Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6080
Peer-review started: May 28, 2020
First decision: September 23, 2020
Revised: October 6, 2020
Accepted: October 27, 2020
Article in press: October 27, 2020
Published online: December 6, 2020
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new virus responsible for the outbreak of respiratory illness known as coronavirus disease 2019 (CoVID-19). Mycoplasma is an uncommon co-infected pathogen with SARS-CoV-2 and has not yet been reported. Computed tomography (CT), used as an accessory examination, may play a more significant role in this co-infection.
A 49-year-old female presented with a cough, expectoration and chest congestion followed by elevated C-reactive protein and erythrocyte sedimentation rate. CT images showed ground-glass opacities in bilateral lower lobes and a patchy and striate shadow in the right upper lobe. Immunoglobulin M antibody of Mycoplasma pneumoniae was positive and real-time fluorescence polymerase chain reaction of sputum was positive for SARS-CoV-2 nucleic acid. The diagnosis of CoVID-19 was made based on laboratory results, chest CT images, clinical manifestations and epidemiologic characteristics. She was treated with combination therapy for 17 d and showed a marked reCoVery.
Co-infection with SARS-CoV-2 and Mycoplasma in CoVID-19 patients appears to be uncommon. CT is an acceptable method for the primary diagnosis and treatment should be initiated as soon as possible. Combination therapy with antiviral, anti-inflammatory, traditional Chinese herbal medicine and interferon inhalation may be a reference for further progress in treating this co-infection.
Core Tip: In this study, we evaluated the disease evolution of a 49-year-old lady co-infected with severe acute respiratory syndrome coronavirus 2 and Mycoplasma. This co-infection is rare and her computed tomography (CT) images showed both typical manifestations of coronavirus disease 2019 and untypical findings which suggested Mycoplasma infection. Although the disease developed rapidly, with early intervention and treatment, we successfully prevented her from becoming worse. Clinical improvement on CT images suggested that our combination therapy of antiviral, anti-inflammatory, traditional Chinese herbal medicine and interferon inhalation may be an effective early treatment and a reference for further progress in treating this co-infection.
- Citation: Gao ZA, Gao LB, Chen XJ, Xu Y. Fourty-nine years old woman co-infected with SARS-CoV-2 and Mycoplasma: A case report. World J Clin Cases 2020; 8(23): 6080-6085
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6080.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6080
Coronavirus disease 2019 (CoVID-19) is a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which has already infected over 70000 and killed more than 2000, especially in Wuhan, China. A study of 8274 samples showed that 5.8% of CoVID-19 infected and 18.4% of non-CoVID-19-infected patients had other infections[1]. However, co-infection with SARS-CoV-2 and Mycoplasma has not been reported previously. We report the case of a 49-year-old female co-infected with SARS-CoV-2 and Mycoplasma.
A 49-year-old woman came to the Outpatient Service of our hospital complaining of a cough, chest discomfort and fatigue on January 20, 2020.
The patient's symptoms started 5 d ago with a cough, expectoration and chest congestion.
She mentioned a travel history to Wuhan one week ago, the center of this CoVID-19 outbreak.
On admission, symptoms of cough, expectoration of white sputum, chest congestion and fatigue were observed, but her body temperature was normal 37.0°C (98.6°F). Coarse breath sounds in both lungs with wet rales distributed at the base of both lungs were heard on auscultation.
Laboratory studies showed a normal leukocyte count (white blood cell count, 5.58 × 109/L) and normal lymphocyte count (lymphocyte count, 1.47 × 109/L). The leukocyte differential count indicated 64.9% neutrophils, 26.3% lymphocytes, and 5.9% monocytes. There were elevated blood levels of C-reactive protein (12.50 mg/L) and erythrocyte sedimentation rate (37 mm/h). Albumin (32.1 g/L) and serum calcium (3.26 mmoL/L) were lower. Immunoglobulin M (IgM) antibody of Mycoplasma pneumoniae was positive (Table 1).
