
- Behnood, A.; Golafshani, E.M.; Hosseini, S.M. Determinants of the infection rate of the COVID-19 in the US using ANFIS and virus optimization algorithm (VOA). Chaos Solitons Fractals 2020, 139, 110051. [Google Scholar] [CrossRef]
- Tobías, A.; Molina, T. Is temperature reducing the transmission of COVID-19? Environ. Res. 2020, 186, 109553. [Google Scholar] [CrossRef]
- Liu, X.; Dong, B. Influence of the Tibetan Plateau uplift on the Asian monsoon-arid environment evolution. Chin. Sci. Bull. 2013, 58, 4277–4291. [Google Scholar] [CrossRef] [Green Version]
- Casanova, L.M.; Jeon, S.; Rutala, W.A.; Weber, D.J.; Sobsey, M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010, 76, 2712–2717. [Google Scholar] [CrossRef] [Green Version]
- Chan, K.-H.; Peiris, J.M.; Lam, S.; Poon, L.L.; Yuen, K.-Y.; Seto, W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Munster, V. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Eurosurveillance 2013, 18, 20590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moeller, P.W.; Fields, P.A.; Dutson, T.R.; Landmann, W.A.; Carpenter, Z.L. Effect of high temperature conditioning on subcellular distribution and level of lysosomal enzymes. J. Food Sci. 1976, 41, 216–217. [Google Scholar] [CrossRef]
- Yuan, J.; Yun, H.; Lan, W.; Wang, W.; Sullivan, S.G.; Jia, S.; Bittles, A.H. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Control 2006, 34, 234–236. [Google Scholar] [CrossRef] [PubMed]


| Cites | Season | Duration of COVID-19 Outbreaks | Duration of Community Control | Cumulative Number of the Confirmed Cases (N) | Cumulative Number of the Asymptomatic Infected Persons (N) |
|---|---|---|---|---|---|
| Wuhan | Winter | 8 December 2019–23 March 2020 | 11 February 2020–27 March 2020 | 68,100 | NA |
| Harbin | Spring | 10 April 2020–21 May 2020 | 12 April 2020–10 June 2020 | 66 | 26 |
| Beijing | Summer | 11 June 2020–6 August 2020 | 13 June 2020–6 July 2020 | 335 | 53 |
| Urumqi | Summer | 15 July 2020–7 September 2020 | 13 July 2020–23 August 2020 | 828 | 390 |
| Dalian | Summer | 22 July 2020–23 August 2020 | 22 July 2020–20 August 2020 | 92 | 97 |
| Qingdao | Autumn | 11 October 2020–12 November 2020 | 12 October 2020–26 October 2020 | 13 | 8 |
| Kashgar | Autumn | 24 October 2020–at present | 24 October 2020–at present | 81 | 423 |
| Models | Equations | Wuhan | Beijing | Urumqi | Dalian | ||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | p | R2 | p | R2 | p | R2 | p | ||
| Gaussian model | 0.88 | <0.01 | 0.74 | <0.01 | 0.78 | <0.01 | 0.48 | <0.01 | |
| Logistic model | NA | NA | 0.67 | <0.01 | NA | NA | NA | NA | |
| Lognormal distribution model | 0.89 | <0.01 | 0.89 | <0.01 | 0.79 | <0.01 | 0.86 | <0.01 | |
| Allometric model | 0.02 | <0.01 | 0.21 | <0.01 | 2.27 × 10−5 | <0.01 | 0.11 | <0.01 | |
| City | Tmax (°C) | Tmin (°C) | DTR (°C) | Tm (°C) | RH (%) | MWS (m·s−1) | TP (mm) |
|---|---|---|---|---|---|---|---|
| Wuhan (January–March) | −0.42 * | −0.55 ** | 0.12 | −0.53 ** | 0.15 | 0.13 | 0.34 |
| Beijing (June–July) | 0.36 | 0.14 | 0.24 | 0.31 | −0.67 ** | 0.65 ** | −0.25 |
| Urumqi (July–August) | −0.22 | −0.47 ** | 0.29 | −0.39 ** | 0.42 * | −0.04 | 0.21 |
| Dalian (July–August) | −0.27 | −0.02 | 0.11 | −0.11 | −0.65 ** | −0.33 | 0.22 |
| City | Regression Equation | R2 | p-Values |
|---|---|---|---|
| Wuhan (January–March) | Y = 897.06 − 73.24XTmin | 0.30 | <0.001 |
| Beijing (June–July) | Y = 142.10 − 3.32XTm − 0.87XRH + 1.65XMWS | 0.68 | <0.001 |
| Urumqi (July–August) | Y = -293.62 + 7.19XTmax + 2.94XRH | 0.27 | <0.05 |
| Dalian (July–August) | Y = 121.01 − 5.72XTmax + 6.72XTmin − 1.30XRH | 0.75 | <0.001 |
| Meteorological Factor | Cites | Statistical Parameter | ||||
|---|---|---|---|---|---|---|
| Wuhan (January–March) | Beijing (June–July) | Urumqi (July–August) | Dalian (July–August) | F | p-Value | |
| Tmax (°C) | 15.52 ± 4.40c | 31.34 ± 2.57a | 29.67 ± 2.76a | 27.41 ± 1.90b | 144.39 | <0.001 |
| Tmin (°C) | 6.47 ± 4.30c | 21.84 ± 1.87a | 19.95 ± 2.84b | 22.61 ± 0.83a | 173.34 | <0.001 |
| DTR (°C) | 9.05 ± 4.15c | 9.50 ± 2.77b | 9.72 ± 2.45a | 4.80 ± 1.66d | 9.64 | <0.001 |
| Tm (°C) | 10.87 ± 3.93d | 26.73 ± 2.01a | 24.83 ± 2.59b | 24.69 ± 1.24c | 193.43 | <0.001 |
| RH (%) | 76.49 ± 8.82a | 54.91 ± 13.87b | 40.60 ± 9.34c | 79.67 ± 10.85a | 78.52 | <0.001 |
| MWS (m·s−1) | 1.29 ± 0.97d | 6.41 ± 2.51a | 2.73 ± 0.72c | 3.08 ± 1.76b | 51.89 | <0.001 |
| TP (mm) | 3.21 ± 6.96a | 1.13 ± 5.38a | 1.13 ± 3.23a | 2.25 ± 6.11a | 0.96 | 0.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.-D.; Li, H.-L.; Cao, Y.-E. Influence of Meteorological Factors on the COVID-19 Transmission with Season and Geographic Location. Int. J. Environ. Res. Public Health 2021, 18, 484. https://doi.org/10.3390/ijerph18020484
Yang X-D, Li H-L, Cao Y-E. Influence of Meteorological Factors on the COVID-19 Transmission with Season and Geographic Location. International Journal of Environmental Research and Public Health. 2021; 18(2):484. https://doi.org/10.3390/ijerph18020484
Chicago/Turabian StyleYang, Xiao-Dong, Hong-Li Li, and Yue-E Cao. 2021. "Influence of Meteorological Factors on the COVID-19 Transmission with Season and Geographic Location" International Journal of Environmental Research and Public Health 18, no. 2: 484. https://doi.org/10.3390/ijerph18020484