1. Introduction
Coronavirus disease (COVID-19) is a new infectious disease that is mainly transmitted by respiratory droplets and contact and is generally infectious to human beings [
1]. The impact of the COVID-19 pandemic is the most significant flu pandemic since 1918, which resulted in a huge impact worldwide [
2]. According to the World Health Organization, as of 16 February 2022, the total number of confirmed COVID-19 cases globally is 414,525,183, including 5,832,333 deaths [
3]. As a result, the COVID-19 epidemic becomes the focus of worldwide attention. Since the outbreak of the COVID-19 epidemic, a large number of relevant studies, mainly in the areas of disease characteristics and causative mechanisms [
4,
5,
6,
7,
8], public mental health [
9,
10,
11,
12], socio-economic impact [
13,
14,
15] and social governance [
16,
17,
18,
19], with the medical field dominating, have been conducted by researchers in various fields worldwide. Relatively few studies have been carried out at the spatial level, mainly focusing on the spread pattern of the COVID-19 epidemic between provinces and cities [
20,
21,
22], and the spatial factors that affect the spread of the epidemic. Several studies have mentioned the role of migrant population density [
23,
24] or lived population density [
25,
26,
27] on the spread of COVID-19, in addition to studies that have explored factors such as Within this scope, medical facilities are an important part of the city’s public facilities, and the effective deployment of medical facilities plays an important role in curbing the rapid spread of COVID-19. Therefore, exploring the allocation of urban healthcare facilities is important in responding to major public health emergencies.
The uncertainty and strong contagiousness of COVID-19 not only threatens one’s physical health but also seriously affects one’s psychological health, especially in terms of one’s emotional well-being [
28,
29]. An effective way to stop the spread of the epidemic is to stop human communication and activity, which can be extremely emotionally challenging. In China, COVID-19 was first identified and rapidly broke out in Wuhan, Hubei Province [
8]. To slow and stop the spread of the virus, Wuhan declared a city lockdown on 23 January 2020, suspending public transport in the city and imposing transport restrictions on individuals [
30]. This measure has been described as the most severe epidemic prevention measure ever taken in human history for a major city with a population of 10 million, and the people of Wuhan faced prolonged panic and confusion as a result [
31,
32,
33]. Under this circumstance, a large number of studies on human emotions during the epidemic have emerged, but most of the existing studies have focused on specific groups, such as health care workers, infected patients, or susceptible people [
34,
35,
36], mainly in the areas of mental health [
37,
38,
39] and public reactions [
40,
41], and only a few studies have focused on the spatio-temporal characteristics of mood fluctuations of home-isolated citizens [
42].
At the same time, public mood and the allocation of healthcare facilities have clear correlation [
22]. Hospitals, as facilities for daily life services, are conducive to evoking positive public sentiment [
43]. However, when faced with a major public health emergency, hospitals are high-risk areas with large numbers of pathogen carriers that can facilitate the spread of the virus amongst health care workers, patients and hospital visitors, thereby leading to negative emotions amongst the surrounding population [
2]. Therefore, this study focused on public sentiment and medical facility during the COVID-19 outbreak to explore the concordance between them.
The spread of COVID-19 has led to increased difficulty in on-site social surveys and small, time-consuming research samples [
44]. Social media data provide geolocation data with temporal information [
45], which creates a new solution for relevant research. With its real-time nature and high interactivity, social media has become an important way for citizens in terms of self-perception and information exchange in the process of controlling the spread of the COVID-19 [
46,
47,
48,
49]. These spatiotemporal data have great potential to be used for machine learning and text mining to analyse and understand human behaviour, public reactions, potential courses of action and public opinion better [
50,
51].