| Index | Result | Reference range | |
| Blood leukocyte count (109/L) | 4.29 | - | 3.5-9.5 |
| Lymphocyte count (109/L) | 0.94 | ↓ | 1.1-3.2 |
| Platelet count (109/L) | 214 | - | 125-350 |
| Hemoglobin level (g/L) | 138 | - | 115-150 |
| C-reactive protein level (mg/L) | 3.50 | - | 0-10 |
| Procalcitonin level (ng) | 0.031 | - | 0.000-0.500 |
| Lactate dehydrogenase (U/L) | 252 | ↑ | 120-250 |
| Aspartate aminotransferase (U/L) | 25 | - | 13-35 |
| Alanine aminotransferase (U/L) | 17 | - | 7-40 |
| Total bilirubin (μmoL/L) | 13.9 | - | 0-23 |
| Creatinine kinase (U/L) | 52 | - | 0-145 |
| Creatinine (μmoL/L) | 49.2 | - | 41-73 |
| D-dimer (μg/L) | 290 | - | 0-550 |
| Sodium (mmoL/L) | 138.6 | - | 137-147 |
| Potassium (mmoL/L) | 3.26 | ↓ | 3.5-5.3 |
| Chloride (mmoL/L) | 102.8 | - | 99-110 |
| Total calcium (mmoL/L) | 1.77 | ↓ | 2.11-2.52 |
| Blood oxygen saturation (%) | 95 | - | 95-98 |
| Erythrocyte sedimentation rate (mm/h) | 37 | ↑ | 0-20 |
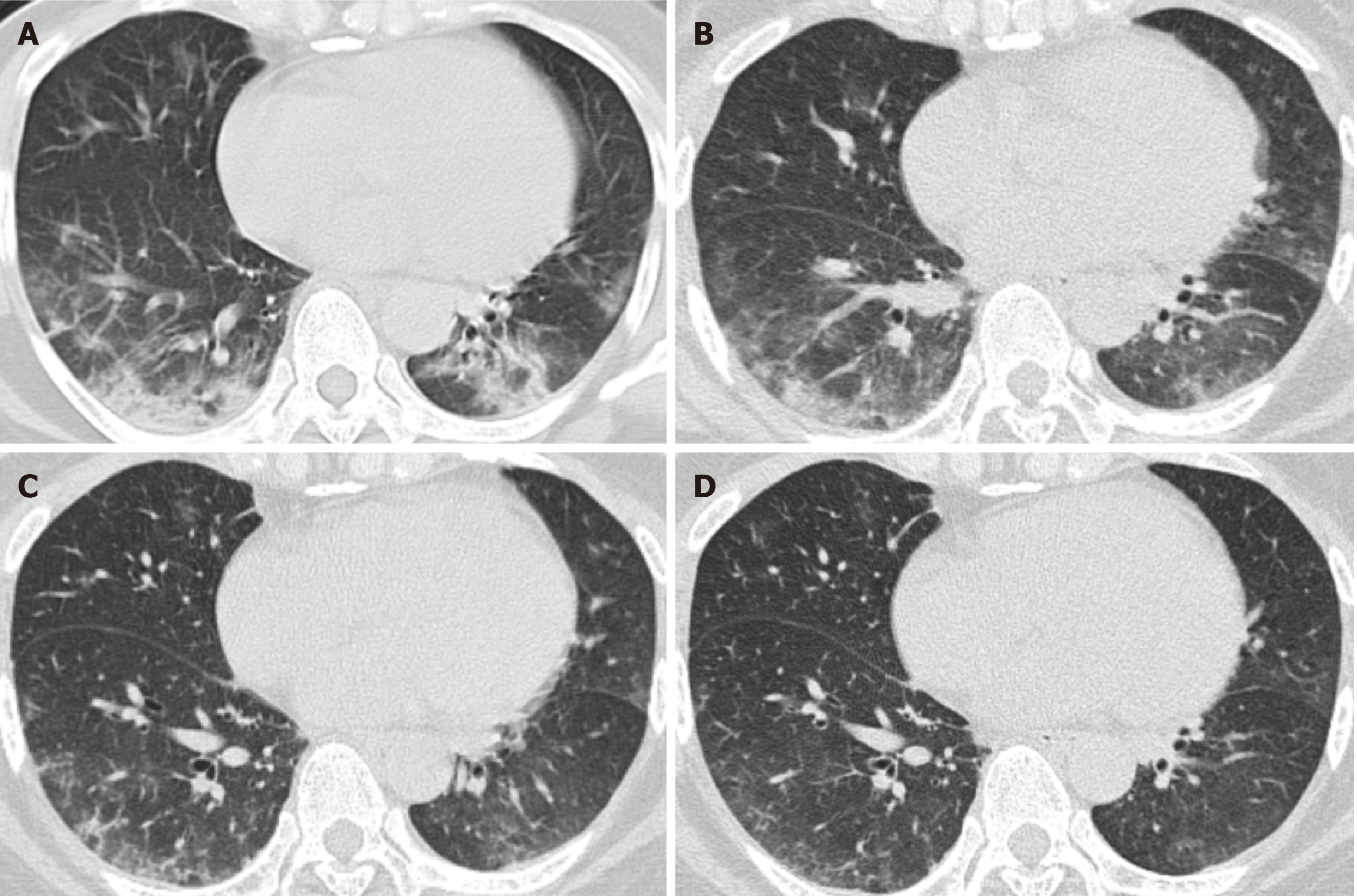
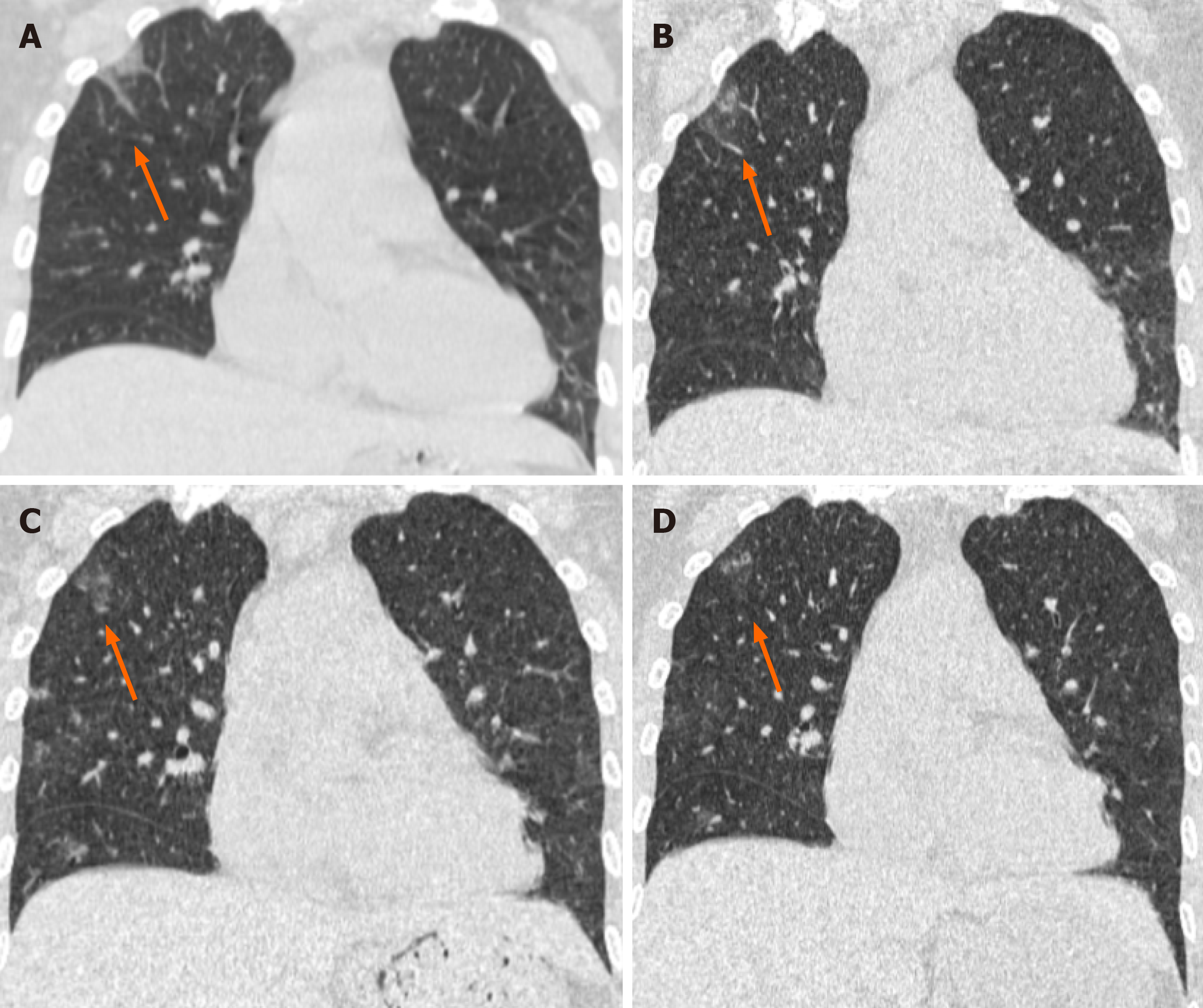
Unenhanced chest computed tomography (CT) showed ground-glass opacities in bilateral lower lobes and a patchy and striate shadow in the right upper lobe. According to these findings and due to her travel history to Wuhan, we speculated that she had Mycoplasma infection and suspected SARS-CoV-2 infection; therefore, we sent a throat swab for analysis and the results were expected to take several days. Considering her CT images and the rapid development of CoVID-19, we treated the patient with anti-inflammatory and empirical antiviral drugs in the first three days. CT images showed progressive manifestations.
