A multi-center, cross-sectional study on the prevalence of facial dermatoses induced by mask use in the general public during the COVID-19 pandemic
Tanreet Kaur1, Simplepreet Kaur 2
2
1Department of Dermatology, Government Medical College, Amritsar, India, 2Consultant dermatologist, Government Multispeciality Hospital sector 16, Chandigarh, India
Corresponding author: Simplepreet Kaur, MD
How to cite this article: Kaur T, Kaur S. A multi.center, cross.sectional study on the prevalence of facial dermatoses induced by mask use in the general public during the COVID-19 pandemic. Our Dermatol Online. 2022;13(1):1-5.
Submission: 11.09.2021; Acceptance: 21.11.2021
DOI: 10.7241/ourd.20221.1
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The use of face masks and coverings has been recommended in public settings to minimize the risk of the transmission of coronavirus. The rampant surge in the use of masks for a prolonged duration has resulted in various facial dermatoses.
Materials and Methods: The present study was an outpatient, multicentric, observational survey conducted over the period of one year. A total of 350 patients were enrolled. A structured questionnaire was employed to collect data identifying adverse skin reactions that had occurred in the area covered by a face mask.
Results: Most of the facial dermatoses were observed in the urban population (78.85%). Maskne was the most common facial dermatosis, detected in 62% of the participants, followed by hypopigmentation (11.42%), hyperpigmentation (8.28%), contact dermatitis (5.42%), non-specific erythema (4.28%), desquamation (3.71%), urticaria (2.57%), and cheilitis (2.28%). The mean duration of mask use was 5.76 hours. A majority of the participants reported maskne in the U zone (both on the cheeks and the chin area) of the face (34%), followed by isolated involvement of the chin (26%), cheeks (20%), mandible region (14%), and bridge of the nose (6%).
Conclusion: The use of face masks for extended hours without adequate precautions causes various cutaneous adverse effects. Thus, it is important to identify the risk factors precipitating mask-related facial dermatoses.
Key words: COVID-19; Maskne; Viral pandemic; Masks
INTRODUCTION
In late 2019, a novel coronavirus emerged in Wuhan, China. Because of its high rate of infectivity, low virulence, and asymptomatic transmission, it has spread rapidly across the geographic boundaries, leading to a pandemic [1]. To curb the widespread infection, the National Center for Disease Control (NCDC) has issued various preventive measures, such as physical and social distancing, quarantining, ventilation of indoor spaces, covering coughs and sneezes, hand washing, and keeping unwashed hands away from the face. The use of face masks or coverings has been recommended in public settings to minimize the risk of transmission [2]. These masks are intended to serve as a mechanical barrier that prevents the spread of virus-laden droplets expelled by the user. The NCDC recommends wearing cloth face coverings, such as homemade face masks, in public settings, where it is difficult to maintain a six-foot distance from other people. Due to their critical supply, surgical masks and N95 respirators are mainly reserved for hospitals and healthcare workers. Surgical masks vary in design, yet the mask itself is often flat and rectangular in shape with pleats or folds. The top of the mask contains a metal strip that may be formed to the shape of the nose. Elastic bands or long, straight ties help to hold the surgical mask in place while wearing it. An N95 respirator is a more tight-fitting face mask. In addition to splashes, sprays, and large droplets, a respirator may also filter out 95% of minute particles such as viruses and bacteria [3]. However, wearing a mask for a prolonged amount of time causes a physiological and psychological burden to the host. Various adverse effects such as headache, maculopapular rash, mask-induced acne (maskne), contact dermatitis, and impaired cognition have been reported in the literature. As we remain amid the pandemic and more waves are predicted to take place in the future, the recognition and management of mask-induced facial dermatoses is imperative for enduring prolonged mask use. Hence, the present study was conducted with the objective to study facial dermatoses induced by mask use in the general public and to provide recommendations for the prevention and treatment of mask-induced facial dermatoses.
MATERIALS AND METHODS
The present study was an outpatient, multicentric, observational survey conducted over the period of one year. A total of 350 patients participated in the study. Patients with a history of facial dermatoses, such as acne, rosacea, or seborrhea, prior to mask use were excluded from the study. Informed consent was obtained from all participants.
A structured questionnaire was employed to collect data identifying adverse skin reactions that had occurred in the area covered by a face mask. The demographic background information included in the questionnaire were age, sex, occupation, Fitzpatrick skin type. The details regarding the possible risk factors predisposing to adverse reactions in the skin covered by a face mask, included types of face masks, the average duration of wearing a face mask in a day, cleaning methods after face mask use, details regarding the use of cosmetic products on the skin underneath the mask, and were addressed in a structured questionnaire.
