Abstract
World is under threat of COVID-19 pandemic, associated with many numbers of critically ill patients. To manage these intubated patients there are need of more ventilators but world is not prepared for this type of situation and there are lacunae of such arrangements in most of the countries. As we know patients cannot be intubated for long time and they should be given preference to alternative airway in the form of tracheostomy. COVID-19 is aerosol transmitted disease which lead to indeed challenge to health care providers to safely perform tracheostomy and provide post tracheostomy care to these patients with minimising risks of nosocomial transmission to themselves and accompanying nursing staff. There are so many guidelines and recommendations for the timing, desired place of tracheostomy, change in tracheostomy steps related to conventional method and the subsequent management of patients. So, the aim of this systematic review is to give a brief review of available data on COVID-19 related to the timing, personal protections, operative steps modifications, and subsequent post tracheostomy care during this pandemic.
Similar content being viewed by others
Introduction
The COVID-19 pandemic caused by the SARS-CoV-2 virus is big health related issue faced by many doctors across world since it began in late 2019 [1]. Till date COVID-19 has infected more than 30.6 million people and cause 950 000 deaths [2]. The Doctors are in search for definite treatment and methods for reduction of transmission. Tracheostomies are commonly done in critically ill patients which are on mechanical ventilation to facilitate their weaning from ventilation and to increase the availability of intensive care unit (ICU) beds for new infected patients. However, as we know tracheostomy is an aerosol generating procedure, so health-care workers are at risk of infection during procedure and post tracheostomy care even though appropriate personal protective equipment (PPE) is used. So COVID-19 positive patients are challenge for tracheostomy procedure to be done safely. There are many Conflicting recommendations exist about the timing, ideal place, performance of tracheostomy and the subsequent management of patients.
Methodolgy
The report of this systematic review was made according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Fig 1). The review protocol was not previously registered. MEDLINE (accessed from PubMed) from 6 august 2019 to 7 august 2020 were systematically searched for related published articles. In electronic databases, the following search strategy was implemented and these key words (in the title/abstract) were used: “COVID 19” OR “CORONAVIRUS” OR “SARS COV-2” AND “TRACHEOSTOMY”. Articles written in English and available full text were all included in this search. All authors participated through each phase of the review independently (screening, eligibility, and inclusion) .They independently screened the titles and abstracts yielded by the search against the inclusion criteria. They resolved any disagreement through discussions. Neither of the authors were blind to the journal titles or to the study authors or institutions. The following data were extracted from the included studies: study authors, study designs, main results. We included only human studies and articles with clearly defined clinical outcome. The exclusion criteria was animal studies and review articles. The search was performed at specified date and time on 7/08/2020 at 11:30 Am.
Results
Total of 56 full article studies were obtained on PubMed database search, out of which 40 studies were excluded due to not relevant title, not relevant content, review articles, head neck oncology related tracheostomy. Finally, we reviewed the final 15 articles based on our selection criteria to extract the following information from each: first author, date of publication, study design, main results data related to tracheostomy guidelines for COVID-19. The extracted data is jotted in Table 1.
Discussion
General Recommendations for Tracheostomy in COVID-19 positive Patients based on systemic analysis of included articles are developed as under in different headings:
Timing of Tracheostomy
Timing of tracheostomy should be between ventilator [post intubation] days 14–21 when viral load is expected to be decreasing and 21–30 days after onset of symptoms.
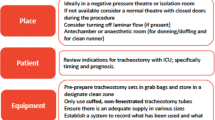
Place of Procedure
The ideal location for performing a tracheostomy on a COVID-19 positive patient should be an isolated room with lower pressure than the corridor with closed doors-windows and no laminar flow. If not possible, Operating room or ICU room with negative pressure using a portable high efficiency particulate air (HEPA) filtration system can be beneficial.
Preparation and Safety
Personal protective equipment-PPE should include: Fitted respiratory mask [N95 OR PAAR OR PFF3], surgical cap, impermeable sterile gown, shoe covers, goggles, and full-face shields, sterile double gloves and additional surgical mask (in front of the N95 or PFF3). There should be minimum number of people in the room (2 procedural staff-ENT surgeon and anaesthetic). Use only a conventional cuffed tracheostomy tube, avoiding the fenestrated models. If shifting of patient is needed to isolated room or operating room then do deep suctioning of the chest and oral cavity using the closed suctioning circuit to reduce the amount of secretions at the time of opening the trachea. During transfer of patient, Security staff should have to close the corridor temporarily and the patient should be transferred along the back corridor of the theatre [not through the main theatre entrance] and transfer team should have to take all personal protection measures.