Three days later, real-time fluorescence polymerase chain reaction (RT-PCR) of sputum was positive for SARS-CoV-2 nucleic acid and her diagnosis of CoVID-19 was finally made based on laboratory results, chest CT images, clinical manifestations and epidemiologic characteristics. We were glad that we performed early intervention with antiviral therapy based on the previous CT manifestations.
CT showed multiple patchy ground-glass opacities and consolidated opacities in bilateral lower lobes (Figure 1) and a patchy and striate shadow of slightly high density in the upper right lung (Figure 2). This asymmetrical lesion in the upper right lobe was quite rare in the cases reported so far.
CoVID-19 and Mycoplasma infection.
According to Chinese newest treatment guidelines for SARS-CoV-2, the patient was treated with antiviral drugs (Aluvia, Peramivir, Interferon-α2b), anti-inflammatory drugs (Cefonicid Sodium, Azithromycin, Moxifloxacin) and traditional Chinese herbal medicine (Lianhuaqingwen), combined with supportive care and interferon inhalation from January 25, 2020 and she was discharged on February 10, 2020.
On the 7th day, her cough, expectoration, chest congestion and debilitation started to improve. Laboratory tests of SARS-CoV-2 nucleic acid, lymphocyte count, erythrocyte sedimentation rate, potassium, total calcium, lactate dehydrogenase, blood oxygen saturation and IgM antibody of Mycoplasma pneumoniae all showed that the patient had improved. A marked reCoVery was noted in this patient at the 2 wk follow-up.
The outbreak of CoVID-19 caused by SARS-CoV-2 has resulted in significant harm to human health globally, and has been declared a public health emergency of international concern by the WHO[2].
CoVID-19 has spread in 43 countries, including South Korea, Japan, Italy, and the United States. Person-to-person transmission in hospital and family settings has been identified and more than 2600 lives have been lost. From up-to-date data, it can seen that fever and cough are the most common symptoms, and both diarrhea and vomiting are rare. Most patients have lymphopenia and elevated levels of C-reactive protein on admission[3]. Among 2745 CoVID-19 patients, 104 were positive for multiple respiratory pathogens and 6/104 had co-infection with coronavirus (3/104), influenza A virus (2/104), rhinovirus (2/104), and influenza A H3N2 (1/104)[1]. Co-infection with SARS-CoV-2 and Mycoplasma is unusual and has not been reported previously. Treatment protocols and prognosis are new with few references.
Imaging studies have shown that ground-glass opacity and bilateral patchy shadowing are the most common features on chest CT[3-5]. In our patient, progressive changes in typical CT manifestations were seen in bilateral lower lobes which were thought to be caused by CoVID-19, but an untypical isolated shadow in the upper right lung was also seen. This was thought to be caused by Mycoplasma infection.
In conclusion, co-infection with SARS-CoV-2 and Mycoplasma should not be ignored in clinical diagnosis and treatment, especially in the early course as CoVID-19 is a rapidly developing disease. CT manifestations may be a better and quicker route to the diagnosis of CoVID-19 than nucleic acid testing using RT-PCR, and can result in timely treatment. Clinical improvement in CT images in our patient suggested that our novel combination therapy may be a reference for further progress in the treatment of this co-infection. As these pathogens are very infectious, doctors and nurses, particularly those on the first line, require personal protective equipment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hossain MG, Phan T S-Editor: Fan JR L-Editor: Webster JR P-Editor: Xing YX
| 1. | Analysis of 8274 cases of novel coronavirus nucleic acid detection and co-infection in Wuhan. Zhonghua Jianyan Yixue Zazhi. 2020;43:341-345. [DOI] [Cited in This Article: ] |
| 2. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18987] [Cited by in F6Publishing: 16536] [Article Influence: 4134.0] [Reference Citation Analysis (0)] |
| 3. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for CoVid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19202] [Cited by in F6Publishing: 18004] [Article Influence: 4501.0] [Reference Citation Analysis (5)] |
| 4. | Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295:202-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1827] [Cited by in F6Publishing: 1641] [Article Influence: 410.3] [Reference Citation Analysis (0)] |
| 5. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32663] [Cited by in F6Publishing: 28495] [Article Influence: 7123.8] [Reference Citation Analysis (3)] |