We employed descriptive statistics to calculate the frequencies and percentages of categorical variables, and means (M) ± standard deviations (SD) for normally distributed continuous variables. Statistical analysis was performed with commercial software (SPSS, version 22.0). To determine the association of maskne with the use of cosmetic products, an odds ratio was calculated, in which the enrolled patients without maskne served as the controls.
RESULTS
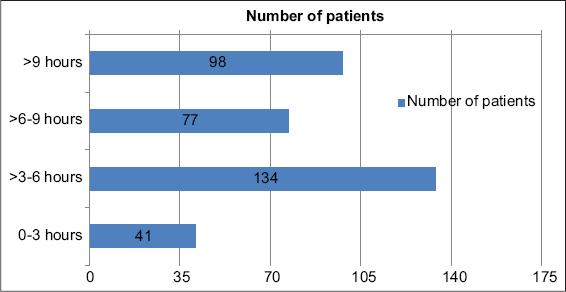
Among the 350 participants with mask-induced facial dermatoses, there were 192 males and 158 females. Their ages ranged from 14 to 76 years (mean: 37.7 ± 11.67 years). Most of the patients had Fitzpatrick skin type IV (54.85%), followed by Fitzpatrick skin type III (25.42%) and V (19.71%) (Table 1). Most of these facial dermatoses were observed in the urban population (78.85%). Maskne was the most common facial dermatosis, detected in 62% of the participants, followed by hypopigmentation (11.42%), hyperpigmentation (8.28%), contact dermatitis (5.42%), non-specific erythema (4.28%), desquamation (3.71%), urticaria (2.57%), and cheilitis (2.28%) (Fig. 1). The mean duration of mask use was 5.76 hours (Fig. 2). A majority of the participants reported maskne in the U zone (both in the cheeks and chin area) of the face (34%), followed by isolated involvement of the chin (26%), cheeks (20%), mandible region (14%), and the bridge of the nose (6%) (Fig. 3). A history of the application of cosmetic products such as foundations, concealers, face powders, etc. was present in 124 (35.42%) patients. The odds ratio of maskne in patients exposed to cosmetics versus those non-exposed was 3.3 (Table 2). The most frequently used type of face mask used was the surgical mask (50.28%), followed by homemade cloth masks (25.71%) and N95 masks (24%).
 |
Table 1: Demographic profile of the study population. |
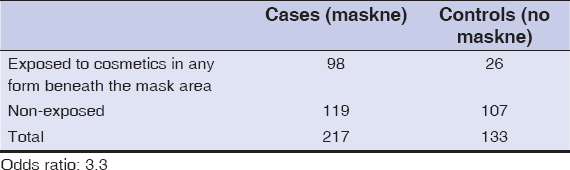 |
Table 2: Correlation coefficient (odd’s ratio) between patients with maskne exposed to cosmetics versus those non-exposed. |
DISCUSSION
During the current coronavirus disease 2019 (COVID-19) epidemic, the concern for halting disease transmission has led to a widespread increase in face mask use. In 2013, a study was conducted in which researchers found that masks led to a more than threefold reduction in how much of the virus was sprayed into the air by an individual [4]. Another study, analyzing data on thousands of Japanese schoolchildren, found that vaccinating and wearing a face mask reduced the likelihood of developing seasonal influenza [5]. However, during this pandemic, we have observed a corresponding increase in adverse effects associated with mask use. A pilot study by Foo et al. discussed adverse skin reactions such as rashes, acne, and itching from mask use in the general public and health care professionals [6]. A New York study conducted among healthcare workers during the COVID-19 pandemic revealed detectable skin damage in 51% and acne in 53% of mask users [7]. Prolonged mask use without adequate breaks causes hyperthermia and an increase in humidity due to the condensation of the exhaled air beneath the mask; this changes the normal skin microflora of the perioral and perinasal areas considerably. Microbiome dysbiosis is implicated in the pathogenesis of maskne, perioral dermatitis, and seborrheic dermatitis [8]. The pressure of a face mask also causes an obstruction in the physiological flow of lymph and blood vessels in the face. In addition, increased mechanical stress and altered skin hydration and pH value of the skin beneath the mask lead to the disruption of the skin barrier rendering it more susceptible to further damage. In an experimental study, the authors were able to prove disturbed barrier function of the skin after only four hours of wearing a mask in twenty healthy volunteers, both with surgical masks and N95 masks [9]. Contact dermatitis, persistent erythema, and urticaria are generally described in connection with hypersensitivities to the ingredients of industrially manufactured masks (surgical masks and N95 masks), such as formaldehyde and thiram (an ingredient in the ear bands). The casual agents for contact urticaria may be fragrances, medications, preservatives, and disinfectants [10]. In the present study, maskne was the most common facial dermatosis, detected in 62% of the participants, followed by hypopigmentation (11.42%), hyperpigmentation (8.28%), contact dermatitis (5.42%), non-specific erythema (4.28%), desquamation (3.71%), urticaria (2.57%), and cheilitis (2.28%) (Figs. 4a – 4d). Similar findings were reported in a study by Ramesh et al., in which maskne was observed in 43% of