Psychologic Stress of COVID-19 Pandemic and Oral Health: A Case Series
Article Information
Wendy Fu1, Raime Shah2, Donald A Curtis1, Yvonne Kapila2*
1Preventive and Restorative Dental Sciences, Division of Prosthodontics, School of Dentistry, University of California, San Francisco, California, United States
2Department of Orofacial Sciences, Division of Periodontology, School of Dentistry, University of California, San Francisco, California, United States
*Corresponding Authors: Yvonne L Kapila, Professor and Chair of Periodontology, Division of Periodontology, Department of Orofacial Sciences, University of California, San Francisco, 513 Parnassus Avenue, S616C, Box 0422, San Francisco, CA 94143, USA
Received: 20 July 2021; Accepted: 14 September 2021; Published: 07 October 2021
Citation: Wendy Fu, Raime Shah, Donald A Curtis, Yvonne Kapila. Psychologic Stress of COVID-19 Pandemic and Oral Health: A Case Series. Archives of Clinical and Medical Case Reports 5 (2021): 672-679.
View / Download Pdf Share at FacebookAbstract
Introduction: High stress levels associated with the COVID-19 pandemic may be a risk factor for accelerating inflammatory disease processes, such as periodontitis and peri-implant disease, and parafunctional activities, such as bruxism.
Case Presentation: The purpose of this report is to outline unique clinical examples of complications observed in our clinics during the COVID-19 pandemic, review potential mechanisms of action, and offer general recommendations.
Conclusions: The consideration of how high levels of psychologic stress might impact patient management is relevant.
Keywords
Psychologic Stress; COVID-19; Periodontal Disease; Peri-Implantitis; Bruxism; Oral Health
Psychologic Stress articles; COVID-19 articles; Periodontal Disease articles; Peri-Implantitis articles; Bruxism articles; Oral Health articles
Article Details
1. Background
The COVID-19 pandemic resulted in significant health concerns related to stress, anxiety, insomnia, and anger [1]. In a recent meta-analysis, prevalence of stress symptoms in the general population was estimated at nearly 25% [2]. As the reciprocal interaction between mental and physical health is better understood, the negative impact of stress on oral health is more often reported [3-6]. Psychological stress can directly and indirectly impact oral health, manifesting as biological and mechanical complications [6, 7]. The biological mechanisms involve increasing cytokines and pro-inflammatory mediators in the gingival crevicular fluid [3, 6], dysregulation of the hypothalamic-pituitary-adrenal axis [8], and catecholamine release from the adrenal medu-lla favoring growth of pathogenic microbiota [6]. Some of these same biological responses to stress can contribute to parafunctional activities, increasing mechanical complica-tions. The purpose of this report is to outline unique clinical examples of complications seen in our clinics during the COVID-19 pandemic, review potential mechanisms of action, and offer general recommendations.
2. Clinical Presentation
2.1 Case 1
A 69-year-old Hispanic female with a medical history significant for liver transplant with Tacrolimus use, hypercholesterolemia, hypertension, and type II diabetes presented to the University of California, San Francisco (UCSF) Postgraduate Periodontics Clinic in 2019. Initial treatment was proposed to address localized 5-6mm probing depths (Figure 1a). Due to COVID-19 pandemic, treatment was delayed. When the patient was seen for an emergency exam in September 2020, she presented with multiple gingival micro-ulcerations, pain on biting, and extensive vertical bony defects (Figure 1b). Teeth with a previously questionable prognosis were then deemed hopeless, thereby requiring extraction. Patient reported her HbA1c had been well-controlled at 7.4-7.7% from March 2019 to October 2020.
2.2 Case 2
A 55-year-old Caucasian female presented to the Postgraduate Prosthodontics Clinic for fabrication of a new maxillary implant-supported partial denture. The patient’s medical history was non-contributory. She reported history of smoking and quitting in 2010. The patient had a history of previously treated periodontal disease and was compliant with periodontal maintenance. Following bilateral maxillary lateral window sinus lift procedures, implants (Astra Osseospeed TX) were placed in site #4, 12, and 14 in November 2011 and in site #5 in December 2014. Implants healed uneventfully and locator abutments were used for an implant-supported partial denture (Figure 2a). Slight marginal bone loss was first noted around #12,14 implants in April 2019 (Figure 2b). When the patient presented to the Postgraduate Periodontics Clinic in August 2020 with emergent sinus symptoms, implants #4,5, and 14 demonstrated >50% radiographic bone loss, probing depths >7mm, bleeding on probing, suppuration, and pain on palpation (Figure 2c).