Operative Steps/Technique Modification
-
Deep neuromuscular blockade and sedatives should be given for adequate paralysis with glycopyrrolate to reduce tracheal secretions.
-
Avoid electrocautery usage during tracheostomy procedure to reduce risk of smoke formation and viral transmission via aerosol. After trachea identification, Pre oxygenate the intubated patient with PEEP and then stop ventilation and turn off flows of ventilation.
-
Allow time for passive expiration with open APL valve.
-
To avoid the aerosol transmission- clamp ET tube, deflate cuff and push down the ET tube beyond [up to carina] the site chosen for the tracheal stoma at the beginning of the procedure.
-
Create appropriate tracheal window opening, deflate the cuff of ET tube and pull the ET tube until the tip is proximal to the tracheal window opening.
-
Tracheal or wound suctioning of blood or secretions should not be done, to avoid aerosol generation.
-
Insert the tracheostomy tube quickly into the opening, inflate tracheostomy tube cuff almost simultaneously and the tracheostomy tube is rapidly connected to the ventilator with immediate resumption of the ventilation.
-
Confirm position of the tracheostomy tube with end tidal CO2 only to avoid contamination of stethoscope by auscultation.
-
An HME type filter (Heat and moisture exchanger) must be placed on the tracheostomy tube to reduce the exposure of the virus, in case of accidental disconnection of circuit and if patient is not on mechanical ventilation.
-
Suspension of ventilation support should be minimum, with satisfactory oxygen saturation [do quick tracheostomy].
Post Procedural care and Rehabilitation
-
Team involved in the procedure should use a shower for body cleaning.
-
Avoid humidified oxygen, use only HME filters.
-
Do suctioning always in a closed circuit.
-
Tracheostomy Cuff should be always inflated.
-
Avoid tracheostomy stoma dressing changes unless there are clear signs of infection.
-
Avoid tracheostomy tube change before 7–10 days, giving preference to a period of lower viral load. During tracheostomy tube change the anaesthesiologist should have to sedate the patient and perform a neuromuscular block to reduce any risk of coughing.
-
Follow same sequence of pause in ventilation with flows off before deflating cuff and inserting new tube with immediately re-inflation of cuff and reconnection of circuit.
-
Use full PPE for tracheostomy tube change.
-
Next Subsequent planned tube change should be at least 30 days interval.
-
Patients not on a closed ventilation circuit should wear a surgical mask over their stoma if tolerated as this may decrease spread of droplets from leakage around the stoma and/or HME. Use Closed circuit with HEPA filter if on mechanical ventilatory support.
-
Manipulation of the tracheostomy site should be minimized. Use of tracheostomy tube without fenestrations until the COVID exam is negative.
-
All nonurgent clinic visits should be postponed and/or converted to telehealth visits when possible.
-
Nebulizer treatments should be avoided to minimize risk of aerosolization.
-
All disposable material that has been in contact with the cannula or trachea (filters, suction probes) during the post-tracheostomy care must be eliminated through the infectious waste circuit.
-
Avoid circuit disconnection as much as possible during tracheostomy and post tracheostomy care.
Conclusion
Our recommendations on the use of tracheostomy during the COVID-19 pandemic are presented in above mentioned panel. There are limited data related to corona virus infectivity risk in each step of tracheostomy and many other questions remain unanswered which require prospective analysis in near future. Increases in the number of patients with COVID-19 positive status requiring long term ventilation will definitely require tracheostomy to facilitate recovery. As we know Tracheostomies in COVID-19 patients are extremely high-risk procedures for all members of the procedural team. At present, there is no high-level evidence upon which to make definitive recommendations, but we have made our proposed recommendations based on currently available literature to form a safe approach which would be helpful to involved physicians in management of critically ill COVID-19 patients. It is advised for every institution to make its own guidelines for tracheostomy in COVID-19 and follow strictly. There is no doubt that as more rapidly emerging higher-level evidence becomes available and our recommendations will be refined and improved.