patients, followed by seborrhea (28%), frictional dermatitis (18%), contact dermatitis (16%), non-specific pruritus (14%), and non-specific erythema (13%) [11]. In a Thai study by Chaiyabutr et al., the most common adverse skin reaction to face mask use was reported to be flareups of previously existing acne [12]. This correlates with our study, in which the most common facial dermatosis was maskne. It is likely a disorder of follicular occlusion and is directly related to mechanical stress (pressure, occlusion, friction) and microbiome dysbiosis (heat, pH, moisture from biofluids). Both of these are affected by increased durations of mask use, as most of the facial dermatoses in the present study were reported in patients wearing masks for more than three hours. Cunliff et al. found that sebum secretion is elevated by 10% as the local temperature increases by 1°C. [13] A Chinese research group reported cutaneous adverse effects such as acne, contact dermatitis, and persistent erythema among 542 participants wearing N95 masks as well as a correlation between the skin damage that occurs and the time of exposure (68.9% in ≤ 6 h/day and 81.7% in > 6 h/day) [14]. The use of cosmetic products beneath a mask further aggravates the situation, as it intensifies the delivery of allergens through an already compromised skin barrier. In the present study, the odds of maskne in patients exposed to cosmetics were higher than in those non-exposed (odds ratio: 3.3, confidence interval: 95%). Pigmentary alteration in the form of hypopigmentation (11.42%) was more common than hyperpigmentation (8.28%) in the mask area. A possible explanation might involve the relatively increased sun exposure of mask-free areas of the face, which causes tanning in these areas. Contact dermatitis due to sensitivity to common allergens such as thiuram, formaldehyde textile resins, etc. results in post-inflammatory hyperpigmentation in mask-covered areas. In our study, contact dermatitis occurred mostly in patients wearing N95 masks, followed by surgical masks. The most common sites involved were the bridge of the nose (45.76%) and the retroauricular area (34.78%). Polyurethanes contained in the sponge strip inside the mask are produced by reaction with diisocyanates, which may cause contact sensitization. Rubber accelerators are employed to accelerate the vulcanization of rubber and have been identified to be allergens in mask elastic bands. Rubber antioxidants, such as N-isopropyl-N’-phenyl-p-phenylenediamine, are also added during the vulcanization process and have been reported in mask-associated contact dermatitis and cheilitis [15]. In a study conducted by Mehak Singh et al. generalized lip dryness was reported in 4% of patients, whereas in the present study, 2.28% of the participants reported cheilitis [16]. In a study by Lan et al. on adverse skin reactions following different types of mask use during the COVID-19 pandemic, erythematous rash was found in mask users. Similarly to the present study, 4.28% of participants reported non-specific erythema on the face [17]. There are reports of the coronavirus leading to vasodilation and telangiectatic vessels in the dermis. Sungnak et al. explained a possible pathway in which SARS.CoV-2 binding to angiotensin-converting enzyme 2 receptors leads to an aberrant elevation in the levels of angiotensin 2 and the activation of endothelial nitric oxide synthase, ensuing persistent vasodilation [18]. As mask use is imperative in the present situation, it is necessary to follow preventive measures to avoid naïve facial dermatoses or the exacerbation of previously existing dermatoses. Recommendations that have been addressed in the literature include frequent work breaks to allow for shorter durations of mask use, an appropriate mask design with a focus on safety, comfort, and tolerability, and general preventative measures such as applying moisturizers, emollients, and barrier creams to maintain a healthy skin barrier. Special consideration for skincare should include the use of gentle antibacterial cleansers, non-comedogenic emollients, hydrogel carrier formulations of retinoid/antibiotic combinations to minimize local irritation, and avoiding the use of occlusive facial makeup under the mask. A better design for face masks would include the omission of abrasive metallic parts that cause nickel sensitization. To prevent mechanical acne measures such as the use of gentle exfoliating cleanser wipes throughout one’s shift, using an ear saver or a headband with buttons to allow ear straps to rest on these instead of behind the ears, and the use of Tegaderm on the bridge of the nose to decrease mechanical stress should be employed.
