- 1Eye Center, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 2Zhejiang Provincial Key Lab of Ophthalmology, Hangzhou, China
- 3Department of Orthopedics, First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 4Key Laboratory of Cancer Prevention and Intervention, Ministry of Education, Cancer Institute, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 5Department of Cardiology, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 6Department of Medical Oncology, Key Laboratory of Cancer Prevention and Intervention, Ministry of Education, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
Background: The Coronavirus disease 2019 (COVID-19) has presented a major challenge to the health, economic, and social sectors of the entire world. This study aimed to investigate the mental health and academic performance of medical postgraduates during the COVID-19 pandemic in China.
Methods: A cross-sectional online survey was conducted from March 20 to April 20, 2022 at the Zhejiang University School of Medicine in China. The questionnaire consisted of three parts: general information, mental health and academic performance. Mental health outcomes were assessed according to the Generalized Anxiety Scale (GAD-7) and the Patient Health Questionnaire-9 Scale (PHQ-9).
Results: A total of 153 valid questionnaires were obtained. Of the medical postgraduates in this study, (1) 41.8% had no anxiety symptoms. In addition, 51.0% had mild anxiety symptoms during the COVID-19 pandemic. None of the participants had a severe anxiety or depression disorder; (2) Females experienced significantly more symptoms in mental health measure scores than the males (P < 0.01); (3) 78.4% believed that the COVID-19 pandemic had varying degrees of impact on their academics. Doctoral postgraduates showed greater academic stress, and they were more worried about not meeting graduation standards than the master's postgraduates (P < 0.05). There were no significant differences between the surgical postgraduates and internal postgraduates in either mental health or academic performance.
Conclusions: Our study found that the COVID-19 pandemic has had a mild impact on the mental health and academic performance of medical postgraduates in China. Females experienced significantly more symptoms on mental health measure scores than the males. Doctoral postgraduates showed greater academic stress than the master's postgraduates. There is uncertainty regarding how long this COVID-19 situation will persist and increasing recognition that there may be periods of recurrence in the future. We need more active curricular innovation and transformation to maintain and improve medical postgraduates' mental health and academic performance.
Introduction
Since the World Health Organization (WHO) declared a global emergency on January 30, 2020 concerning the novel coronavirus disease-19 (COVID-19) outbreak (1, 2), COVID-19 has presented a huge challenge to the health, economic and social sectors of the entire world. The WHO reported 514 million confirmed cases of COVID-19 and 6.2 million confirmed deaths worldwide as of May 4, 2022 (3). Due to COVID-19, mental health illnesses including anxiety, depression, stress, and sleep disorder have become prevalent problems across the world. Various studies demonstrated that during the COVID-19 pandemic, mental health problems such as fear, anxiety and depression were common among the general public, patients, medical staff, children, and older adults (4–8). Previous research concluded that throughout 2020, the COVID-19 pandemic led to a 27.6% increase in cases of major depressive disorders and 25.6% increase in cases of anxiety disorders globally (9). Among general population in China, the prevalence of depressive symptoms, anxiety, and stress ranging from moderate to severe were, respectively, 16.5, 28.8, and 8.1% (10).
Considered as a top-down management system, the Chinese government has effectively adopted a dynamic clearance policy to control the COVID-19 pandemic over the past 2 years (11). Specifically, the local government is carrying out community, block, district, or regional lockdowns as needed whenever COVID-19 cases are reported. Therefore, schools and public places are closed in lockdown areas, and students must study online at home. For postgraduate medical students, many courses have been transferred from classroom learning to online learning due to the changes in learning and living environments. Consequently, medical students are unable to communicate effectively with teachers, and there is a lack of internship opportunities for clinical learning in the hospital (12). These unprecedented changes and unique challenges have affected medical students' mental health and academic performance. There are a growing number of studies on how college and medical students have adapted to the COVID-19 pandemic (13–16). Mental health disorders among Greek medical students have been reported in connection with the COVID-19 pandemic (17). Similar findings have also been reported in China. Specifically, compared with non-medical students, medical students had fewer mental health symptoms in the early stages of the COVID-19 pandemic since they are more knowledgeable about COVID-19 (18).
Medical students in China have experienced various restrictions and challenges due to the prevention and control of the pandemic during the past 2 years. Compared with the beginning of the pandemic, medical students have become more and more adaptable to these various restrictions and challenges, resulting in our study of the impacts on their mental health and academic performance. Undergraduate medical students in China mainly study in the classroom. Meanwhile, postgraduate medical students need to spend a large amount of time in the hospital for clinical learning and research under their supervisors' hands-on guidance. Therefore, the COVID-19 pandemic has had a greater impact on postgraduate medical students' academic studies and clinical learning in the hospital. Therefore, the aim of the present study is to evaluate the impact of the 2 year COVID-19 pandemic on the postgraduate medical students' mental health (e.g., anxiety, depression) and academic performance in China. The present study was a web-based, cross-sectional study. The questionnaire consisted of three parts: general information, mental health and academic performance.