2.3 Case 3
A 75-year-old Asian male presented to the Postgraduate Prosthodontics Clinic for evaluation of fractured implant restorations at site #12,13. The patient was in good general health. In 2016, the patient had implants (Nobel Replace Straight Groovy Narrow Platform 3.5mm diameter) placed in site #12,13. In 2017, individual screw-retained custom abutments were designed for a cement-retained fixed dental prosthesis (Figure 3). For three years the patient was seen for periodic recall without significant findings. In December 2020, the patient presented with fractured abutment screws and fractured implant abutments dislodged inside of the cemented restorations (Figures 4, 5). Patient denied wearing an occlusal splint.
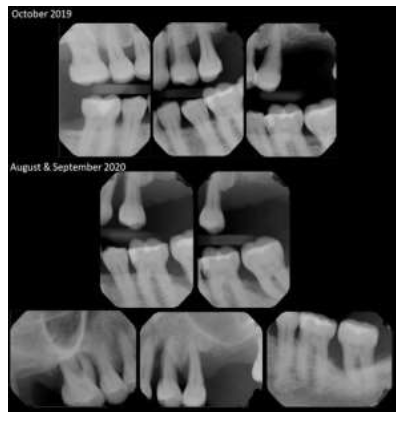
Figure 1a (top): Radiographs of initial presentation (October 2019) with generalized horizontal attachment loss and localized 5-6mm pocket depth.
Figure 1b (bottom): Radiographs of presentation during COVID-19 pandemic (August and September 2020), with vertical bony defects extending to the apex of teeth #3,12,13,18.

Figure 2a (top): Radiographs of #4,5 implants after delivery of Locator abutments.
Figure 2b (middle): Radiographs demonstrating first sign of marginal bone loss around implants #4,5.
Figure 2c (bottom): Radiographs during COVID-19 pandemic, demonstrating >50% marginal bone loss.

Figure 3:Screw-retained custom abutments delivered for implants #12,13.
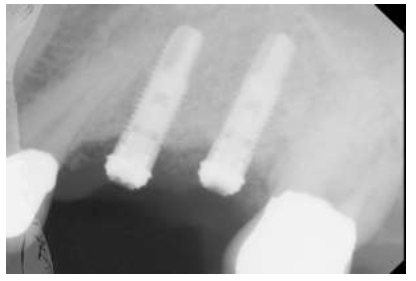
Figure 4: Radiograph during COVID-19 pandemic, of fractured abutment screws and fractured implant abutments.

Figure 5: Fractured custom abutments are retained inside of splinted PFM restorations.
3. Case Management
3.1 Case 1
Patient was diagnosed with localized chronic periodontitis (localized stage III grade C). Following extractions and scaling and root planing, further treatment was delayed in December 2020 due to her positive COVID-19 diagnosis and subsequent hospitalization. When patient returned to clinic, additional teeth were deemed hopeless. On the Perceived Stress Scale [9], the patient scored 7. This score is lower than averages for her gender, age, and race. However, patient reported periods of heightened stress during the pandemic. Positive COVID-19 diagnosis and psychosocial factors may be implicated as risk factors for her rapidly deteriorating condition.
3.2 Case 2
Patient was diagnosed with peri-implantitis. Implants #4,5,14 demonstrated significant circumferential crater defects and were eventually removed (Figures 6, 7). The patient reported no changes in medical history, aside from increased stress during the pandemic. On the Perceived Stress Scale [9], the patient scored 20. This score is significantly higher than averages for her gender, age, and race. The accelerated osseous breakdown may be associated with a history of treated periodontitis, missed maintenance appointments, and heightened stress during the pandemic.
3.3 Case 3
The patient is treatment planned for removal of the fractured abutment screws, fabrication of a new splinted screw-retained prosthesis, and delivery of an occlusal splint. As the patient did not undergo any known changes in his health history, we considered the heightened stress during the pandemic as a possible contributing factor to his prosthetic complication.

Figure 6: #4 implant demonstrating significant circumferential crater defects with greater than 50% bone loss.