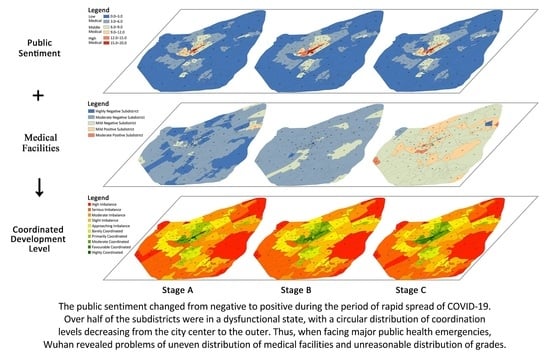
This study analyses public sentiment at different stages of COVID-19 through social media data; dynamically evaluates the allocation of urban medical facilities during the COVID-19 epidemic at a finer spatial scale; and uses a coordination degree model to determine the level of coordination between them, thereby providing a basis and suggestions for future urban responses to severe public health emergencies and optimising the spatial allocation of urban healthcare resources. The respondents of this study are all discussions about COVID-19 on Weibo by Wuhan residents during the rapid spread of COVID-19. The methods of this paper consist of four steps: (1) by using keywords and SVM classifier to filter the microblog text data related to COVID-19 and classify the epidemic into different phases according to public attention; (2) by using an extended sentiment dictionary to determine the sentiment polarity of Weibo text; (3) by analysing the spatial distribution characteristics of public sentiment and medical facilities at different levels during various stages of the epidemic; and by (4) measuring the ratio of sentiment values and medical facility coverage in each subdistrict of Wuhan at different stages of the epidemic and determining the coordination level based on the coordination degree model. The paper is structured as follows: the first part is an introduction and research background. The second part discusses the basic social background of the study area, data sources and pre-processing process. The third section explains the screening method and sentiment polarity determination method of Weibo text, as well as the kernel density method and the coordination model used subsequently. The three latter sections present the results, discussion and conclusions.
4. Discussion
The COVID-19 outbreak prompted researchers to begin rethinking urban space. From historical experience, urban planning is an important way for local governments to safeguard urban public health and reduce infectious diseases. For example, the Black Death epidemic led to the strengthening of basic sanitation facilities in European countries. The cholera epidemic forced the UK government to set a number of health standards and provide public health services [
22]. Therefore, creating healthier urban spaces in the post-epidemic era is particularly important.
The key to a healthy city is urban healthcare facilities, which are mostly evaluated in existing studies focusing on spatial accessibility, equity [
73,
74,
75] and supply-demand balance of healthcare facilities [
76,
77,
78]. The outbreak of COVID-19 has reduced the geographic accessibility of medical facilities [
79,
80,
81,
82], and the reduction is greater in the urban periphery than in the central city [
83]. Different from them, this study focuses on public emotions and evaluates the spatial configuration of medical facilities. it was found that the allocation of medical facilities in Wuhan showed a gradually decreasing distribution pattern from the centre to the periphery, which is similar to other Chinese cities, such as Zhengzhou, Shanghai, and Shenzhen [
73,
84,
85], implying that the government needs to take seriously the lag in healthcare service facilities during urban expansion. On the other hand, public sentiment surveys are highly valuable for improving health systems [
86], which is mainly used to evaluate the quality of services provided by the health care system [
87,
88]. Studies at the spatial level have focused on the urban perspective [
22,
89], while there is a lack of evaluation of the configuration of health care facilities at a finer scale, this study examines the subdistrict scale to fill this gap.
Nevertheless, this study has limitations, and future refinements are needed in the following areas.
- (1)
Weibo users are not representative of all Wuhan residents during the COVID-19 pandemic. According to the 2020 Weibo User Development Report [
58], most Weibo users are between the ages of 20 and 30, accounting for 48% of the population. In contrast, according to the Wuhan Statistical Yearbook 2021 [
90], the proportion of 20- to 30-year-olds in the total population of Wuhan is 14%. The way the information is shared may vary by gender and age. Since few of the social media users are elderly or children, social media data cannot fully reflect public sentiment. Further research considering the diversity of data sources is needed to obtain more extensive and accurate conclusions. In addition, given that there is evidence to suggest that cultural background and household situation can influence perceptions and experiences with the health system [
91,
92], we will aim to include such questions in similar future surveys.