Methods
Setting and sample
A cross-sectional survey using structured questionnaires was conducted among medical postgraduate students at the Zhejiang University School of Medicine in Hangzhou, China. The data were collected from March 20 to April 20, 2022. During this period, students in China were still affected by the COVID-19 pandemic. The inclusion criteria were as follows: students (1) had normal mental state in the school; (2) who agreed to participate in the study after being fully informed of details of the study. Exclusion criteria were any physical or neurological disease, substance use, psychotic disorders, and personality disorders. We adopted the method of stratified random sampling, and divided the postgraduates in the school of Zhejiang University School of Medicine into a doctoral class of surgery, a master's class of surgery, a doctoral class of internal medicine and a master's class of internal medicine. Forty to fifty postgraduate students were randomly selected from each class, and 177 medical postgraduate students were selected as research objects. They were invited to voluntarily participate in the survey through the network platform (http://www.wjx.cn, which is one of the most popular electronic survey platforms in China). We tested its internal consistency in a pilot study of 50 students. The questionnaire had a high level of internal consistency among our study population, with a Cronbach's alpha 0.88. An online survey questionnaire was distributed randomly to students via WeChat. Participants were asked to read the instructions about the purpose and methods to fill out the questionnaire carefully. Participants were also informed that the survey was anonymous. A total of 177 questionnaires were sent out. Twenty-four of the retrieved questionnaires were invalid and were thus excluded from the study, and 153 were valid. The effective survey questionnaire retrieval rate was thus 86.44%. Ethical approval was obtained from the ethics committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University in China. All participants provided written informed consent prior to participating in the study without identifiable data.
General information
The first part of the questionnaire asked about the basic demographic information of the participants (such as gender, home location, grade, academic major, marital status and health status).
Mental health
The second part of the questionnaire addressed the participants' general anxiety and depression disorders during the COVID-19 pandemic. The questionnaire was adapted from the Generalized Anxiety Scale (GAD-7) and the Patient Health Questionnaire-9 Scale (PHQ-9) (19–21). The revised GAD-7 questionnaire had a total of 6 items. Example item is “I feel nervous or anxious during COVID-19 pandemic.” Items are scored on a four-point Likert scale ranging from 0 (never) to 3 (always), with scores of 0, 1, 2 and 3 according to “none at all,” “a few days,” “more than half of the days” and “almost every day.” According to the final score of the questionnaire, the research subjects were divided into the normal group (0–3 points) and the anxiety symptom group (3–18 points). The revised PHQ-9 questionnaire had a total of 4 items. The total score of the questionnaire is 0–12 points, 0–3 points were divided into normal group, and those with ≥3 points were judged to have depressive symptoms. The higher the score, the more severe the social anxiety or depression. In previous studies on Chinese general and adolescent populations, the GAD-7 and PHQ-9 scores showed good psychometric properties (22–24).
Academic performance
The third part of the questionnaire was the investigation of the personal academic performance of the clinical medical postgraduates. They were asked about the overall impact on academics, worrying that they would not meet graduation standards, the percentage of offline courses converted to online courses, the percentage of practice opportunities reduced and the frequency of counseling and academic communication with graduate tutors.
Statistical analysis
The data from the retrieved electronic survey questionnaires were gathered using Questionnaire Star. Categorical variables were described as counts (n) and percentages (%). The questionnaire scores were expressed as mean ± SD, and between-group statistical comparisons were made using an independent sample t-test or the Mann-Whitney U test, depending on normal distribution (25, 26). Two-sided P-values were considered significant at p < 0.05. All data were analyzed using SPSS version 22.0 software.
Results
Demographic Characteristics
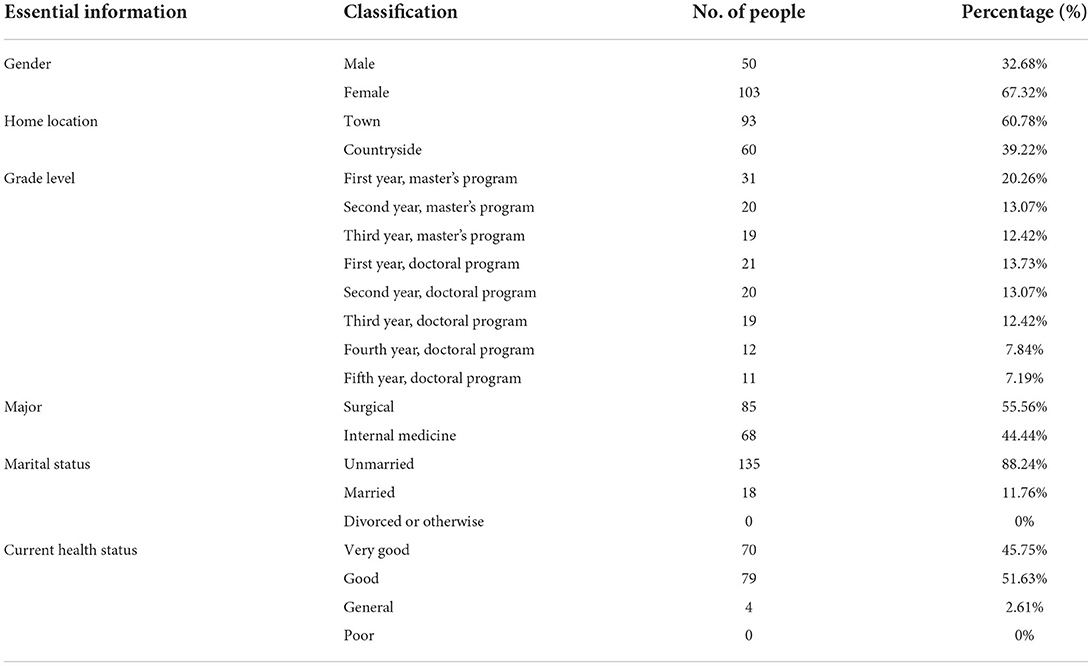
A total of 153 medical postgraduates completed the survey. Table 1 shows the distribution of the study participants. Most (67.32%) were female. Those who completed the survey were 45.76% master's students and 54.24% doctoral students. 55.56% of the postgraduates who participated in this questionnaire were surgical students, and 44.44% were internal medical students. Most were unmarried (88.24%). The current health status of the postgraduates was basically good, and the proportion of students with a poor health status was 0%, based on self-assessment.