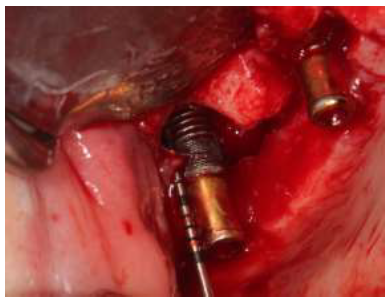
Figure 7: #5 implant demonstrating significant circumferential crater defects with greater than 50% bone loss and communication with right maxillary sinus.
4. Discussion
The objective of this case series was to highlight three clinical cases that took place during the COVID-19 pandemic and to instigate conversations around impacts of psychological stress on oral health during the pandemic. Psychological stress may be considered a risk factor in the development of biologic complications, including accelerated progression of periodontitis and peri-implantitis [4, 10]. There are three main proposed mechanisms of action of stress on predisposition, precipitation, perpetuation, and exacerbation of disease [11].
First, stress is associated with an increase in inflammatory mediators, which are found in the gingival crevicular fluids and are elevated in active periodontitis [12]. Second, stress activates the hypothalamic-pituitary-adrenal axis and results in elevated cortisol levels [6]. In the progression of periodontitis, cortisol has both direct and indirect effects on microbial biofilms, resulting in dysbiosis [13]. Third, the release of epinephrine from adrenal medulla can also shift biofilms towards oral dysbiosis [6]. Psychological stress is one of the risk factors associated with bruxism [14]. In bruxers, studies have found higher levels of cortisol and stress as compared to non-bruxers [7]. Bruxism has significant implications for implant restorations, leading to reversible and irreversible outcomes, including ceramic fracture, prosthetic screw loosening, and fracture of implant components [15].
In conclusion, we should recognize the psychological impact of the COVID-19 pandemic on our patients. Patients at high risk should be monitored closely for progression of periodontitis and peri-implantitis, and patients with implant restorations should be evaluated for need of occlusal guard. Lastly, the importance of enhanced oral hygiene and compliance with recall appointments should be emphasized.
Informed Consent
Written informed consent was obtained from all individual participants included in these case reports.
Conflict of Interest
The authors declare no competing interests.
Disclaimer
None.
References
- Jones NM, Thompson RR, Dunkel Schetter C, et al. Distress and rumor exposure on social media during a campus lockdown. Proc Natl Acad Sci U S A 114 (2017): 11663-11668.
- Cooke JE, Eirich R, Racine N, et al. Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Res 292 (2020): 113347.
- Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A 109 (2012): 5995-5999.
- Decker A, Askar H, Tattan M, et al. The assessment of stress, depression, and inflammation as a collective risk factor for periodontal diseases: a systematic review. Clin Oral Investig 24 (2020): 1-12.
- Decker A, Kapila Y, Wang HL. The psychobiological links between chronic stress-related diseases, periodontal/peri-implant diseases, and wound healing. Periodontol (2000).
- Spector AMP T T, Akram F, Scott A J, et al. Psychological Stress: A Predisposing and Exacerbating Factor in Periodontitis. Current Oral Health Reports 7 (2020): 208-215.
- Karakoulaki S, Tortopidis D, Andreadis D, et al. Relationship Between Sleep Bruxism and Stress Determined by Saliva Biomarkers. Int J Prosthodont 28 (2015): 467-474.
- Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2000 62 (2013): 59-94.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 24 (1983): 385-396.
- Castro MML, Ferreira RO, Fagundes NCF, et al. Association between Psychological Stress and Periodontitis: A Systematic Review. Eur J Dent 14 (2020): 171-179.
- Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol 5 (2005): 243-251.
- Masada MP, Persson R, Kenney JS, et al. Measurement of interleukin-1 alpha and -1 beta in gingival crevicular fluid: implications for the pathogenesis of periodontal disease. J Periodontal Res 25 (1990): 156-163.
- Akcali A, Huck O, Tenenbaum H, et al. Periodontal diseases and stress: a brief review. J Oral Rehabil 40 (2013): 60-68.
- Kuhn M, Turp JC. Risk factors for bruxism. Swiss Dent J 128 (2018): 118-124.
- Manfredini D, Poggio CE, Lobbezoo F. Is bruxism a risk factor for dental implants? A systematic review of the literature. Clin Implant Dent Relat Res 16 (2014): 460-469.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