- (2)
Due to the diverse forms of expression in Chinese, the use of emotion dictionaries to determine the emotional polarity of text cannot fully identify the emotion expressed by the user, and future research could use methods, such as machine learning, to capture emotion accurately.
- (3)
Many factors can affect the evaluation of the configuration of medical facilities. Besides considering public sentiment, there are some other variables that cannot be ignored, such as urban population distribution, spatial accessibility, urban spatial development level, actual medical behaviour of residents, spatial spread of COVID-19 epidemics, etc. In the future research, we will further improve the methods and ideas, explore the influence of other factors and the relationship between them, and provide decision reference for the fine layout and function enhancement of perfect urban medical facilities.
5. Conclusions
This study analysed the evolution of public sentiment during the rapid spread of COVID-19 in Wuhan using social media data processed by an SVM classifier; explored the relationship between public sentiment and medical facilities at the subdistrict scale; and conducted a detailed dynamic demand evaluation of COVID-19 medical facilities in Wuhan based on public sentiment.
The results show the following: Firstly, public sentiment has an overall positive trend as the phase of the COVID-19 epidemic changes. Public attention to the epidemic ranged from low to high, with a rapid outbreak after the lockdown of Wuhan and a stabilisation at a later stage. This indicates that public sentiment becomes increasingly positive as the epidemic is effectively controlled and as urban medical resources are replenished. Secondly, during the latent and stable stages of the COVID-19 epidemic, residents of subdistricts with a large coverage ratio of medical facilities had more positive sentiments, whilst an opposite pattern is observed during the outbreak. Adequate medical facility allocation was found to elicit positive public sentiment, but dense medical facilities acting as a source of viral infection at specific times can elicit negative public sentiment, so a reasonable grade allocation with moderate density is key to medical facility layout. Thirdly, in all three phases, more than 50% of the subdistricts are in a state of dissonance, and Stage B is more coordinated than Stages A and C. The distribution of coordination levels is consistent across the three phases, thereby showing a circular decreasing pattern from the city centre to the periphery, with subdistricts of high coordination level distributed in clusters in the city centre with a high level of medical facilities and a dense distribution; subdistricts with a low coordination level are located near the third ring road and in less inhabited scenic areas with weak medical resources. It shows that in the face of severe public health emergencies, Wuhan has the problems of uneven distribution of numbers, unreasonable distribution of levels, and insufficient coverage of tertiary hospitals, and the configuration of medical facilities in the periphery of the city is weaker than that in the central area, which provides a basis for future research on the optimization of the spatial layout of medical facilities in Wuhan.
In the future, urban planners should pay more attention to areas with less coverage of tertiary hospitals, such as Wuchang District, and increase the number of medical facilities, especially hospitals, in these areas. For areas with relatively dense medical facilities, a reasonable layout and rational allocation of hospitals is needed to avoid redundancy of resources. Government departments should establish emergency response plans for major public health emergencies, such as setting up temporary hospitals in areas where medical resources are scarce and setting up designated hospitals in their vicinity to safeguard the public’s demand for medical treatment and alleviate negative public sentiment. In addition, community medical facilities play a vital role in the control of the COVID-19 epidemic [
93], and should respond to the advocacy of “Building a 15 min Community Life Circle” [
94], strengthen the construction of primary healthcare system, improve the level of medical services in community hospitals, and convenience residents by enabling access to medical services closer to home.
The representative characteristics of Wuhan, a metropolis with developed transportation, dense population, and the first city in China to detect COVID-19 virus and its rapid spread, make the research results in Wuhan universal and forward-looking, and may provide lessons for other cities facing major public health emergencies. It is of great value to those involved in urban planning and design and may help them to quickly determine the evolution of public sentiment under a health emergency and whether medical facilities in various areas of the city meet public demand, so that they can act in advance to fill the shortcomings of the urban health system and optimize the spatial layout of urban medical facilities. Additionally, we focus on urban space at the subdistrict scale, which supports the development direction of more humane and refined urban planning in the future.