The impact of the COVID-19 pandemic on the mental health of medical postgraduates
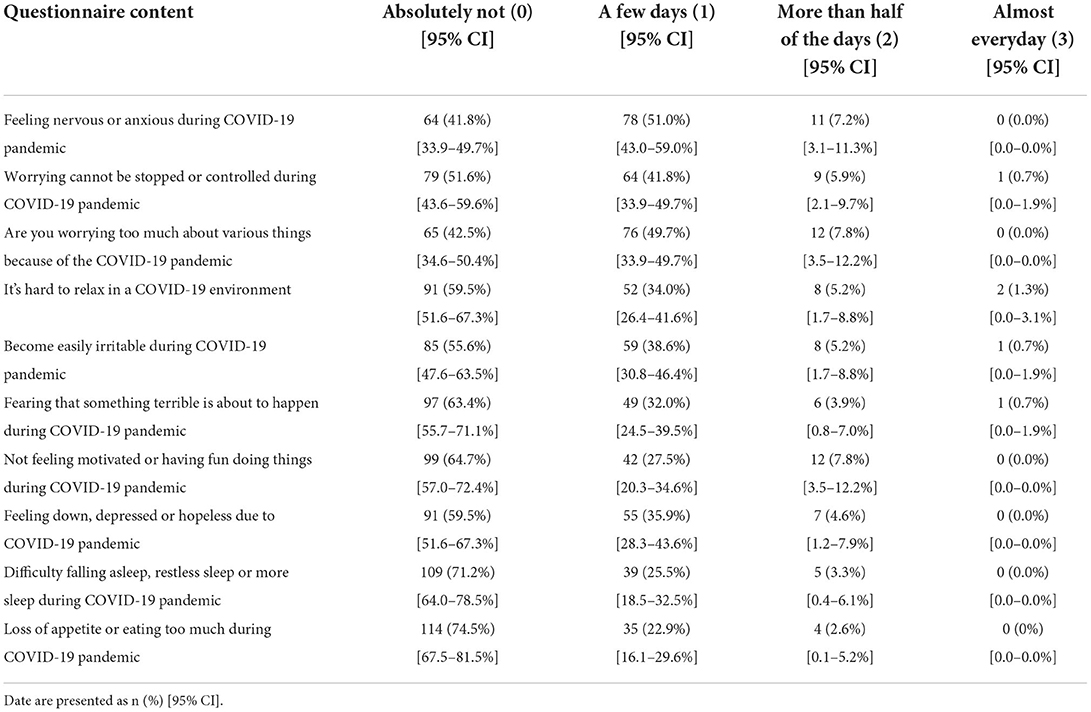
Most of the medical postgraduates who participated in this study had no or mild mental health symptoms during the COVID-19 pandemic (Table 2). Most had low scores for anxiety or depression. Only two people (1.3%) felt that it was hard to relax in the COVID-19 environment almost every day. One person (0.7%) had a severe symptom of anxiety. In addition, none of the participants had a severe depression disorder.
The impact of the COVID-19 pandemic on the academic performance of medical postgraduates
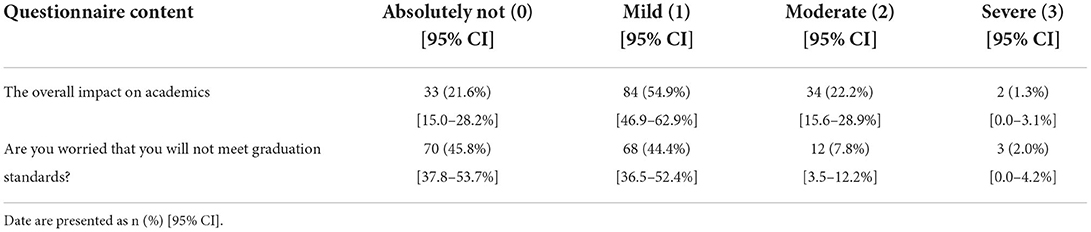
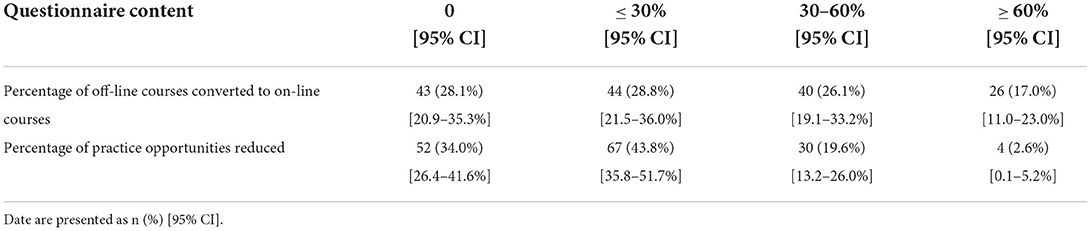
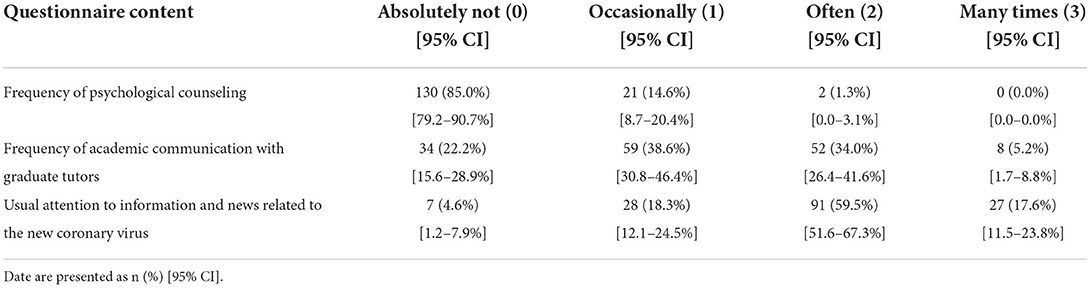
Of the medical postgraduates who participated in this study, 54.9% felt that the COVID-19 pandemic had a mild impact on their academic studies. 22.2% felt that the COVID-19 pandemic had a moderate impact on their academics. Two people (1.3%) believed that the COVID-19 pandemic had a severe impact on their academics. And 83 (54.3%) had varying degrees of concern that they would not meet graduation standards due to the COVID-19 pandemic (Table 3). Furthermore, after investigating the changes in postgraduate courses during the COVID-19 pandemic, we found that the proportion of offline courses that changed to online courses increased, resulting in a reduction in practical operations and less interaction between teachers and students (Table 4). This may explain postgraduates' concerns about their academic performance. Most of the postgraduates (85.0%) were not seeking psychological counseling during this time (Table 5). However, most had an increased frequency of academic communication with graduate tutors. In addition, most of them paid usual attention to information and news related to COVID-19 (Table 5).