Abbreviations
- PAPR:
-
Powered air purifying respirators
- PPE:
-
Personal protective equipment
- HME:
-
Heat and Moisture exchanger
- HEPA:
-
High efficiency particulate air
- PEEP:
-
Positive end expiratory pressure
- APL:
-
Adjustable pressure limiting valve
- ET:
-
Endotracheal tube
- DOP:
-
Date of publication
References
Zhu N, Zhang D, Wang W et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019 N Engl J Med https://doi.org/10.1056/NEJMoa2001017
World Health Organization (WHO) Coronavirus disease (COVID-19) Pandemic Weekly update on 20 september at 10 am
Menegozzo CA, Arap SS, Mariani AW, Minamoto H, Imamura R, Bento RF, Pêgo-Fernandes PA, Kowalski LP, Utiyama E (2020) Standardization of elective tracheostomies at the Central Institute of the Hospital das Clínicas in São Paulo during the COVID-19 pandemic. Revista do Colégio Brasileiro de Cirurgiões, 47
Jacob T, Walker A, Mantelakis A, Gibbins N, Keane O (2020) A framework for open tracheostomy in COVID-19 patients Clin Otolaryngol 45:649–651
Lima DS, Junior MF, Vieira-Jr HM, de Campos T, Di Saverio S. Alternatives for establishing a surgical airway during the COVID-19 pandemic
Botti C, Lusetti F, Castellucci A, Costantini M, Ghidini A (2020) Safe tracheotomy for patients with COVID-19 Am J Otolaryngol 7:102533
Pichi B, Mazzola F, Bonsembiante A, Petruzzi G, Zocchi J, Moretto S, De Virgilio A, Pellini R (2020) CORONA-steps for tracheotomy in COVID-19 patients: a staff-safe method for airway management Oral Oncol 105:104682
Kligerman MP, Vukkadala N, Tsang RK, Sunwoo JB, Holsinger FC, Chan JY, Damrose EJ, Kearney A, Starmer HM (2020) Managing head and neck cancer patients with tracheostomy or laryngectomy during the COVID-19 pandemic Head Neck 42(6):1209
Kowalski LP, Sanabria A, Ridge JA, Ng WT, de Bree R, Rinaldo A, Takes RP, Mäkitie AA, Carvalho AL, Bradford CR, Paleri V (2020) COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice Head Neck 42(6):1259–1267
Vargas M, Servillo G (2020) Improving staff safety during tracheostomy in COVID-19 patients Head Neck 42(6):1278–1279
Xiao H, Zhong Y, Zhang X, Cai F, Varvares MA (2020) How to avoid nosocomial spread during tracheostomy for COVID-19 patients Head Neck 42(6):1280–1281
Miles BA, Schiff B, Ganly I, Ow T, Cohen E, Genden E, Culliney B, Mehrotra B, Savona S, Wong RJ, Haigentz M (2020) Tracheostomy during SARS-CoV-2 pandemic: recommendations from the New York head and neck society Head Neck 42(6):1282–1290
David AP, Russell MD, El-Sayed IH, Russell MS (2020) Tracheostomy guidelines developed at a large academic medical center during the COVID-19 pandemic Head Neck 42(6):1291–1296
Skoog H, Withrow K, Jeyarajan H, Greene B, Batra H, Cox D, Pierce A, Grayson JW, Carroll WR (2020) Tracheotomy in the SARS-CoV-2 pandemic Head Neck 42:1392–1396
Damian B, Panayiotis K, Kevin S, Alistair S, Chetan K, Leandros V (2020) Surgical tracheostomies in Covid-19 patients: important considerations and the “5Ts” of safety Br J Oral Maxillofac Surg 58:585–589
Schultz P, Morvan JB, Fakhry N, Morinière S, Vergez S, Lacroix C, Bartier S, Barry B, Babin E, Couloigner V, Atallah I (2020) French consensus regarding precautions during tracheostomy and post-tracheostomy care in the context of COVID-19 pandemic Eur Ann Otorhinolaryngol Head Neck Dis 137(3):167–169
Foster P, Cheung T, Craft P, Baran K, Kryskow M, Knowles R, Toia A, Galvez C, Bowling A, DiSiena M (2020) Novel approach to reduce transmission of COVID-19 during tracheostomy J Am Coll Surg 230(6):1102–1104
Youn SH, Baek SY, Yoon J, Hong SS, Kim Y (2020) A case report of tracheostomy for a patient with COVID-19: how to minimize medical staff and patient risks J Kor Med Sci 35:28
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Shah, R., Priyadarshini, G. & Parsana, M. “A Systematic Review on Guidelines and Recommendations for Tracheostomy During COVID-19 Pandemic”. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2947–2958 (2022). https://doi.org/10.1007/s12070-021-02517-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02517-9