 |
Figure 4: (a) Mask-induced cheilitis. (b) Mask-induced acne in the U zone. (c)Mask-induced acne in the cheeks. (d) Mask-induced contact dermatitis. |
CONCLUSION
Prolonged mask use for extended hours without adequate precautions causes bacterial optimization under the moist and warm environment beneath the mask, leading to various cutaneous adverse effects. As the third wave of COVID-19 is expected, it is imperative to identify solutions to manage these adverse effects. Frequent breaks, improved hydration, an appropriate skincare regimen, and potentially newly designed comfortable masks are recommendations for the future management of adverse effects related to prolonged mask use.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Sohrabi C, Alsafi Z, O’Neill N, Wo Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency:A review of the 2019 novel coronavirus (COVID-19). Int J Surg Lond Engl. 2020;76:71-6.
2. Teo WL. Diagnostic and management considerations for “maskne“in the era of COVID-19. J Am Acad Dermatol. 2021;84:520-1.
3. Lan J, Song Z, Miao X. Skin damage among healthcare workers managing coronavirus disease (2019). J Am Acad Dermatol. 2020;82:1215-6.
4. Giacalone S, Minuti A, Spigariolo CB, Passoni E, Nazzaro G. Facial dermatoses in the general population due to wearing of personal protective masks during the COVID-19 pandemic:First observations after lockdown. Clin Exp Dermatol. 2021;46:368-9.
5. Wang M-W, Zhou M-Y, Ji G-H, L Ye, Y-R Cheng, Z-H Feng, et al. Mask crisis during the COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:3397-9.
6. Foo CCI, Goon ATJ, Leow Y-H, Goh C-L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome:A descriptive study in Singapore. Contact Dermatitis. 2006;55:291-4.
7. Rosner E. Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. 2000;6:130.
8. Teo WL. The “maskne“microbiome:Pathophysiology and therapeutics. Int J Dermatol. 2021;60:799-809.
9. Tang KM, Chau KH, Kan CW, Fan J. Assessing the accumulated stickiness magnitude from fabric-skin friction:Effect of wetness level of various fabrics. R Soc Open Sci. 2018;5:180860.
10. Singh M, Pawar M, Bothra A. Personal protective equipment induced facial dermatoses in healthcare workers managing Coronavirus disease 2019. J Eur Acad Dermatol Venereol. 2020;34:e378-80.
11. Ramesh A, Thamizhinian K. Clinic epidemiological study of mask induced facial dermatoses due to increased mask usage in general public during COVID-19 pandemic. Int J Res Dermatol. 2021;7:232-8.
12. Chaiyabutr C, Sukakul T, Pruksaeakanan C, Boonchai JTW. Adverse skin reactions following different types of mask usage during the COVID-19 pandemic. J Eur Acad Dermatol Venereol. 2006;55:291-4.
13. Cunliffe WJ, Burton JL, Shuster S. The effect of local temperature variations on the sebum excretion rate. Br J Dermatol. 1970;83:650-4.
14. Choi SY, Hong JY, Kim HJ, Lee GY, Hyun CS, Jung HJ, et al. Mask- induced dermatoses during COVID-19 pandemic:A questionnaire.based study in 12 hospitals of Korea. Clin Exp Dermatol. 2021;3:10.
15. Yu J, Chen JK, Mowad CM, Reeder M, Hylwa S, Chisolm S, et al. Occupational dermatitis to facial personal protective equipment in health care workers:A systematic review. J Am Acad Dermatol. 2021;84:486-94.
16. Singh M, Bothra A, Pawar M, Maheswari A, Tiwari A, Adhicari P. Prevalence of cheilitis in health care workers treating patients with COVID-19. J Am Acad Dermatol. 2020;83:e373-4.
17. Lan J, Song Z, Miao X, Li H, Li Y, Dong L, et al. Skin damage among health care workers managing coronavirus disease (2019). J Am Acad Dermatol. 2020;82:1215-16.
18. Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681-7.
Notes
Source of Support: Nil,
Conflict of Interest: None.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.