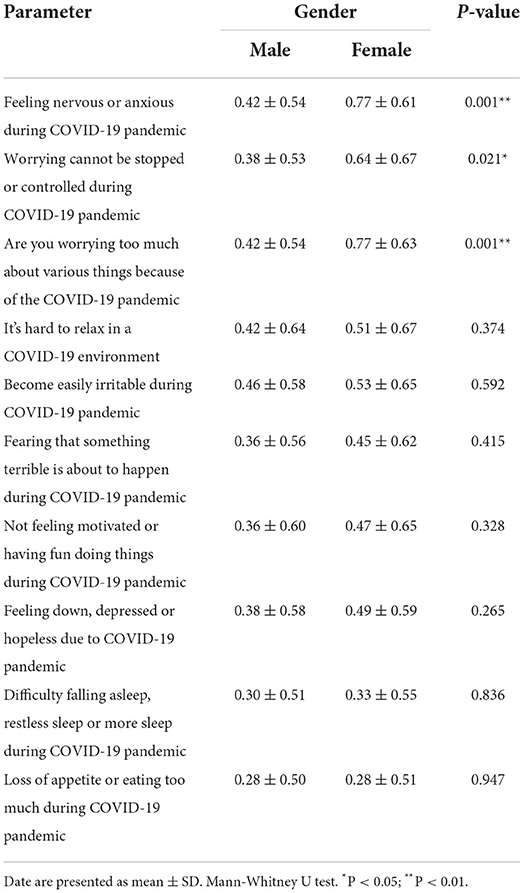
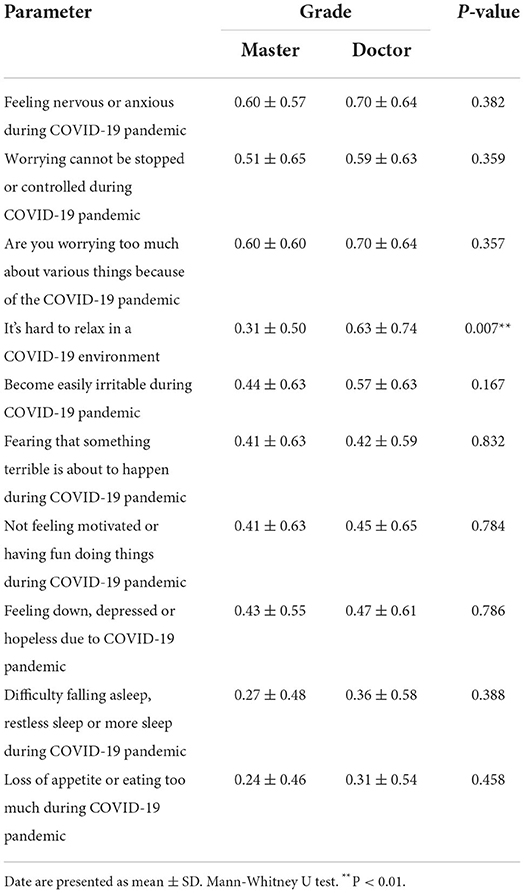
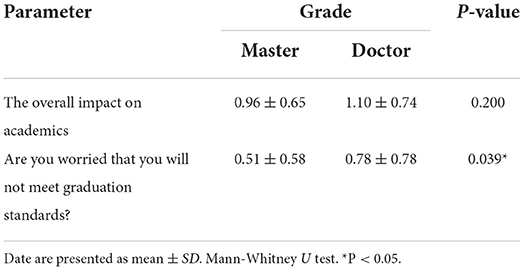
Mental health and academic performance among medical postgraduates with different genders, grades and academic majors
The comparison between genders revealed that females were experiencing significantly more symptoms in mental health measure scores (P < 0.05) (Table 6). The females felt more nervous or anxious during the COVID-19 pandemic than the males (mean 0.77 ± 0.61 vs. 0.42 ± 0.54, P < 0.01). The research showed that the female postgraduates were more likely to worry too much about various things because of the COVID-19 pandemic than the males (P < 0.01). In addition, female postgraduates more commonly felt that worrying could not be stopped or controlled during the COVID-19 pandemic (mean 0.64 ± 0.67 vs. 0.38 ± 0.53, P < 0.05). There were no significant differences in depression symptoms between the males and females (Table 6). In addition, the data showed that there were no significant differences in academic performance between males and females (Supplementary Table 1). Similar results regarding anxiety and depression symptoms were found between the master's class and doctoral class (Table 7). The doctoral students found it harder to relax in a COVID-19 environment (mean 0.63 ± 0.74 vs. 0.31 ± 0.50, P < 0.01). What's more, the doctoral postgraduates were more worried that they would not meet graduation standards (mean 0.78 ± 0.78 vs. 0.51 ± 0.58, P < 0.05) (Table 8). Among the medical postgraduates, there were no significant differences between the surgical students and internal students in either mental health (Supplementary Table 2) or academic performances (Supplementary Table 3).
Multivariable logistic regression of factors influencing mental health and academic studies of medical postgraduates
In the Multivariable logistic regression analysis (Table 9), compared with male postgraduates, the females were experiencing significantly more symptoms in mental health measure scores during the COVID-19 pandemic (OR = 3.256, 95% CI: 1.596–6.642; OR = 2.510, 95% CI: 1.223–5.150; OR = 3.011, 95% CI: 1.481–6.123). The doctoral students (OR = 2.628, 95% CI: 1.303–5.301) found it harder to relax in a COVID-19 environment. What's more, the doctoral postgraduates were more worried that they would not meet graduation standards (OR = 2.019, 95% CI: 1.048–3.889) than the master's class.
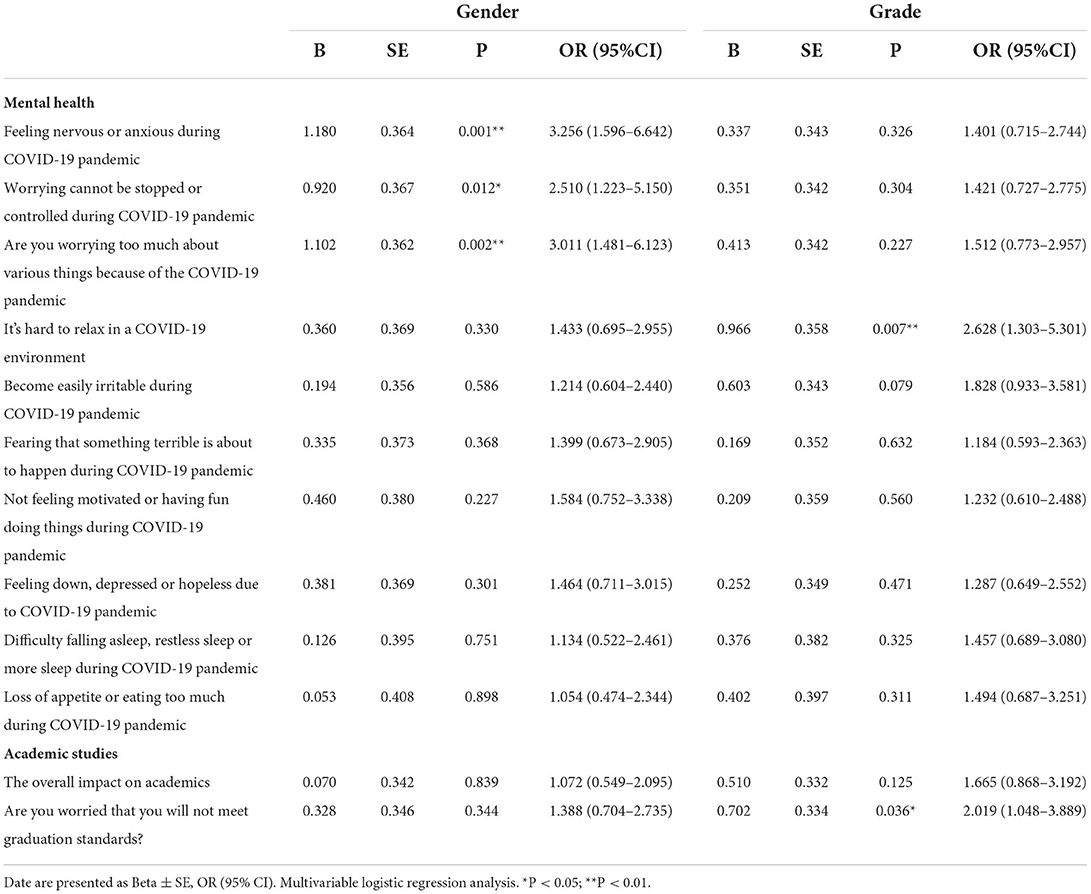
Table 9. Multivariable logistic regression of factors influencing mental health and academic studies.
Discussion
This study used a web-based survey to investigate the mental health and academic performance of medical postgraduates during the COVID-19 pandemic in China. Our major findings are summarized below. First, most of the medical postgraduates had mild anxiety or depression symptoms during the COVID-19 pandemic. Females experienced significantly more symptoms in mental health measure scores than males did. None had a severe depression disorder. Second, 78.43% of participants felt that the COVID-19 pandemic had varying degrees of impact on academics. Moreover, the doctoral postgraduates showed greater academic stress, and they were more worried about not meeting graduation standards than the master's postgraduates.
The outbreak of COVID-19 in the world has had direct and indirect impacts on all areas of society, and the COVID-19 pandemic has lasted for 2 years. Various studies have demonstrated that during the COVID-19 pandemic, mental health problems such as fear, anxiety and depression were common among the general public. A cross-sectional multi-country comparison study demonstrated that substantial variations exist in anxiety and depression symptoms across countries during the COVID-19 lockdown, with personal COVID-19 exposure being a significant risk factor (27). College students who received a large amount of negative information about COVID-19 may be at a greater risk of psychological maladjustment (28–30). Medical students in China face severe depression and anxiety because of their difficult circumstances, such as the long length of schooling, academic pressure, and the stress of clinical practice (31, 32). Therefore, it is of great importance to pay special attention to the psychological status of medical students and to take appropriate interventions to improve their mental health. In the early stages of this pandemic, medical postgraduate education was disrupted and transformed into prolonged home isolation and online learning. People knew little about the novel coronavirus, leading to increased anxiety and depression symptoms in medical students (33, 34). In the later stages, pandemic prevention and control work has become a norm (35). The present study showed that most of the medical postgraduates had mild anxiety or depression symptoms during the COVID-19 pandemic. None had a severe depression disorder. This indicated that most medical students had strong psychological adjustment abilities and adaptability during the pandemic period, which is consistent with previous studies (18, 36). Another reason for this might be the enhanced prevention and control behaviors of postgraduates. The interdisciplinary faculty similarly launched COVID-19 courses focusing on the pathophysiology, diagnosis and treatment of the infection, the health disparities and ethical considerations associated with the pandemic worldwide (37). During the COVID-19 pandemic, especially in the stage of the normalization of pandemic prevention and control work in China, postgraduates have had a relatively positive attitude, doing a good job of protecting themselves in their clinical practice (38).
According to our findings, females experienced significantly more symptoms on mental health measure scores than males did. Previous studies associating gender and mental health have been inconclusive. In a study by Xie et al. (39) males showed more depressive symptoms. However, some previous studies have reported no significant differences in gender with regard to anxiety and depression. This indicates that male and female students experienced similar stresses and negative emotions as a result of the COVID-19 pandemic (29, 40). Another study showed that depression was more prevalent in female students than male students (41). Moreover, a systemic review found that female students experienced higher levels of anxiety and stress (42). These studies are consistent with ours. A possible explanation is that women are more likely to be affected by the COVID-19 pandemic, displaying higher levels of insomnia, sleep disturbances, anxiety and depression (12) and are more likely to report experiencing higher levels of anxiety (43).
The present study also demonstrated that most postgraduates felt that the COVID-19 pandemic had varying degrees of impact on their academics. After investigating the changes in postgraduate courses during the COVID-19 pandemic, we found that the proportion of offline courses changed to online courses has increased, resulting in a reduction in practical operations and less interaction between teachers and students (Table 4). Several barriers to online learning have contributed to students' overall negative experiences. Clinical skills sessions may occur online. Examinations have also been transitioned to online or, in some cases, may be deferred. Many students have reported concerns about not being able to learn and practice clinical skills in person (44). Moreover, there is a decrease in the number of clinical teachers because some of them have devoted their time to pandemic prevention and control teams (45). These factors may explain postgraduates' concerns about their academic performance. Furthermore, the doctoral postgraduates showed greater academic stress, and they were more worried about not meeting graduation standards than the master's postgraduates. This is consistent with a previous study, which indicated that for more senior students, the academic pressure is greater, and some of them face graduation, employment, and practice, etc., but the epidemic of COVID-19 inevitably affects the development of various things (29). In our study, 68.63% of the postgraduates expressed their willingness to participate in volunteer work. Postgraduates have participated in many ways to care for patients and communities in this crisis.
In the midst of this COVID-19 crisis, it is necessary and important to pay special attention to the psychological status of medical students and take appropriate interventions to improve their mental health. In addition, the COVID-19 pandemic may represent an enduring transformation in medical education. There is uncertainty regarding how long this situation will persist and increasing recognition that there may be periods of recurrence in the future. We need more active curricular innovation and transformation to maintain and improve medical students' academic performance. This may be a seminal moment for many disciplines in medicine.
Our study certainly has limitations. First, the sample size was relatively small, but these participants comprised the vast majority of medical postgraduates at the institution in question during the 2 year COVID-19 pandemic. We will combine multiple medical schools distributed over the province to carry out a large sample survey. Additionally, there were a few related factors affecting the postgraduates' mental health and academic performance in this questionnaire. Our follow-up research should strengthen the investigation of related influencing factors.
Conclusions
Our study found that the COVID-19 pandemic has had a mild impact on the mental health and academic performance of medical postgraduates in China. Females experienced significantly more symptoms on mental health measure scores than males. Moreover, doctoral postgraduates showed greater academic stress, and they were more worried about not meeting graduation standards than master's postgraduates. It is necessary and important to take appropriate interventions to lighten their psychological burdens and improve their academic performance.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The Second Affiliated Hospital, School of Medicine, Zhejiang University. The participants provided their written informed consent to participate in this study.
Author contributions
YY and QT: conceptualization, formal analysis, funding acquisition, writing and preparation of manuscript, and writing original draft. HS, TC, and KY: data curation. YY, YW, and HH: methodology. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Zhejiang Provincial Natural Science Foundation of China [LQ20H120009] and The National Natural Science Foundation [Nos. 82101098, 82070939, and 81971667].
Acknowledgments
We are greatly indebted to all subjects who were enrolled in our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.948710/full#supplementary-material
References
1. International Health Regulations Emergency Committee on novel coronavirus in China. Available online at: https://www.who.int/news-room/events/detail/2020/01/30/default-calendar/international-health-regulations-emergency-committee-on-novel-coronavirus-in-china (accessed May 9, 2022).
2. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-−11-march-2020 (accessed May 9, 2022).
3. WHO, Coronavirus (COVID-19) Dashboard,. WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available online at: https://covid19.who.int/ (accessed May 9, 2022).
4. Dixon LJ, Witcraft SM, Schadegg MJ. COVID-19 anxiety and mental health among university students during the early phases of the U.S. pandemic. J Am Coll Health. (2021) 8:1−9. doi: 10.1080/07448481.2021.1923504
5. Yildirim M, Akgül Ö, Geçer E. The Effect of COVID-19 Anxiety on General Health: the Role of COVID-19 Coping. Int J Ment Health Addiction. (2022) 20:1110–21. doi: 10.1007/s11469-020-00429-3
6. Karadem FB, Demirdaş A, Işik Ü, Kiliç F. Investigation of the psychiatric factors that determine the fear of COVID-19 in healthcare workers and hospital staff in a university hospital in Turkey. J Community Psychol. (2021) 7:1–13. doi: 10.1002/jcop.22657
7. Yildirim M, Arslan G, Özaslan A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: exploring the mediating effects of resilience and coronavirus fear. Int J Ment Health Addiction. (2022) 20:1035–45. doi: 10.1007/s11469-020-00424-8
8. Balakrishnan V, Ng KS, Kaur W, Lee ZL. COVID-19 mental health prevalence and its risk factors in South East Asia. Curr Psychol. (2022) 12:1–16. doi: 10.1007/s12144-021-02556-z
9. Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
10. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. IJERPH. (2020) 17:1729. doi: 10.3390/ijerph17051729
11. Gao J, Zhang P. China's public health policies in response to COVID-19: from an “authoritarian” perspective. Front Public Health. (2021) 9:756677. doi: 10.3389/fpubh.2021.756677
12. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in greece during the COVID-19 pandemic. Front Public Health. (2021) 9:775374. doi: 10.3389/fpubh.2021.775374
13. Hall AK, Nousiainen MT, Campisi P, Dagnone JD, Frank JR, Kroeker KI, et al. Training disrupted: practical tips for supporting competency-based medical education during the COVID-19 pandemic. Med Teach. (2020) 42:756–61. doi: 10.1080/0142159X.2020.1766669
14. Jervis CG, Brown LR. The prospects of sitting ‘end of year' open book exams in the light of COVID-19: a medical student's perspective. Med Teach. (2020) 42:830–1. doi: 10.1080/0142159X.2020.1766668
15. Kapadia SJ. Perspectives of a 2nd-year medical student on ‘students as partners' in higher education – what are the benefits, and how can we manage the power dynamics? Med Teach. (2021) 43:478–9. doi: 10.1080/0142159X.2020.1779922
16. Lee YM, Park KD, Seo J-H. New paradigm of pediatric clinical clerkship during the epidemic of COVID-19. J Korean Med Sci. (2020) 35:e344. doi: 10.3346/jkms.2020.35.e344
17. Rose S. Medical student education in the time of COVID-19. JAMA. (2020) 323:2131–2. doi: 10.1001/jama.2020.5227
18. Xiong P, Ming W, Zhang C, Bai J, Luo C, Cao W, et al. Factors influencing mental health among chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front Public Health. (2021) 9:603331. doi: 10.3389/fpubh.2021.603331
19. Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, et al. Measurement invariance of the patient health questionnaire (PHQ-9) and generalized anxiety disorder scale (GAD-7) across four European countries during the COVID-19 pandemic. BMC Psychiatry. (2022) 22:154. doi: 10.1186/s12888-022-03787-5
20. Mills SD, Fox RS, Malcarne VL, Roesch SC, Champagne BR, Sadler GR. The psychometric properties of the generalized anxiety disorder-7 scale in hispanic Americans with English or Spanish language preference. Cultur Divers Ethnic Minor Psychol. (2014) 20:463–8. doi: 10.1037/a0036523
21. Sun J, Liang K, Chi X, Chen S. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of Chinese adolescents. Healthcare. (2021) 9:1709. doi: 10.3390/healthcare9121709
22. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
23. Zhang Y-L, Liang W, Chen Z-M, Zhang H-M, Zhang J-H, Weng X-Q, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. (2013) 5:268–75. doi: 10.1111/appy.12103
24. Zhang C, Wang T, Zeng P, Zhao M, Zhang G, Zhai S, et al. Reliability, validity, and measurement invariance of the general anxiety disorder scale among Chinese medical university students. Front Psychiatry. (2021) 12:648755. doi: 10.3389/fpsyt.2021.648755
25. Arifagaoglu O, Koseoglu Secgin C, Yuzugullu B. Effect of the COVID-19 pandemic on anxiety in patients with masticatory muscle pain. J Prosthet Dent. (2021) 21:1–6. doi: 10.1016/j.prosdent.2021.09.002
26. Silva Almodovar A, Surve S, Axon DR, Cooper D, Nahata MC. Self-directed engagement with a mobile App (Sinasprite) and its effects on confidence in coping skills, depression, and anxiety: retrospective longitudinal study. JMIR Mhealth Uhealth. (2018) 6:e64. doi: 10.2196/mhealth.9612
27. Ding K, Yang J, Chin M-K, Sullivan L, Demirhan G, Violant-Holz V, et al. Mental health among adults during the COVID-19 pandemic lockdown: a cross-sectional multi-country comparison. IJERPH. (2021) 18:2686. doi: 10.3390/ijerph18052686
28. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
29. Fu W, Yan S, Zong Q, Anderson-Luxford D, Song X, Lv Z, et al. Mental health of college students during the COVID-19 epidemic in China. J Affect Disord. (2021) 280:7–10. doi: 10.1016/j.jad.2020.11.032
30. Lee H, Park SJ, Kim JE, Kong F, Zhao B, Nam H, et al. International comparison of depression during the COVID-19 pandemic among university students in 13 countries: a web-based cross-sectional survey. Asia Pac J Public Health. (2021) 33:928–31. doi: 10.1177/10105395211034062
31. Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X, et al. Systematic review of depression and anxiety in medical students in China. BMC Med Educ. (2019) 19:327. doi: 10.1186/s12909-019-1744-2
32. Xu D-D, Rao W-W, Cao X-L, Wen S-Y, An F-R, Che W-I, et al. Prevalence of depressive symptoms in primary school students in China: a systematic review and meta-analysis. J Affect Disord. (2020) 268:20–7. doi: 10.1016/j.jad.2020.02.034
33. Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. (2020) 8:e10164. doi: 10.7717/peerj.10164
34. Wang J, Liu W, Zhang Y, Xie S, Yang B. Perceived stress among Chinese medical students engaging in online learning in light of COVID-19. Psychol Res Behav Manag. (2021) 14:549–62. doi: 10.2147/PRBM.S308497
35. Tsang HF, Chan LWC, Cho WCS Yu ACS, Yim AKY, Chan AKC, Ng LPW, et al. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther. (2021) 19:877–88. doi: 10.1080/14787210.2021.1863146
36. Liu Z, Liu R, Zhang Y, Zhang R, Liang L, Wang Y, et al. Latent class analysis of depression and anxiety among medical students during COVID-19 epidemic. BMC Psychiatry. (2021) 21:498. doi: 10.1186/s12888-021-03459-w
37. Wayne DB, Green M, Neilson EG. Medical education in the time of COVID-19. Sci Adv. (2020) 6:eabc7110. doi: 10.1126/sciadv.abc7110
38. Feng L, Xie Z, Shen J. Investigation of the cognitive attitudes and behaviors of medical post-graduates in clinical practice during the COVID-19 pandemic in China. Front Public Health. (2021) 9:755163. doi: 10.3389/fpubh.2021.755163
39. Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in china: a survey of medical students. Front Public Health. (2021) 8:588578. doi: 10.3389/fpubh.2020.588578
40. Liu J, Zhu Q, Fan W, Makamure J, Zheng C, Wang J. Online mental health survey in a medical college in china during the COVID-19 outbreak. Front Psychiatry. (2020) 11:459. doi: 10.3389/fpsyt.2020.00459
41. Tareq SR, Likhon RA, Rahman SN, Akter S, Basher MS, Hasan MS, et al. Depression among medical students of Bangladesh. Mymensingh Med J. (2020) 29:16–20.
42. Batra K, Sharma M, Batra R, Singh TP, Schvaneveldt N. Assessing the psychological impact of COVID-19 among college students: an evidence of 15 countries. Healthcare. (2021) 9:222. doi: 10.3390/healthcare9020222
43. Chaplin TM, Hong K, Bergquist K, Sinha R. Gender differences in response to emotional stress: an assessment across subjective, behavioral, and physiological domains and relations to alcohol craving. Alcohol Clin Exp Res. (2008) 32:1242–50. doi: 10.1111/j.1530-0277.2008.00679.x
44. Andersen S, Leon G, Patel D, Lee C, Simanton E. The impact of COVID-19 on academic performance and personal experience among first-year medical students. Med Sci Educ. (2022) 32:389–97. doi: 10.1007/s40670-022-01537-6
Keywords: COVID-19 pandemic, medical postgraduates, mental health, academic performance, education
Citation: Yu Y, Tang Q, Shi H, Chen T, Wang Y, Hu H and Yao K (2022) The impact of the COVID-19 pandemic on the mental health and academic performance of medical postgraduates. Front. Public Health 10:948710. doi: 10.3389/fpubh.2022.948710
Received: 20 May 2022; Accepted: 02 August 2022;
Published: 15 September 2022.
Edited by:
Md Anwarul Azim Majumder, The University of the West Indies, Cave Hill, BarbadosReviewed by:
Rui Liu, Beijing Anding Hospital, Capital Medical University, ChinaVidisha Vallabh, Swami Rama Himalayan University, India
Mohammed Dauda Goni, Universiti Malaysia Kelantan, Malaysia
Copyright © 2022 Yu, Tang, Shi, Chen, Wang, Hu and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiaomei Tang, 11518246@zju.edu.cn
 Yibo Yu
Yibo Yu Qiaomei Tang
Qiaomei Tang Haifei Shi
Haifei Shi Ting Chen
Ting Chen Yaping Wang5
Yaping Wang5 Hanguang Hu
Hanguang Hu